Background: Despite the availability of effective vaccines, hepatitis B virus (HBV) infection is still frequent worldwide, and accounts for significant morbidity and mortality. However, data of acute HBeAg negative hepatitis still remain limited. Aims and Methods: To understand clinical pictures of acute HBV hepatitis and its natural evolution, a prospective study was conducted in adult patients. Results: Ninety patients were enrolled between March 2004 and April 2005 at Hospital for Tropical Diseases in Ho Chi Minh city. The prevalence of HBeAg negative was 53%. No significant difference was found in clinical characteristics and laboratory findings between HBeAg positive and negative patients. HBV-DNA was detected in 75% and 88% HBe negative and positive patients, respectively, where the frequency of ALT below 400 U/L was significantly higher in HBeAg negative cases (p = 0.01). Six month follow-up was available in 47 patients. HBsAg positivity was found in 16% of HBeAg negative subjects but only in 4.5% of HBeAg positive cases. Thirty two patients had neither HBsAg nor anti-HBs. Conclusions: The clinical and laboratory feature and the outcome at 6 months of HBV acute hepatitis in Vietnam is similar in HBeAg positive and negative patients.
Abbreviations: HBV: hepatitis B virus; HBeAg: Hepatitis B e antigen; HBsAg: hepatitis B surface antigen; anti-HBs: antibody anti hepatitis B surface antigen; ALT: alanin transferase; γGT: gamma-glutamin drug user; n.s: not significant, SD: standard deviation
IntroductionIn spite of the fact that the strategies of Hepatitis B vaccination are working well globally, hepatitis B virus (HBV) infection is still frequent worldwide. More than 350 million people are chronically infected with this virus,1 of whom 75% are Asian. Although the opened-vaccination program has been widely conducted in Vietnam since 1997, the current chronic HBsAg infection rates among Vietnamese adolescents and adults are still 18.8% and 20.5%, respectively.1,2
The Hospital for Tropical Diseases (HTD) in Ho Chi Minh city, the more advanced center for infectious diseases for the Southern Vietnam, receive about 250-300 adult patients with HBV-related symptomatically acute hepatitis each year. Mortality rate of these patients was approximately 1.4% (unpublished data from HTD, year 2003 and 2004).
By natural evolution or under the pharmacological pressure of the available treatments, hepatitis B virus has gradually changed its molecular structure,2 potentially causing either sub-clinical damage to hepatocytes or becoming resistant to the treatment. Even more, the virus integrates its genetic material into cell and becomes undetectable in sera but still results in severe consequences such as cirrhosis and HCC.4-6 Some kinds of those changes are precore and core promoter mutants presenting the HBeAg negative phenotype.3,6-8
HBeAg, a circulating peptide derived from the core gene, is believed to play a role on the pathogenesis and viral replication. Its interaction with host’s immunity9,10 still remains unclear.11-14 HBeAg negative phenotype was suggested to cause more severe liver damage since it was found in patients with more active liver disease or fulminant hepatitis.15 However, data of clinically acute HBeAg negative hepatitis has still been limited.
The aim of this study was to determine the clinical course and the rate of development to chronic infection in patients admitted to the hospital with the diagnosis of acute HB related hepatitis.
Patients and methodsStudy designThis prospective study was conducted at Hospital for Tropical Diseases in Ho Chi Minh city, Vietnam. Patients were prospectively enrolled from March 1, 2004 to April 30, 2005. All patients were informed of the study and gave written consent to participate.
PatientsPatients older than 15 years, admitted to the hospital with signs and symptoms suggesting acute viral hepatitis, were enrolled in this study. Exclusion criteria were a coexisting chronic disease, also affecting liver functions such as severe malaria, leptospirosis, biliary obstruction, severe sepsis, cancer, exotoxicity, IgM-anti HAV positivity, anti-HCV positivity or HBsAg positivity known from more than 6 months.
Acute hepatitis B was defined by the presence of HBsAg, IgM antibody against HBcAg (anti-HBc IgM) and ALT serum level at least 2 times higher than the upper limit of the normal range within last 6 months.
