Liver disease is characterized by the progression from hepatitis to cirrhosis, followed by liver cancer, i.e., a disease with a higher mortality rate as the disease progresses. To estimate the cost of illness (COI) of liver diseases, including viral hepatitis, cirrhosis, and liver cancer, and to determine the overall effect of expensive but effective direct-acting antivirals on the COI of liver diseases.
Patients or materials and methodsUsing a COI method from available government statistics data, we estimated the economic burden at 3-year intervals from 2002 to 2017.
ResultsThe total COI of liver diseases was 1402 billion JPY in 2017. The COI of viral hepatitis, cirrhosis, and liver cancer showed a downward trend. Conversely, other liver diseases, including alcoholic liver disease and nonalcoholic steatohepatitis (NASH), showed an upward trend. The COI of hepatitis C continued to decline despite a sharp increase in drug unit prices between 2014 and 2017.
ConclusionsThe COI of liver diseases in Japan has been decreasing for the past 15 years. In the future, a further reduction in patients with hepatitis C is expected, and even if the incidence of NASH and alcoholic liver disease increases, that of cirrhosis and liver cancer will likely continue to decrease.
Liver diseases, including viral hepatitis and primary malignant neoplasm of the liver and intrahepatic bile ducts (ICD-10 code: B15–B19, C22, and K70–K77), caused 47,875 deaths in 2017, which comprised approximately 3.6% of all deaths in Japan [1]. Liver disease is characterized by the progression from hepatitis to cirrhosis, followed by liver cancer; i.e., disease with a higher mortality rate as the disease progresses. In recent years, the incidence of viral hepatitis has been decreasing owing to the development of viral hepatitis vaccines, screening, and prevention of mother-to-child transmission; thus, overall liver diseases have been also decreasing. Moreover, direct-acting antivirals (DAAs), which have become available in recent years, are expected to further reduce the prevalence of hepatitis C virus (HCV) [2–4]. The death toll from liver disease among all deaths in 1997 was 5.9%, with a decrease of 2.6% over the last 20 years [1]. However, morbidity and mortality from nonalcoholic fatty liver disease and nonalcoholic steatohepatitis (NASH) are increasing, suggesting that the composition of liver diseases has greatly changed [5–7].
Considering that liver diseases have characteristics such that the disease transitions in the long term, it is desirable to observe long-term changes for each related diseases with respect to social costs. Previous studies have calculated the costs for hepatitis B (HBV), HCV, and related diseases (cirrhosis and liver cancer) [8–12]. There are time-series studies on social costs, including indirect costs in the United States [13,14], Korea [15,16], and Spain [17].
However, there are few studies on the social costs of liver disease in Japan. In Japan, approximately 80% of liver cancers have been demonstrated to be caused by HBV and HCV [18], with those caused by HCV being predominant [19,20]. Regarding HBV, in 1986, the Japanese government initiated a nationwide HBV screening and immunization program for infants born to mothers carrying HBV. Since the 1986 birth cohort, the number of HBV carriers has decreased remarkably. As for carriers of HCV, a first-generation HCV antibody test was introduced as early as 1990 for screening blood for blood transfusions; in 1999, a nucleic acid amplification test was also introduced [21]. Furthermore, DAAs are covered and reimbursed by public medical insurance, which has continuously reduced the social cost of liver disease as a whole.
The authors have reported the social costs of cirrhosis and hepatocellular carcinoma (HCC) [22,23]. The cost of illness (COI) for HCC was 579.2 billion JPY as of 2014, a 29.0% decrease compared with 1996; the COI for cirrhosis was 208.1 billion JPY, a decrease of 53.1% since 1996; and the mortality cost for both diseases accounted for the largest part of the COI, approximately 70%–80%. However, these two estimations are based on aggregated statistical data published by the government, and it is not possible to classify liver diseases in greater detail. The limitations included round-off errors and rough estimates.
In this study, therefore, social costs were estimated using the COI method for various liver diseases, including viral hepatitis, cirrhosis, and liver cancer, using individual statistical data from the government. The purpose of this study was to clarify how each cost has changed.
