Cutaneous amyloidosis is a rare disease characterized by the deposition of amyloid in the dermis. It can be primary or secondary, depending on associated diseases. It has been linked to various autoimmune diseases, including primary biliary cirrhosis. We present the case of a patient with an autoimmune hepatitis-primary biliary cirrhosis overlap syndrome with concomitant cutaneous amyloidosis, a very unusual association, and discuss similar cases and possible pathophysiological implications.
Amyloidosis can be classified as either systemic or cutaneous, with both primary and secondary forms. Histopathologic evidence of extracellular deposition of amyloid protein (apple-green birefringence in Congo red stained slides under polarized light) within the dermis is the prominent characteristic of cutaneous amyloidoses.1,2 Autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC) are the three main variants of autoimmune liver disease, and when patients present with clinical, biochemical or histopathological features of more that one of these entities, they are called overlap syndromes.3,4 We present a case of a patient showing AIH-PBC overlap syndrome and simultaneous primary localized cutaneous amyloidosis (PLCA), an extremely rare association.
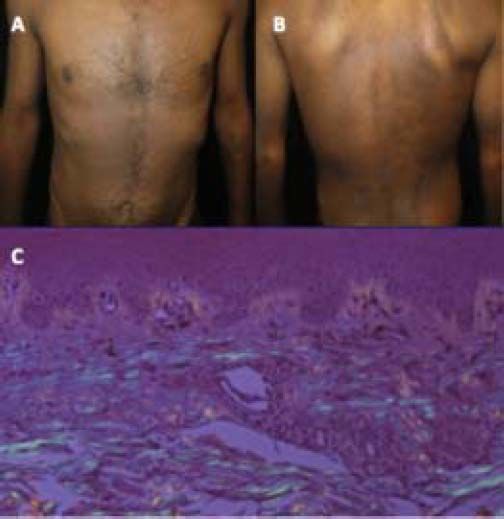
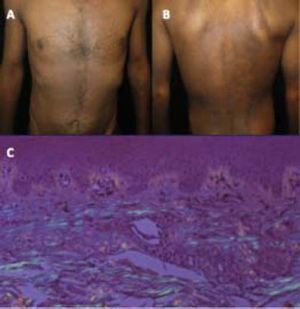
Case ReportA 36-years-old male patient presents with pruritic papules with brownish pigmentation of his arms for 5 months. The patient also referred 3 months with icteric jaundice, acholia and choluria. During this period, the patient reported no fever, use of medications or blood transfusions. On physical examination there were several hyperpigmented papules super imposed upon macular areas over extensor surfaces of arms and legs, also hyperpigmented macules with a rippled appearance on upper chest and upper back (Figures 1A and 1B). A painless liver with a thick edge 1 cm below the right costal margin was noted. No evidence of chronic liver disease.
Laboratory exams revealed:
- •
Total bilirubin = 6.2 mg/dL (normal value: 1.0 mg/dL).
- •
Direct bilirubin = 3.4 mg/dL (0.4 mg/dl).
- •
Gamma-glutamyltransferase = 849 U/l (30 U/l), and
- •
Alkaline phosphatase = 767 U/l (250 U/l).
- •
Alanine aminotransferase = 254 U/I (48 U/I) and
- •
Aspartate aminotransferase = 231 U/I (49U/I).
Serology for hepatitis A, B and C was negative, and the iron store profile was normal. Ultrasound of the liver only showed a homogeneous liver in the absence of biliary lithiasis or dilatation of the bile ducts.
Skin biopsy with Congo red staining revealed an apple-green birefringence under polarized light (Figure 1C). These lesions were diagnosed as the macular form of PLCA.
Determination of serum anti-mitochondrial antibody (AMA) and anti-smooth muscle antibody (ASMA) was positive (1:320).
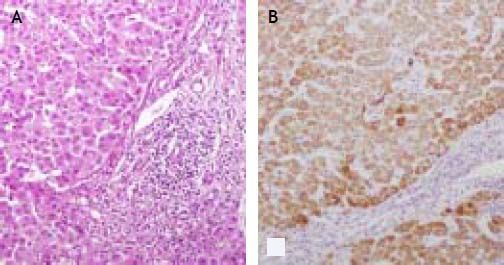
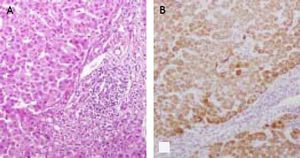
The patient was submitted to a percutaneous liver biopsy to rule out hepatic involvement with deposition of amyloid material. The liver biopsy showed non-suppurative destructive cholangitis with ductopenia with interface hepatitis and the absence of an amyloid deposit after staining with Congo red (Figures 2A and 2B).
