Background. Thrombocytopenia is a common hematologic disorder observed in patients with chronic hepatitis C virus (HCV) infection. Combined peginterferon (PEG-INF) and ribavirin treatment may exacerbate thrombocytopenia in patients with HCV.
Objective. The aim of this pilot clinical trial was to assess the efficacy, tolerability and safety of Danazol in thrombocytopenia associated with PEG-INF and ribavirin treatment in patients with HCV.
Material and methods. We included patients whose platelets were < 90,000/mm3 and who were undergoing antiviral treatment. Danazol (300–600 mg/day) was administered during and until the end of antiviral therapy [7.6 months (2 to 11 months)]. The monitoring was performed through platelet analysis and liver function tests. A viral load test was done at the beginning and end of treatment. Forty-nine patients receiving a combined therapy of PEG-INF, ribavirin and Danazol increased their platelet levels to 121,081/mm3 (46,000-216,000/mm3); 10.6% of patients gained > 100,000 platelets/mm3, and 71% of patients maintained their initial platelet levels. Sustained viral response (SVR) was achieved in 63% of patients. SVR rates were high in patients with genotype non 1 (78.7%) and decreased in patients with genotype 1 (60.1%). The increase in platelet levels was associated to an increase in fibrinogen levels and a decrease in the activity of ALT. By contrast, patients without SVR presented a delayed response to increased platelet levels and showed no significant improvement in liver function when they received Danazol.
Conclusion. Danazol can be used along with PEG-INF and ribavirin to treat thrombocytopenia in patients with HCV.
The current standard therapy for patients with chronic hepatitis C infection (HCV) combines pe-gylated interferon (PEG-IFN) and ribavirin for 24 or 48 weeks; this cures ~45% of patients infected with HCV genotype 1, and 80% of patients infected with genotypes 2 or 3. However, PEG-INF and ribavirin treatment is known to potentially exacerbate neutropenia and thrombocytopenia in those pa-tients.1,2
The frequency and diversity of adverse events associated with the use of interferon is quite significant. Virtually all treated patients report some manner of complaint attributed to PEG-INF at some time during therapy.3 However, most adverse events can be managed appropriately and premature discontinuation of therapy or prolonged dose reductions owing to side effects should not be required in most patients.
Hematological complications currently associated with PEG-INF treatment include anemia, neutropenia and thrombocytopenia due to myelosuppressive and bone marrow toxic effects.4,5 A decrease in platelet count has been specifically associated to PEG-INF-associated autoimmune thrombocytopenia. From the clinical standpoint, thrombocytopenia poses infrequent problems unless a severe decrease of platelet count is already present before therapy, such as in cirrhotic patients with portal hypertension and sple-nomegaly.6 If thrombocytopenia is severe and the condition does not improve, the first step is a temporal reduction to 20 to 50% of the dose or, in the worst case scenario, cancelling PEG-INF treatment. However, modifications in dosage decrease the chance of successful treatment and increase the risk of liver function impairment with hepatocellular carcinoma (HCC) as a potential consequence. Mild thrombocytopenia is a well-recognized complication of PEG-INF therapy.7
Danazol therapy seems to be a useful and well-tolerated treatment for refractory immune thrombo-cytopenia associated with several autoimmune diseases.8-10 The ways in which Danazol acts upon autoimmune thrombocytopenia are unknown. It has, however, been shown that Danazol therapy modifies the level of antiplatelet antibodies, inhibits the mononuclear phagocyte system, and reduces the complex of GPIIb-IIIa in patients with refractory autoimmune thrombocytopenia.11–13
The treatment of thrombocytopenia associated to antiviral therapy for HCV infection remains unresolved, but previous reports have shown Danazol improves thrombocytopenia and liver injury in rats with CCl4-induced fibrosis.14
ObjectiveThe aim of the present pilot clinical trial was to evaluate the efficacy, tolerability and safety of Dana-zol for increasing and maintaining platelet levels in chronic HCV patients receiving PEG-INF and riba-virin treatment.