Materials and methodsMaterialsAll estimates were based on government statistics. Estimations include data on health-related indicators and economic data such as labor value lost from the disease. For the former data, “vital statistics” were used to estimate the number of deaths, and a “patient survey” was used to estimate the number of discharges, the number of outpatients, and the average length of hospital stay. Vital statistics is an exhaustive survey conducted annually by the government, and the published data are also tabulated by sex and age. The patient survey is a sample survey conducted by the government once every 3 years for patients in hospitals and clinics. It covers 70%–80% of all hospitals in Japan and 6%–7% of clinics. The sample size was approximately 2 million outpatients and 0.8–1.1 million discharged patients; the published summary table is only a rough figure. In this study, individual data, which are necessary to apply to the Statistics Bureau of the Ministry of Internal Affairs and Communications, were obtained and aggregated to tabulate a more detailed disease classification than the published tabulated data. In addition, data on medical expenses by disease were obtained from the Survey of National Medical Care Insurance Services [24].
Regarding the aggregation of economic data, the Basic Survey on Wage Structure [25] was used for wages, and the Employment Status Survey [26] was used for employment rates. Furthermore, for unpaid work such as housework, we used a series of estimation results determined by the Cabinet Office on the monetary evaluation of unpaid work [27].
MethodsThe COI method, developed by Rice et al., converts the social burden of disease into a monetary value, and is widely used because it can easily evaluate the social cost of disease [28–34]. There are 2 types of COI estimation: the top-down method, which calculates the national COI using national data; and the bottom-up method, which is accumulated from the results of individual surveys. The top-down method was used in this study. Additionally, there are 2 estimation methods: one based on prevalence and the other based on incidence. In this study, the estimation was performed on a yearly basis based on incidence. The target diseases are (1) HBV (ICD-10 code: B16, B17.0, B18.0, B18.1); (2) HCV (ICD-10 code: B17. 1, B18.2); (3) other viral hepatitis (ICD-10 code: the rest of B15–B19); (4) malignant neoplasm of the liver and intrahepatic bile ducts (ICD-10 code: C22); (5) nonalcoholic cirrhosis (ICD-10 code: K74.3–K74.6); and (6) other liver diseases (ICD-10 code: the rest of K70–K76).
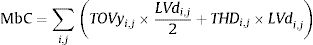
We evaluated 3 COI components: direct cost (DC), morbidity cost (MbC), and mortality cost (MtC). The total cost can be defined as follows:
The direct costs are the medical expenses used for the medical treatment of the disease. In Japan, almost all medical practices are covered and reimbursed by public medical insurance; thus, the cost can be calculated directly by combining the payment of medical insurance and the self-payment. Specifically, using the Survey of National Medical Care Insurance Services, we calculated the direct cost, summing the cost of public medical insurance paid for inpatient services, that for outpatient services (both including drug costs), and self-payment. Viral hepatitis is not subdivided in the Survey of National Medical Care Insurance Services. Therefore, viral hepatitis was classified into HBV, HCV, and other viruses, and it was assumed that there was no difference in average unit price per hospital day and outpatient until 2014. Then, the proportion of the three viral diseases in total hospital days and outpatient visits calculated from the individual patient survey questionnaire was calculated, and the direct cost of viral hepatitis was prorated. Since approximately 2015, expensive DAAs, such as sofosbuvir, have been introduced for treatment of HCV. During this time, however, no expensive treatment was introduced for hepatitis caused by HBV and other viruses. Therefore, for 2017, the direct cost of hepatitis caused by HBV and other viruses was calculated, assuming that the increase of the average unit price per visit was equivalent to the average growth rate from 1996 to 2014. The direct cost of HCV was calculated as a residual.
The morbidity cost is the labor value lost by hospitalization or hospital visits. In this study, the opportunity cost method was used for the calculation. The morbidity cost can be expressed by the following formula:
TOVy:the total number of hospital visits for the disease;LVd:labor value per day;
THD:total length of hospital stay due to the disease.
Specifically, the total number of outpatients and the total length of stay classified by disease, sex, and age group were tabulated from the individual patient survey data. Labor value per day was classified by sex, and age group was calculated from the Basic Survey on Wage Structure, the Employment Status Survey, and estimation results determined by the Cabinet Office on monetary evaluation of unpaid work. We calculated the morbidity cost by multiplying these.