Clinical protocolSymptoms and signs of acute liver disease were recorded at the admission together with liver function tests (ALT, bilirubin direct and indirect, yGT, ALP, prothrombin time, serum albumin) and blood cell counts. All these biochemical tests were repeated every week for the first month, every 2 weeks for the second month and monthly for a follow-up period of 6 months. HBsAg, IgM anti HBc, HBeAg and anti-HBe (kit tests from Abbott Laboratories, Chicago, Illinois) and HBV-DNA qualitative (measured by PCR assay, Nam Khoa Biotech, Vietnam, cut off value of 50-100 IU/mL) were performed at the time of admission. HBsAg and anti-HBs were repeated at 6 month since the onset (the end of the follow-up period). The presence of HBsAg at 6 months after the enrollment was considered as sign of chronicity of the disease. Acute hepatitis was defined as fulminant in the presence of grade III or IV coma and liver-related extensive coagulopathy developing within 8 weeks from the onset of acute hepatitis.16
Statistical analysisData are expressed as percentage, median [min, max]. The Chi-squared test or Fisher’s exact test for categorical variables, and Student t-test or Mann-Whitney U-test for continuous variables were performed. For all tests, 2 tailed - p values less than 0.05 were considered to be statistically significant. All statistical calculations were performed using SPSS for Windows©, version 11.5 (SPSS Inc., Chicago, IL, USA)
ResultsGeneral characteristicsTable I reports the characteristics of the patients enrolled and the chronological events before admission to, and during the stay in the hospital. Among the 90 patients enrolled, 48 (53.3%) were HBeAg negative while the remaining 42 (46.7%) were HBeAg positive. Age and sex were similarly distributed between the HBeAg negative and positive group. All HBeAg negative patients were anti-HBe positive. Seventy five of 90 patients were admitted to the hospital within the first or the second week from the onset of symptoms, and none was referred to the hospital later than 3 weeks since the first symptoms appeared. In nearly all cases, the possible routes of transmission could not be determined with the exception of four IVDU patients (3 of whom were also HIV positive) and 3 other cases with HBV positive spouses.
General characteristics of patients with HBeAg negative and positive groups.
| All patients N = 90 | HBeAg negative N = 48 | HBeAg positive N = 42 | |
|---|---|---|---|
| Age, median, range* | 27 [16-81] | 27 [16-77] | 26 [16-81] |
| Mean ± SD** | 30 ± 14 | 31 ± 14 | 30 ± 14 |
| 16-30 | 59 (65.6) | 31 (65) | 28 (67) |
| 31-50 | 22 (24.4) | 12 (25) | 10 (24) |
| > 50 | 9 (10) | 5 (10) | 4 (9) |
| Female | 32 (35.6) | 15 (31.3) | 17 (40.5) |
| Admission time from the onset of symptoms | |||
| Week 1 | 41 (45.5) | 22 (45.8) | 19 (45.2) |
| Week 2 | 34 (37.8) | 18 (37.5) | 16 (38.1) |
| Week 3 | 15 (16.7) | 8 (16.7) | 7 (16.7) |
| Possible route of transmission | |||
| Sexual contact to the HBV positive | 3 (3.3) | 1 (2.1) | 2 (4.8) |
| IVDU | 4 (4.4) | 3 (6.3) | 1 (2.4) |
| Unknown | 83 (92.2) | 44 (91.7) | 39 (92.9) |
| Anti-HIV positive | 3 (3.3) | 3 (6.3) | 0 |
The main clinical characteristics of the two groups are presented in Table II There were no significant differences in signs and symptoms between the two groups. Fatigue and appetite loss were the 3 most common symptoms and were present in more that 80% of the cases. All patients, with the exception of one HBeAg positive case, had jaundice.