Materials and MethodsPatient selectionPatients were recruited from the Liver Clinic at the Hospital of the Mexican Institute of Social Security in Cuernavaca, Morelos (Mexico), between January 2003 and December 2009. Patients of both sexes were eligible for inclusion if they were HCV RNA-positive, were receiving PEG-INF plus ribavi-rin treatment, developed thrombocytopenia (platelet count < 90,000 platelets/mm3), and had abnormal serum alanine aminotransferase levels on two occa-sions during the preceding six months, with compensated cirrhosis in the Child-Pugh class A or B. Patients with histories of drug and/or alcohol abuse, psychiatric illnesses, decompensated cirrhosis, positive hepatitis B surface antigen, positive anti-human immunodeficiency virus, or who suffered from other relevant concurrent medical conditions were excluded. Patients were also excluded if they had neutropenia (< 1,500 neutrophils/mm3), > 90,000 platelets/mm3; anemia (women < 12 g, men < 13 g of hemoglobin/dL); presence of autoimmune throm-bocytopenic purpura; human immunodeficiency virus; antinuclear antibodies (ANA); anti-smooth muscle antibodies; rheumatoid factor; decompensa-ted liver disease; alcohol or drug dependence; had taken glucocorticoids during the previous year; had danazol-associated allergies; were pregnant or breast feeding; had autoimmune-associated disease; used steroid therapy, and were unable to continue drug treatment for more than a month. Patients who missed a platelet count for more than two consecutive months, did not attend more than two appointments, and/or suffered severe side effects were excluded from the study. Cirrhosis was diagnosed in correlation to clinical manifestations and en-doscopic or ultrasound studies. The protocol was approved by the Institutional Review Board of the Mexican Institute of Social Security. The study was performed in accordance with the Declaration of Helsinki and amendments15 relevant to biomedical research involving human subjects, and the principles of the Guideline for Good Clinical Practice.16 All eligible volunteers were informed of the aim and risks of the study by the clinical researchers and provided written informed consent before enrollment.
Study design and end pointA prospective study with historical control was conducted with 49 patients suffering from chronic hepatitis C and PEG-INF-associated thrombocytope-nia, a platelet count < 90,000/mm3, and compensated Child-Pugh A or B liver impairment. Patients with genotype 1 were treated with PEG-INF alfa-2a (Pe-gasys®) 180 pg/week and ribavirin (Copegus®; 1,000 mg/day for those weighing < 75 kg and 1,200 mg/day for those weighing > 75 kg) during 48 weeks. Patients with genotype non-1 were treated with riba-virin (800 mg/day) for 24 weeks. The dose of Dana-zol depended on the platelet count. When the platelet count was between 90,000-80,000/mm3, the initial Danazol dose was 200 mg/day. If the platelet count was between 79,999-60,000/mm3, the Danazol dose was 300 mg/day; a count of < 60,000/mm3 received a 600 mg/day dose. This was increased month by month depending on the response in platelet count. Danazol treatment was stopped if patients presented severe side effects or toxicity-e.g., hepatocellular cholestasis with an increase in bilirubin levels, alkaline phosphatase (AP), or an increase in aminotransferases level (> 5 fold). If patients presented moderate side effects, the dose was reduced. Danazol was prescribed in a concurrent manner with PEG-INF and ribavirin for the duration of combined therapy in order to avoid adjusting interferon doses for thrombocytopenia. If necessary, Danazol treatment was continued for three months after interferon treatment finished in order to increase platelet counts.
Primary and secondary endpointsThe primary efficacy endpoint was to maintain or increase basal platelet level to 20,000, which was defined as a sustained platelet level above 45,000 plate-lets/mm3 and helped prevent adjustments to the PEG-INF dose or its temporary suspension. The secondary efficacy endpoints were biochemical im-provement of liver function and sustained virological response (SVR). Biochemical improvement was defined as a decrease in the alanine aminotransferase (ALT) level. SVR was defined as undetectable plasma HCV RNA (< 50 IU/mL) at 24 weeks post-HCV treatment.
All data were prospectively obtained from medical records and registered onto a structured database that included medical history, clinical status, relevant biochemical data, and blood cell count. Treatment data, including dose and duration of Danazol, as well as tolerance and adherence, were also registered. The monthly viral load was monitored at the beginning and end of HCV treatment, as well as 24 weeks later.
Adherence to treatment was monitored through interviews with the patient. Patients were also given a form where, after each query, they recorded the drugs they received each day for the duration of the month and dosage and dosing intervals, in addition to all adverse events related or unrelated to the monthly treatment.