Mortality costs are social losses due to death from the disease. In this study, we calculated them using the human capital method, which is a method of calculating the value of a person as capital using current and future labor values. The age of death is specified, and the amount of labor value that can be produced if he/she survives to the average age is calculated as the present value of total future income. Thus, mortality costs can be defined as follows:
NDy:the number of deaths by disease;LVl:lifetime labor value of the deceased individual;
in which
LVy:1-year labor value; r:discount rateThe discount rate was set to 2% because Japanese economic evaluation guidelines recommend 2% [35].
For chronic and disabling diseases, such as cerebrovascular diseases, long-term care costs should be included in COI. In our previous study, the long-term care costs for malignant neoplasms had been estimated to be approximately 3% of the total [36]. For liver diseases, the long-term care costs are considered small and were not included in the present study.
The protocol of this study was reviewed by the Ethical Committee of Toho University School of Medicine, and the committee confirmed that no approval is necessary for this kind of study in Japan because of the anonymous nature of the data (reference number A19034).
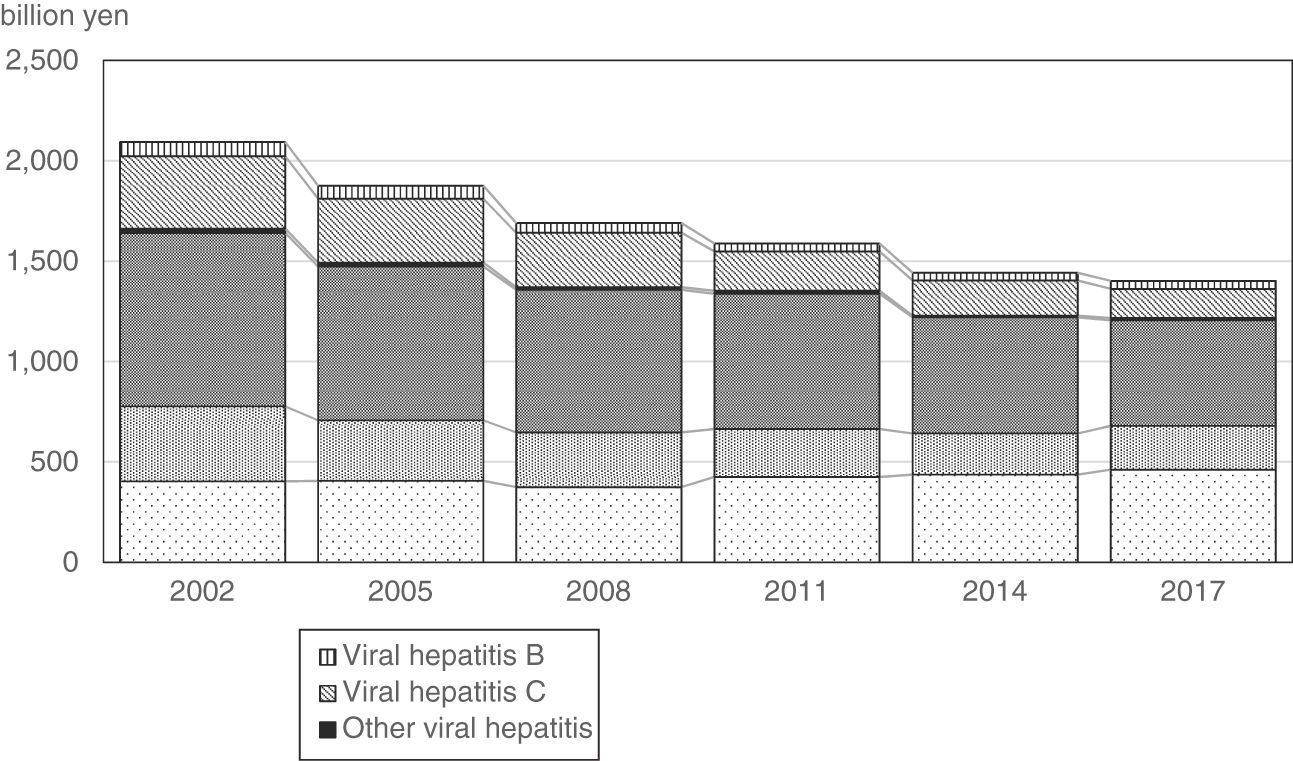
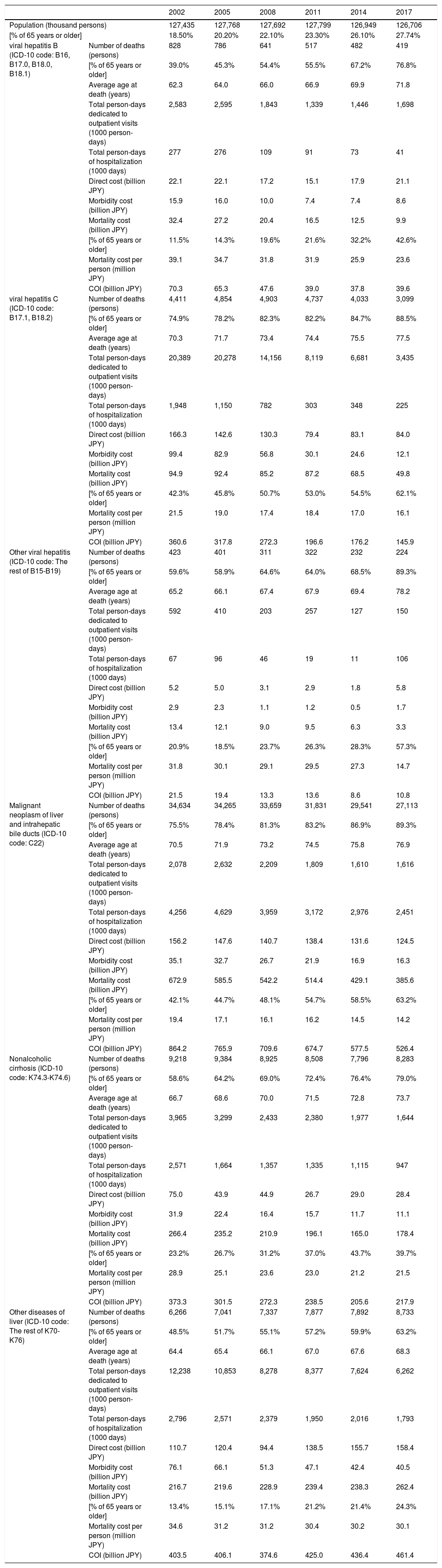
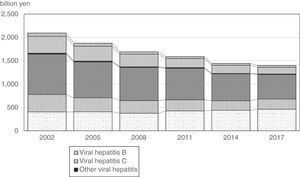
ResultsFig. 1 shows changes in COI by disease, and Table 1 shows the changes in COI and related indicators. The total COI of liver diseases was 1402 billion JPY in 2017. The breakdown is 39.6 billion JPY for HBV; 145.9 billion JPY for HCV; 10.8 billion JPY for other viral hepatitis; 526.4 billion JPY for malignant neoplasm of the liver and intrahepatic bile ducts; 217.9 billion JPY for nonalcoholic cirrhosis; and 461.4 billion JPY for other diseases of the liver. In terms of time series, in the 15 years since 2002, the COI of liver disease decreased by 33.0%, giving an annual average change (APC) of −2.8%. The largest reduction was in HCV, a decrease of 59.5% over 15 years, with an APC of −6.3%. Conversely, other liver diseases, including alcoholic liver disease and NASH, increased by 14.3%, with an APC of 1.0%.
The time trend of cost of illness (COI) of liver diseases.