Signs and symptoms of HBeAg negative and HBeAg positive groups.
| Symptoms and signs, n (%) | All patients N = 90 | HBeAg negative N = 48 | HBeAg positive N = 42 |
|---|---|---|---|
| Fever | 35 (38.9) | 18 (37.5) | 17 (40.5) |
| Fatigue | 80 (88.9) | 44 (91.7) | 36 (85.7) |
| Appetite loss | 74 (82.2) | 41 (85.4) | 33 (78.6) |
| Abdominal discomfort | 30 (33.3) | 15 (31.3) | 15 (37.5) |
| Jaundice | 89 (98.9) | 48 (100) | 41 (97.6)* |
| Nausea | 45 (50) | 26 (54.2) | 19 (45.2) |
| Vomiting | 26 (28.9) | 14 (29.2) | 12 (28.6) |
| Diarrhea | 13 (14.4) | 6 (12.5) | 7 (16.7) |
| Itching | 10 (11.1) | 5 (10.4) | 5 (11.9) |
| Colorless feces | 16 (17.7) | 8 (16.7) | 8 (19) |
| Head, muscle and joint aches | 18 (20) | 8 (16.7) | 10 (23.8) |
| Hepatomegaly | 5 (5.6) | 2 (4.2) | 3 (7.1) |
The comparison of laboratory findings in the two groups is reported in Table III. There were no significant differences in the peak value of yGT and in total bilirubin. The presence of prothrombin time less than 50% of the reference value and albumin content less than 30 g/L were also comparable in the two groups. On the contrary, the median of ALT maximum value in HBeAg negative patients was significantly lower (p = 0.02) than in HBeAg positive cases. The ALT values (approximately 15-20 times the upper normal value) peaked on the first week but decreased quickly on the 2nd week and returned to the normal base line within 4 weeks. At week 2 the difference in ALT value at the admission between HBeAg negative and positive cases disappeared.
Laboratory findings.
| Laboratory findings | All patients N = 90 | HBeAg negative N = 48 | HBeAg positive N = 42 |
|---|---|---|---|
| Maximum ALT level median, mean [95CI] | 624, 9 [532-1483] | 488, 8 [532-1483] | 791, 1 [752-1217]* |
| Maximum γGT level median, mean [95CI] | 119, 1 [42-508] | 126, 1 [128-192] | 117, 1 [114-179] |
| Prothrombin time < 50 %, n (%) | 34 (37) | 22 (45.6) | 12 (28.6) |
| Albumin < 30 g/L, n (%) | 9 (10) | 7 (14.6) | 2 (4.8) |
| HBV-DNA qualitative positive, n (%) | 73 (81) | 36 (75) | 37 (88) |
Although the frequency of HBV-DNA positivity was slightly lower in HBeAg negative than in HBeAg positive patients (75 vs 88%), the difference was not statistically significant. When only HBV-DNA positive cases where considered, the frequence of ALT peak below 400 U/L and of PT below 50% the reference value was significantly higher in HBeAg negative than in HBeAg positive ones (p < 0.01 and p < 0.05, respectively).
Complications and mortalitySix males (6.7%) age ranging from 19 to 76 year, died for causes related to the acute hepatitis. One additional subject died one month after discharge from the hospital for myocardial infarction but he was not considered further in the elaboration. Among the liver-related deaths, three (3.3%) were due to fulminant hepatitis and expired within the first week after hospitalization. These patients were younger (19-27 years old), HBeAg negative, anti HBe positive and HIV co-infected. The remaining 3 died much later (within 6-24 weeks after hospital admission) due to progressive impairment of liver function. Five out of 6 deaths were HBeAg negative.
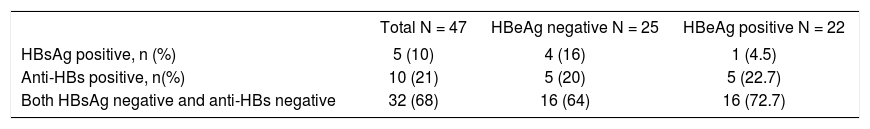
Follow-upTable IV reports data regarding six months follow-up available only in 47 patients (57%) of whom 25 HBeAg negative and 22 HBeAg positive. As indicated above, HIV infected patients were excluded due to early mortality. HBsAg was detected in 4 (16%) HBeAg negative patients but only in one (4.5%) HBeAg positive subject; the difference was not statistically significant. Anti-HBs level (equal or more than 10 mUI/mL) was also equally distributed between the two groups (20% and 23%, respectively). Finally, 32 out of 47 patients had neither HBsAg nor anti-HBs in serum.