Statistical analysisEach patient had an average 10 ± 3.5 measurements used in the statistical analysis. A bivariate analysis considering total response as the dependent variable and sociodemographic characteristics as independent variables was performed. Odds ratios and their corresponding confidence intervals were estimated in order to establish the magnitude of the association. In the intention-to-treat analysis, all patients who received at least one dose of Danazol were included, and patients without SVR and patients who were lost to follow-up were recorded as non-responders. Genotype was classified as 1 and non 1. For the continuous variables T-Student analysis was done. Results were analyzed using a commercial statistical software package (SPSS, for Windows Version 15). Association between parameters was examined using multinomial logistic regression. A p-value of < 0.05 was considered statistically significant.
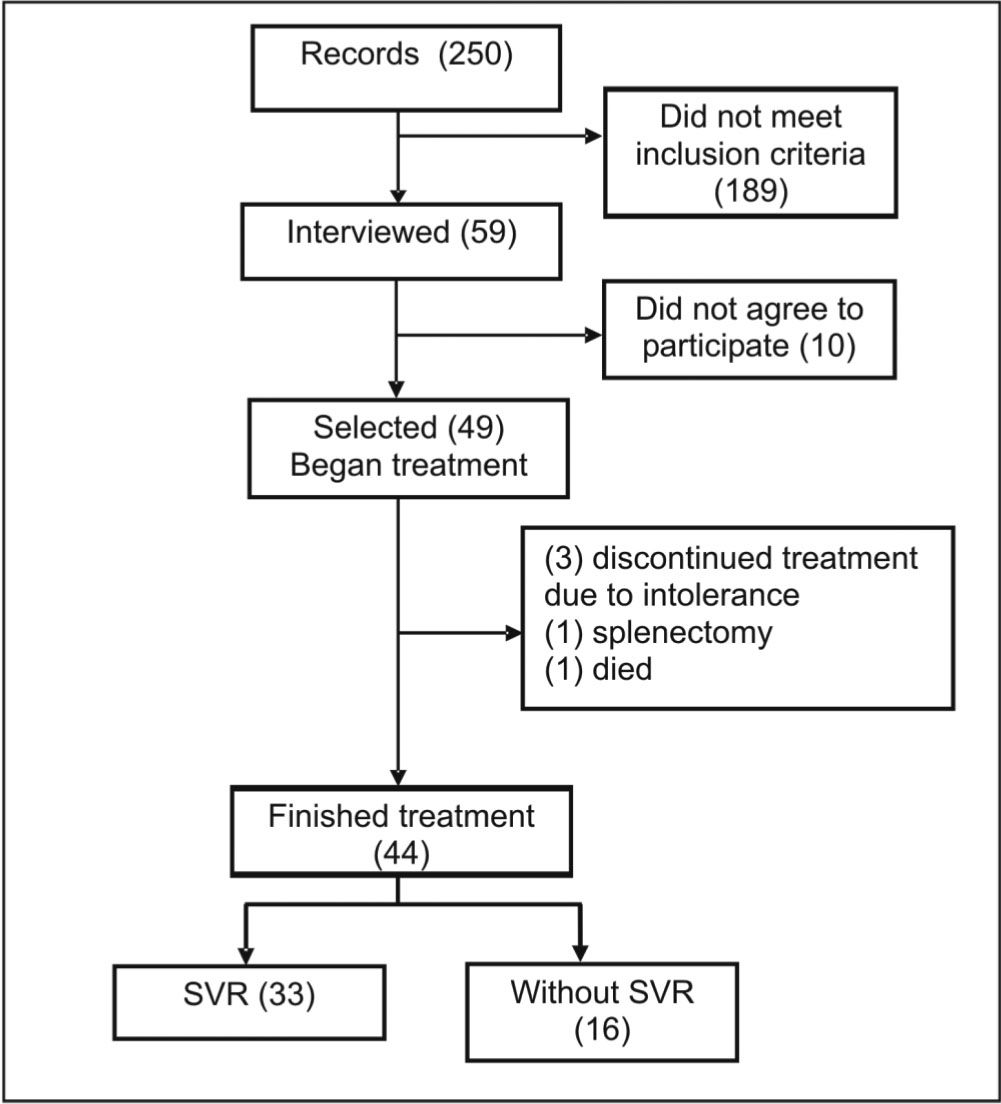
ResultsA total of 250 patients with HCV were identified from 2003 to 2009. Out of these, 57 were receiving PEG-INF plus ribavirin and had decreased platelet levels. Forty-nine patients (37 females and 12 males) were selected for the present study according to inclusion criteria. All were treated with Dana-zol; 46 responded to Danazol therapy and 44 finished the anti HCV treatment. Five patients withdrew prematurely from therapy; the reasons were (Figure 1):
- •
Decease (1 patient).