| 2002 | 2005 | 2008 | 2011 | 2014 | 2017 | ||
|---|---|---|---|---|---|---|---|
| Population (thousand persons) | 127,435 | 127,768 | 127,692 | 127,799 | 126,949 | 126,706 | |
| [% of 65 years or older] | 18.50% | 20.20% | 22.10% | 23.30% | 26.10% | 27.74% | |
| viral hepatitis B (ICD-10 code: B16, B17.0, B18.0, B18.1) | Number of deaths (persons) | 828 | 786 | 641 | 517 | 482 | 419 |
| [% of 65 years or older] | 39.0% | 45.3% | 54.4% | 55.5% | 67.2% | 76.8% | |
| Average age at death (years) | 62.3 | 64.0 | 66.0 | 66.9 | 69.9 | 71.8 | |
| Total person-days dedicated to outpatient visits (1000 person-days) | 2,583 | 2,595 | 1,843 | 1,339 | 1,446 | 1,698 | |
| Total person-days of hospitalization (1000 days) | 277 | 276 | 109 | 91 | 73 | 41 | |
| Direct cost (billion JPY) | 22.1 | 22.1 | 17.2 | 15.1 | 17.9 | 21.1 | |
| Morbidity cost (billion JPY) | 15.9 | 16.0 | 10.0 | 7.4 | 7.4 | 8.6 | |
| Mortality cost (billion JPY) | 32.4 | 27.2 | 20.4 | 16.5 | 12.5 | 9.9 | |
| [% of 65 years or older] | 11.5% | 14.3% | 19.6% | 21.6% | 32.2% | 42.6% | |
| Mortality cost per person (million JPY) | 39.1 | 34.7 | 31.8 | 31.9 | 25.9 | 23.6 | |
| COI (billion JPY) | 70.3 | 65.3 | 47.6 | 39.0 | 37.8 | 39.6 | |
| viral hepatitis C (ICD-10 code: B17.1, B18.2) | Number of deaths (persons) | 4,411 | 4,854 | 4,903 | 4,737 | 4,033 | 3,099 |
| [% of 65 years or older] | 74.9% | 78.2% | 82.3% | 82.2% | 84.7% | 88.5% | |
| Average age at death (years) | 70.3 | 71.7 | 73.4 | 74.4 | 75.5 | 77.5 | |
| Total person-days dedicated to outpatient visits (1000 person-days) | 20,389 | 20,278 | 14,156 | 8,119 | 6,681 | 3,435 | |
| Total person-days of hospitalization (1000 days) | 1,948 | 1,150 | 782 | 303 | 348 | 225 | |
| Direct cost (billion JPY) | 166.3 | 142.6 | 130.3 | 79.4 | 83.1 | 84.0 | |
| Morbidity cost (billion JPY) | 99.4 | 82.9 | 56.8 | 30.1 | 24.6 | 12.1 | |
| Mortality cost (billion JPY) | 94.9 | 92.4 | 85.2 | 87.2 | 68.5 | 49.8 | |
| [% of 65 years or older] | 42.3% | 45.8% | 50.7% | 53.0% | 54.5% | 62.1% | |
| Mortality cost per person (million JPY) | 21.5 | 19.0 | 17.4 | 18.4 | 17.0 | 16.1 | |
| COI (billion JPY) | 360.6 | 317.8 | 272.3 | 196.6 | 176.2 | 145.9 | |
| Other viral hepatitis (ICD-10 code: The rest of B15-B19) | Number of deaths (persons) | 423 | 401 | 311 | 322 | 232 | 224 |
| [% of 65 years or older] | 59.6% | 58.9% | 64.6% | 64.0% | 68.5% | 89.3% | |
| Average age at death (years) | 65.2 | 66.1 | 67.4 | 67.9 | 69.4 | 78.2 | |
| Total person-days dedicated to outpatient visits (1000 person-days) | 592 | 410 | 203 | 257 | 127 | 150 | |
| Total person-days of hospitalization (1000 days) | 67 | 96 | 46 | 19 | 11 | 106 | |
| Direct cost (billion JPY) | 5.2 | 5.0 | 3.1 | 2.9 | 1.8 | 5.8 | |
| Morbidity cost (billion JPY) | 2.9 | 2.3 | 1.1 | 1.2 | 0.5 | 1.7 | |
| Mortality cost (billion JPY) | 13.4 | 12.1 | 9.0 | 9.5 | 6.3 | 3.3 | |
| [% of 65 years or older] | 20.9% | 18.5% | 23.7% | 26.3% | 28.3% | 57.3% | |
| Mortality cost per person (million JPY) | 31.8 | 30.1 | 29.1 | 29.5 | 27.3 | 14.7 | |
| COI (billion JPY) | 21.5 | 19.4 | 13.3 | 13.6 | 8.6 | 10.8 | |