DiscussionThis is the first study of acute HBV hepatitis reported on Vietnamese patients and including a sufficiently large sample. The study deals with 90 consecutive patients admitted to the hospital for symptoms (fatigue and loss of appetites) and signs (jaundice) compatible with acute hepatitis. Interestingly they were admitted within three weeks the onset of symptoms, when HBeAg may be still present.17,18 The HBeAg positivity observed at the admission (47%) fell within the range previously reported (32-76%).19,20
Most HBV infection in developed countries results from sexual activity, needle sharing injection-drug use or occupation exposure, while in developing countries infection mainly is related to vertical transmission, although no clear risk factor is found in 20-30% of patients.21 In our study, known risk factors (IVDU or sexual transmission) were found only in 7 cases (8%) in spite of stringent medical recording system.
More than 50% of adult patients with acute hepatitis B is asymptomatic.21-23 All our patients had at least one symptom, the most common being fatigue and appetite loss which were present in more than 80%. More important observation that jaundice, was present in all but one case. Interestingly there was no difference between HBeAg negative and positive patients suggesting that clinically speaking the two groups were fully comparable.
Admittedly we cannot have any figure on the number and clinical course of those patients with acute HBV hepatitis who did not have symptoms and therefore where not admitted to the hospital and then in the study.
The prevalence of serum HBV DNA positivity varies in different series, depending on methods used in detecting HBV DNA.24 In our study HBV-DNA positivity was found in 75% and 88% in HBeAg negative and HbeAg positive cases, respectively, with no difference between the 2 groups. This finding indicates that at the time of testing, the vast majority of our patients had not cleared the virus. In HBV-DNA positive patients, the frequency of ALT level below 400 U/L was significantly higher in HBeAg negative cases. On the contrary, the frequency of PT lower than 50%, suggesting reduction in hepatic protein synthesis, was significantly higher in the HBeAg negative cases. Collectively these findings suggest that in HBeAg negative hepatitis there is an apparent increased impairment in liver function is spite of a lower degree of cellular necrosis.
HBeAg negativity was reported to be more frequent in patients with fulminant hepatic failure compared with those with acute hepatitis.25 In our study, 3.3% patients had fulminant hepatitis, a figure higher than that previously reported Hospital of Tropical Disease (0.1-0.5%)18 and from the annual mortality report of the hospital (1.4%). It is interesting that all of these subjects were HBeAg negative and had HIV co-infection, in line with the demonstration that HIV is one of the known factors to increase the risk of fulminant hepatitis.26,27
After six months the acute episode in more than 55% of the cases a follow up was available HBsAg was detectable in 16% of HBeAg negative but only in 4.5% of positive patients to explain this finding one hypothesis is that HBV virus in Vietnam is changing with pre-core and core-promoter mutations3 although this needs to be addressed in prospective studies. Another possibility we cannot exclude is that at the time of hospital admission, part of our patients already had HBe seroconversion. The third hypothesis is that these patients had a chronic undetected hepatitis which became symptomatic for reacutization. This may be in line with the higher rate of mortality and progression to chronic liver disease observed in these subjects.
Although the percentage of cases available for follow-up claims for caution in conclusion, our study provide information on the natural course o HBV hepatitis in Vietnam. The evidence need to be confirmed in series including a larger number of cases and a follow-up longer that what we reported. It would be also interesting to compare what we observed with data derived from other regions of the world.
AcknowledgmentsDr. Nguyen TYX was supported by a grant from the International Center for Theoretical Physics, Program for Training and Research in Italian Laboratories (TRIL), Trieste, Italy. We are indebt with Dr. Claudio Tiribelli for critical comments and thoughtful review. We also thank Dr. Pham Hoang Phiet, Department of Immunology and Drs. Nguyen Huu Chi, Pham Thi Le Hoa, Dinh The Trung, Vu Thi Thuy Ha, Nguyen Thi Do, Hospital for Tropical Diseases-Hepatitis Department (ward E) for helping in recruiting and follow-up patients. We thank the Laboratory Department for performing liver function test and serum viral markers and Medical Diagnosistic Center (Hoa Hao, Ho Chi Minh city) for HBV-DNA PCR analysis.