- •
Splenectomy (1 patient).
- •
Voluntary discontinued therapy due to PEG-INF plus ribavirin treatment intolerance (3 patients;).
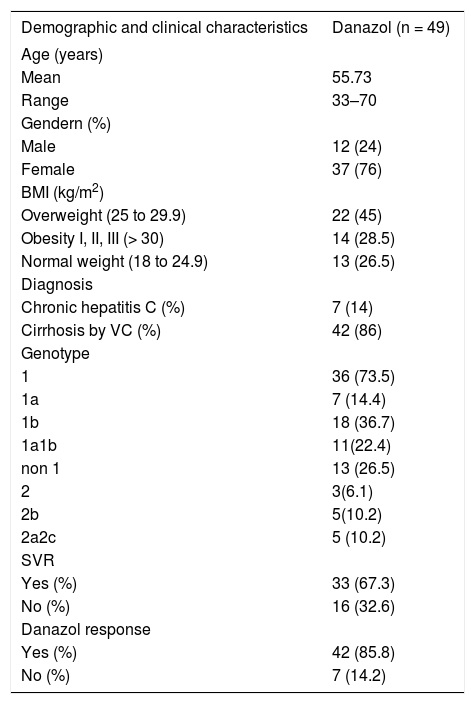
The demographic and clinical characteristics of the patients included in this analysis are listed in table 1. The median age was 55.73 years (range 3370 years), and a total of 33 patients had SVR. Pre-treatment diagnoses were chronic hepatitis C and cirrhosis for 7 patients (14 %) and 42 patients (86%) respectively. Mean body mass index (BMI) was high in 73.5%. Genotypes included:
- •
1a (14.4%).
- •
1b (36.7%).
- •
1a1b (22.4%).
- •
2 (6.1%).
- •
2b (10.2 %).
- •
2a2c (10.2%).
Demographic characteristics of patients.
| Demographic and clinical characteristics | Danazol (n = 49) |
|---|---|
| Age (years) | |
| Mean | 55.73 |
| Range | 33–70 |
| Gendern (%) | |
| Male | 12 (24) |
| Female | 37 (76) |
| BMI (kg/m2) | |
| Overweight (25 to 29.9) | 22 (45) |
| Obesity I, II, III (> 30) | 14 (28.5) |
| Normal weight (18 to 24.9) | 13 (26.5) |
| Diagnosis | |
| Chronic hepatitis C (%) | 7 (14) |
| Cirrhosis by VC (%) | 42 (86) |
| Genotype | |
| 1 | 36 (73.5) |
| 1a | 7 (14.4) |
| 1b | 18 (36.7) |
| 1a1b | 11(22.4) |
| non 1 | 13 (26.5) |
| 2 | 3(6.1) |
| 2b | 5(10.2) |
| 2a2c | 5 (10.2) |
| SVR | |
| Yes (%) | 33 (67.3) |
| No (%) | 16 (32.6) |
| Danazol response | |
| Yes (%) | 42 (85.8) |
| No (%) | 7 (14.2) |
BMI: Body mass index. Genotype non 1 includes all variants of genotype 2. SVR: sustained virological response.
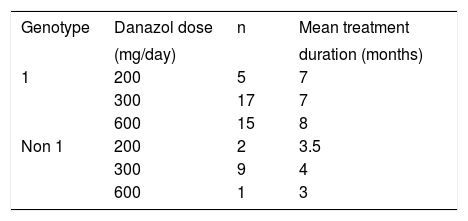
Table 2 shows the dosage schedule of Danazol treatment. Patients received different doses (200, 300 or 600 mg/day) depending on platelet levels and response. The time of treatment was shorter for those patients with genotype non 1 (3–4 months).