| Malignant neoplasm of liver and intrahepatic bile ducts (ICD-10 code: C22) | Number of deaths (persons) | 34,634 | 34,265 | 33,659 | 31,831 | 29,541 | 27,113 |
| [% of 65 years or older] | 75.5% | 78.4% | 81.3% | 83.2% | 86.9% | 89.3% | |
| Average age at death (years) | 70.5 | 71.9 | 73.2 | 74.5 | 75.8 | 76.9 | |
| Total person-days dedicated to outpatient visits (1000 person-days) | 2,078 | 2,632 | 2,209 | 1,809 | 1,610 | 1,616 | |
| Total person-days of hospitalization (1000 days) | 4,256 | 4,629 | 3,959 | 3,172 | 2,976 | 2,451 | |
| Direct cost (billion JPY) | 156.2 | 147.6 | 140.7 | 138.4 | 131.6 | 124.5 | |
| Morbidity cost (billion JPY) | 35.1 | 32.7 | 26.7 | 21.9 | 16.9 | 16.3 | |
| Mortality cost (billion JPY) | 672.9 | 585.5 | 542.2 | 514.4 | 429.1 | 385.6 | |
| [% of 65 years or older] | 42.1% | 44.7% | 48.1% | 54.7% | 58.5% | 63.2% | |
| Mortality cost per person (million JPY) | 19.4 | 17.1 | 16.1 | 16.2 | 14.5 | 14.2 | |
| COI (billion JPY) | 864.2 | 765.9 | 709.6 | 674.7 | 577.5 | 526.4 | |
| Nonalcoholic cirrhosis (ICD-10 code: K74.3-K74.6) | Number of deaths (persons) | 9,218 | 9,384 | 8,925 | 8,508 | 7,796 | 8,283 |
| [% of 65 years or older] | 58.6% | 64.2% | 69.0% | 72.4% | 76.4% | 79.0% | |
| Average age at death (years) | 66.7 | 68.6 | 70.0 | 71.5 | 72.8 | 73.7 | |
| Total person-days dedicated to outpatient visits (1000 person-days) | 3,965 | 3,299 | 2,433 | 2,380 | 1,977 | 1,644 | |
| Total person-days of hospitalization (1000 days) | 2,571 | 1,664 | 1,357 | 1,335 | 1,115 | 947 | |
| Direct cost (billion JPY) | 75.0 | 43.9 | 44.9 | 26.7 | 29.0 | 28.4 | |
| Morbidity cost (billion JPY) | 31.9 | 22.4 | 16.4 | 15.7 | 11.7 | 11.1 | |
| Mortality cost (billion JPY) | 266.4 | 235.2 | 210.9 | 196.1 | 165.0 | 178.4 | |
| [% of 65 years or older] | 23.2% | 26.7% | 31.2% | 37.0% | 43.7% | 39.7% | |
| Mortality cost per person (million JPY) | 28.9 | 25.1 | 23.6 | 23.0 | 21.2 | 21.5 | |
| COI (billion JPY) | 373.3 | 301.5 | 272.3 | 238.5 | 205.6 | 217.9 | |
| Other diseases of liver (ICD-10 code: The rest of K70-K76) | Number of deaths (persons) | 6,266 | 7,041 | 7,337 | 7,877 | 7,892 | 8,733 |
| [% of 65 years or older] | 48.5% | 51.7% | 55.1% | 57.2% | 59.9% | 63.2% | |
| Average age at death (years) | 64.4 | 65.4 | 66.1 | 67.0 | 67.6 | 68.3 | |
| Total person-days dedicated to outpatient visits (1000 person-days) | 12,238 | 10,853 | 8,278 | 8,377 | 7,624 | 6,262 | |
| Total person-days of hospitalization (1000 days) | 2,796 | 2,571 | 2,379 | 1,950 | 2,016 | 1,793 | |
| Direct cost (billion JPY) | 110.7 | 120.4 | 94.4 | 138.5 | 155.7 | 158.4 | |
| Morbidity cost (billion JPY) | 76.1 | 66.1 | 51.3 | 47.1 | 42.4 | 40.5 | |
| Mortality cost (billion JPY) | 216.7 | 219.6 | 228.9 | 239.4 | 238.3 | 262.4 | |
| [% of 65 years or older] | 13.4% | 15.1% | 17.1% | 21.2% | 21.4% | 24.3% | |
| Mortality cost per person (million JPY) | 34.6 | 31.2 | 31.2 | 30.4 | 30.2 | 30.1 | |
| COI (billion JPY) | 403.5 | 406.1 | 374.6 | 425.0 | 436.4 | 461.4 | |
Abbreviations: COI, cost of illness; JPY, Japanese yen.