The patient was treated with a combination of ursodeoxycholic and prednisone. Unfortunately, there the patient did no show to the follow-up visits.
DiscussionPrimary localized cutaneous amyloidosis (PLCA) consists of the deposition of amyloid in previously healthy skin with no systemic involvement, and is usually classified into three major forms, lichen amyloidosis, the commonest type, macular, and a rare nodular form.1,2 Macular and papular forms may co-exist in the same patient and is known as biphasic amyloidosis. Systemic amyloidosis, familial and hemodialysis-associated amyloidosis are may also present with skin involvement.5,6 Nodular amyloidosis typically presents as crusted nodules on the face, acral sites or the extremities. Macular amyloidosis is characterized by brownish macules in a rippled pattern, distributed predominantly over the trunk and extremities. Papular amyloidosis present as pruriginous brownish papular eruptions in the trunk and extremities and characterized by amyloid deposits in the papillary derma.1,2
AIH, PBC and PSC are the three main variants of autoimmune liver disease, and can all present as overlap syndromes.3,4 The AIH-PBC overlap syndrome is the most common form, affecting almost 10% of adults with AIH or PBC.3,4 Overlap syndromes show a very aggressive course, rapidly progressing to liver cirrhosis and liver failure without prompt diagnosis and treatment.
Although rarely there can be cases of isolated deposition of amyloid in the liver (primary hepatic amyloidosis), both immune and non-immune mediated liver diseases have also been associated with PLCA. While chronic hepatitis C virus infection has been reported to co-occur in at least two cases, suggesting it could consist in another extrahepatic manifestation,7,8 hepatitis B infection has only been associated with systemic amyloidosis to date.9 A case of nodular cutaneous amyloidosis in a patient with chronic alcoholic liver cirrhosis has also been recently reported.10 However, an important association between amyloidosis and autoimmune liver diseases has been recognized recently. Systemic AA amyloidosis has been associated with PBC11,12 and PSC.13,14 There is only one case in the published literature associating PBC and cutaneous amyloidosis in a 41 year old woman.15
The precise pathogenesis of PLCA has not been elucidated, but an increasing number of reports in the literature have associated it to autoimmune disorders, which suggests the possibility of a common underlying immune-mediated mechanism.16 Conditions as diverse as Sjogren, Behcet, IgA nephropathy, systemic lupus erythematosus and systemic sclerosis have been associated with PLCA.16–19 Nodular cutaneous amyloidosis results from extra-cellular deposition of fibril-forming monoclonal immunoglobulin-derived light chains produced by a small plasma cell clone, and in systemic amyloidosis the average plasma cell bone marrow infiltration is 7%. Abnormal folding of the light chains leads to amyloid deposition. In macular and papular amyloidosis, an accepted theory is that amyloid could derive from apoptotic keratinocyte-released cytokeratin degradation.1,2
It has been shown that cultivated keratinocytes are damaged by bilirubin, and hyperbilirubinemia can lead to widespread epidermal injury.20 In our case, we surmise that bilirubin deposition in skin could have led to keratinocyte apoptosis and cytokeratin release, leading to amyloid production. Interestingly, overlap liver autoimmune diseases are also associated to alterations in plasma cells and in immunoglobulin production. Besides a chronic hepatitis pattern of injury, periportal and sinusoidal plasma cells infiltrates are a prominent histopathological characteristic of AIH.21 Increased serum IgG and biopsy evidence of IgG-producing plasma cells have now been convincingly linked with both PSC and AIH.4,22 A plasma cells isotyping of IgM and IgG has even been proposed as a distinguishing variable, with overlap syndromes showing a IgG/IgM ratio > 1.23 Besides a state of chronic inflammation in overlap liver autoimmune diseases, plasma cell and immunoglobulin production abnormalities could account for the development of cutaneous amyloidosis in these cases.
There are not evidence-based treatment algorithms for the treatment of PLCA and overlap autoimmune liver diseases. Management of pruritus is essential in the management of PLCA. Topical steroid therapy, ultraviolet light therapy, and surgical treatment (excision, dermabrasion, shave excision) are useful as well. Although patients with cutaneous amyloidosis may develop systemic amyloidosis in the long term and warrant close follow up, this occurrence is rare.1,2,5 The management of overlap liver autoimmune disorders is based on anticholestatic therapy with ursodeoxycholic, combined with immunosuppressive therapy with corticosteroids and/or azathioprine, according to the course of disease.3,4 Liver transplantation is the treatment of choice in the setting of end-stage liver disease. Our patient was treated with a combination of ursodeoxycholic and prednisone; however, a very important limitation in this case is that the patient did not show to follow-up consultations, thereby, we could not evaluate the effect of treatment.
Conflict of InterestThe authors declare no conflict of interest.
All authors read and approved the final manuscript.