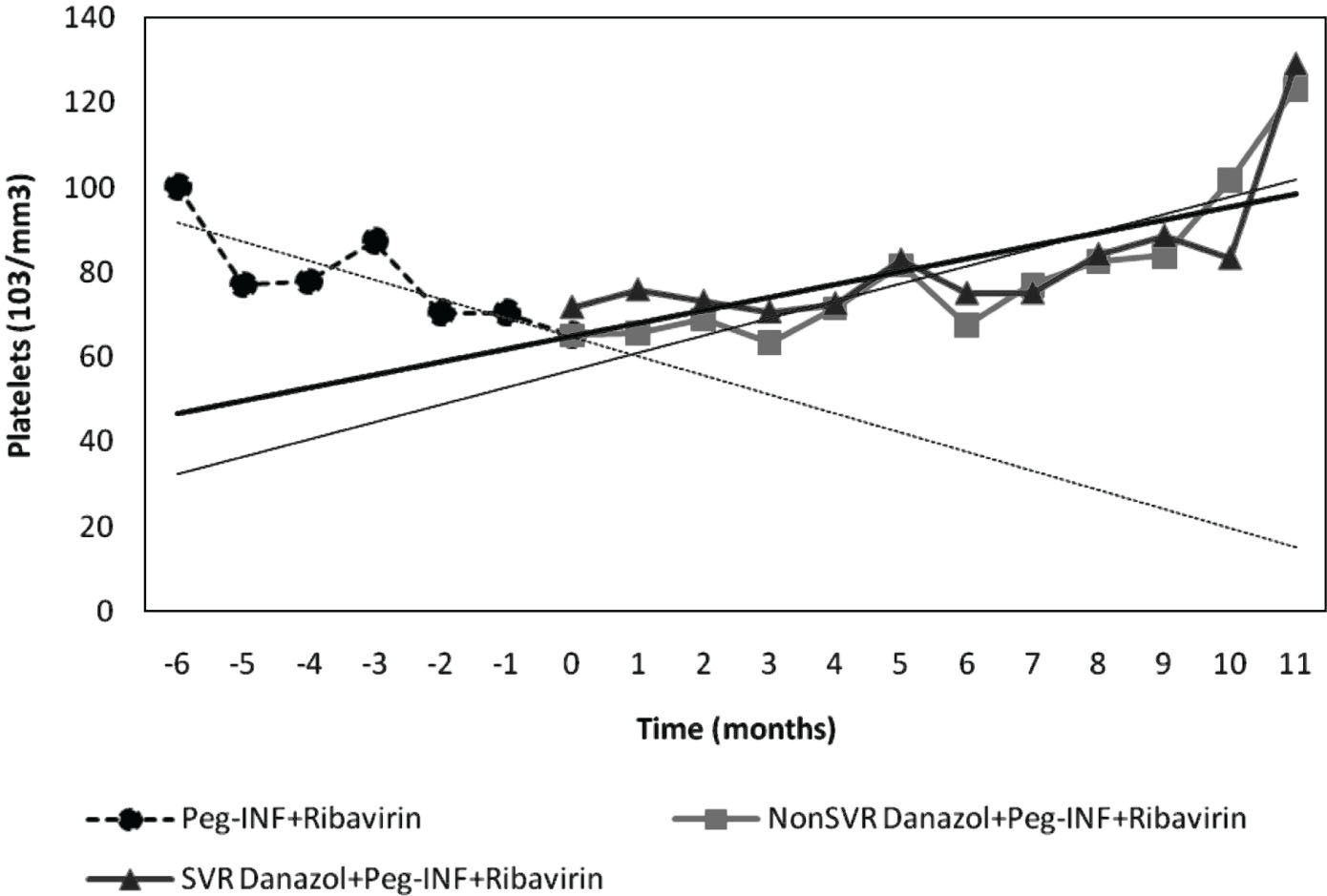
Platelet levelHistorical control of platelet levels prior to study showed a negative tendency with an average loss of 5,217 platelets/mm3/month before Danazol treat-ment. HCV patients treated with PEG-INF plus ri-bavirin had a basal platelet level of 69,067/mm3 (range 34,000-88,200/mm3). Upon receiving the combined PEG-INF, ribavirin and Danazol therapy, the tendency changed to positive (3,467/mm3/month). (Figure 2, Table 3). At the end of treatment, platelet levels had increased to 121,081/mm3 (46,000-216,000/mm3). Six patients (12.3%) had an increase above 100,000/mm3; 26 patients (53%) had an increase between 20,000 and 100,000/mm3; 10 patients (20.4 %) maintained their platelet levels, and the remaining 7 patients (14.2%) continued suffe-ring a decline in platelet levels and were considered unresponsive to Danazol after 11 months of treatment (Table 1). Figure 3 shows individual values of platelet levels before and after Danazol treatment, and we can confirm the differences following Dana-zol implementation, the tendency is to maintain levels of over 70,000 platelets/mm3.