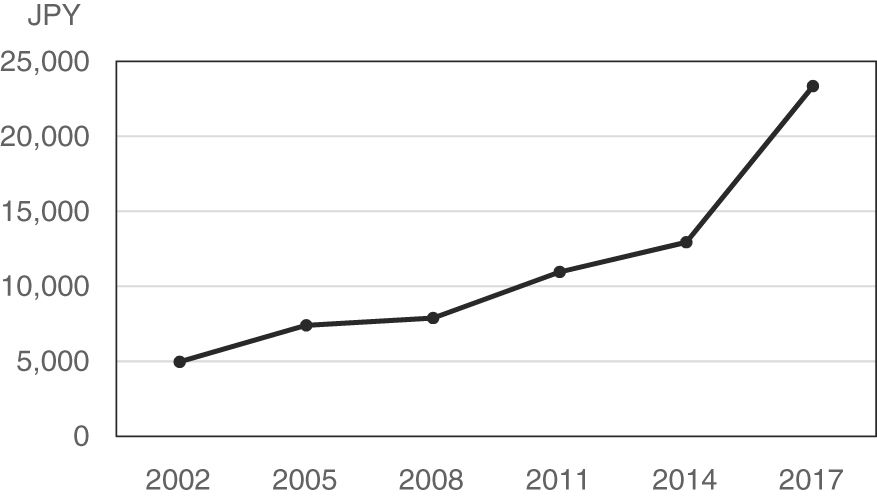
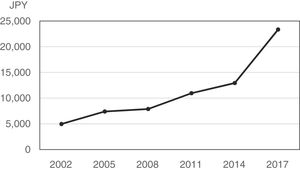
In terms of the 2017 COI composition, viral hepatitis generally has a high direct cost proportion (53.4% for HBV, 57.6% for HCV, and 53.8% for other hepatitis). In 2002, however, the proportion of direct costs was 31.4% for HBV, 46.1% for HCV, and 24.1% for other hepatitis, indicating that the proportions have increased over the past 15 years. This is because the relative proportion of direct costs has increased due to the reduced cost of morbidity and mortality, rather than the direct cost alone. The number of HBV deaths decreased by approximately 49.4%, the total number of hospital visits decreased by 34.3%, and the total length of hospital stay decreased by 85.2%; the number of HCV deaths decreased by approximately 29.7%, the total number of hospital visits decreased by 83.2%, and the total length of hospital stay decreased by 88.4%. These changes have contributed to lowering morbidity and mortality costs, and have also contributed to the suppression of direct cost increases by countering continuous increases in drug unit prices. In particular, HCV showed a significant increase in unit cost of outpatient treatment per day in 2017; however, the total direct cost increased only by 1.1% from 2014.
On the other hand, mortality costs from liver cancer and cirrhosis account for more than 70% of COI, and this proportion has not changed for 15 years. Over the past 15 years, direct costs, morbidity costs, and mortality costs have all declined significantly. For liver cancer and cirrhosis, respectively, the number of outpatients decreased by 22.2% and 58.5%, and the total number of hospital stays decreased by 42.4% and 63.2%.
Against this trend, mortality costs from other liver diseases, the only diseases for which the COI has risen over the past 15 years, accounted for more than 50% of COI and have increased by 21.1% over the past 15 years. This change is thought to be due to a 39.4% increase in the number of deaths. On the other hand, the total number of hospital visits and the total length of hospital stay have been decreasing, as well as direct costs and morbidity costs. Breaking down the number of deaths into more detailed categories, the number of deaths from alcoholic liver disease has risen to 55.1%, and accounted for 74.4% of the increase in COI of other liver diseases.
For all liver diseases, the mortality cost per person has been declining. The decline appears to be related to an increase in the average age of death and the proportion of deaths 65 years or over by all diseases. In particular, the age of death was high, and the most significant increase in the last 15 years was for other viral hepatitis; the mortality cost per death decreased by 53.9%.
In recent years, with the advent of DAAs that are effective but expensive, treatment methods and results for patients with HCV have changed significantly. Particularly since the approval of sofosbuvir in 2015, patients who had been hospitalized and required interferon or peg-interferon administration are now being prescribed outpatient oral DAAs, resulting in an increase in outpatient unit price. Fig. 2 shows the trend for the outpatient unit price from viral hepatitis, which increased rapidly from 2014 to 2017.
DiscussionThe COI of liver disease between 2002 and 2017 has generally decreased except for other liver diseases, including alcoholic liver disease and NASH. In particular, the COI of viral hepatitis has declined significantly, with HCV being reduced to less than half that of 2002. A reduction in the total number of hospital visits and total length of hospital stay, as well as a reduction in the number of deaths, contributed to the reduced COI. In addition, the increase in the average age of death led to a decline in the labor value per person (low human capital value per death), also contributing to the reduced COI. Only other liver disease COIs have risen over the last 15 years, and the increase in mortality cost has led to an increase in COI, especially due to more deaths from alcoholic liver disease. Previous studies have reported that the incidence and mortality of NASH has increased [5–7]; however, NASH itself is unlikely to cause death.
Liver disease has been shown to progress from hepatitis to cirrhosis, and further to liver cancer; thus, a reduction in hepatitis would eventually lead to reduced cirrhosis and liver cancer. In Japan, liver cancer derived from viral hepatitis, especially HCV, has been dominant. Early prevention of infection from blood and blood products during blood transfusions would reduce the number of new patients with hepatitis C over the long term, and the number of those healed by the emergence of effective DAAs is expected to increase. In the future, the COI of liver cirrhosis and liver cancer is expected to decrease further.
Compared with previous studies on the social burden of liver disease in other countries, the cost of social illness for each liver disease in the United States has tended to increase [13,14]. In South Korea, it has been reported that the COI increased until approximately 2013 for liver cancer; in recent years, however, there is a decreasing trend, and liver disease as a whole is also decreasing [15,16]. On the other hand, a study in Spain showed that disease costs for HCV-derived liver disease had already been declining between 2007 and 2011 [17]. In Japan, the social burden of liver disease started decreasing rapidly earlier than in these countries. In Japan, the proportion of alcoholic hepatitis and cirrhosis and liver cancer derived from NASH is still small compared with Western countries. Even if the number of deaths due to these diseases has increased, it is offset by a reduction in the number of deaths due to viral hepatitis, and the overall number of deaths due to liver diseases has not yet been significantly affected.
Our research has limitations. One is that the direct cost of viral hepatitis has not been subdivided; thus, it was necessary to perform calculations using estimated values. The direct cost is divided into the HBV, HCV, and other viral hepatitis, using the number of total hospital visits and the total length of hospital stay. Despite the rapid increase in the unit cost of treatment since 2015, it was assumed that unit prices of type B and other viral hepatitis would have increased as occurred in the past. In addition, we made a strong assumption that all unit prices that were higher than the trend between 2014 and 2017 were due to an increase in the unit cost of direct costs for HCV. In fact, the emergence of sofosbuvir for HCV treatment between 2014 and 2017 caused dramatic changes in the treatment unit price and treatment results; however, new treatment for HBV and other types of viral hepatitis was only tenofovir, and the unit price is not high. Even assuming that the off-trend price increases are all due to HCV treatment, the HCV COI has shown a significant reduction, and the decreasing trend of viral hepatitis has not changed. Second, this study does not include future COI trends. Rather, it is limited to creating basic data for simulating future COIs using models such as Markov models and system dynamics. These estimates will be the subject of our next study.
ConclusionFor liver diseases in Japan, the COIs of viral hepatitis, cirrhosis, and liver cancer have been decreasing for the past 15 years. In the future, a further reduction in patients with HCV is expected, and even if rates of NASH and alcoholic liver disease increase, cirrhosis and liver cancer will likely continue to decrease.
Conflict of interestThe authors have no conflict of interest to declare.
FundingThis study was supported in part by the Japan Society for the Promotion of Science KAKENHI Grant No. 18K09955.
None.