Platelet level before and during Danazol addition to the treatment. Historical control platelet count in patients who completed the study (n = 44). Each point represents mean ± SD. * p = 0.001. † p = 0.003. ‡ p < 0.05. The lines represent linear regression (i.e. behavior in platelet levels).
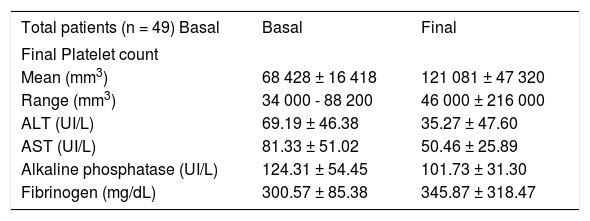
Hepatic functional parameters in patients receiving Peg-INF alfa 2a, ribavirin and Danazol.
| Total patients (n = 49) Basal | Basal | Final |
|---|---|---|
| Final Platelet count | ||
| Mean (mm3) | 68 428 ± 16 418 | 121 081 ± 47 320 |
| Range (mm3) | 34 000 - 88 200 | 46 000 ± 216 000 |
| ALT (UI/L) | 69.19 ± 46.38 | 35.27 ± 47.60 |
| AST (UI/L) | 81.33 ± 51.02 | 50.46 ± 25.89 |
| Alkaline phosphatase (UI/L) | 124.31 ± 54.45 | 101.73 ± 31.30 |
| Fibrinogen (mg/dL) | 300.57 ± 85.38 | 345.87 ± 318.47 |
ALT: Alanino amino transferase. AST: Aspartate amino transferase. Values are expressed as mean ± SD.
There was no statistical difference in platelet levels between patients with and without SVR, but we assume that the rate change in platelets is an approximate and linear function of time, so that the rate of change can be summarized by the slope. We compared it and found that the rate of change in platelet level was associated to SVR (p = 0.007, data not shown). Figure 4 shows platelet levels during Danazol treatment in patients with SVR and without SVR. As can be seen, patients without SVR had a delayed response (one month) to Danazol. However, at the end of the period, their platelet levels were similar to those of patients with SVR.
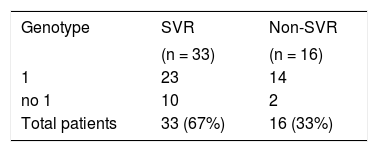
The increase in platelet levels was associated to an increase in fibrinogen levels and a decrease in the activities of ALT and AST (Table 3). SVR was attained by 67.3% (33 patients) of all patients (Table 4). Table 5 shows the predictors of sustained virological response. As can be seen, 65.1% were female and 55.5 % male. Patients older than fifty had lower SVR rates than younger ones (61.5 and 66.4%, respectively). Patients with cirrhosis had a lower SVR rate than those without cirrhosis (59.5 vs. 83.3%). Viral genotype also influenced the outcome: SVR was high in patients with genotype non 1 (78.7%) and lower in patients with genotype 1 (60.1%).
Predictors of sustained virological response (SVR).
| Parameter | *n | SVR % | Odds Ratio (95% CI) | p value |
|---|---|---|---|---|
| Sex | ||||
| Female | 372 | 65.1 | 1.5 (0.99-2.25) | 0.054 |
| Male | 128 | 55.5 | 1.0 | |
| Age | ||||
| < 50 | 140 | 66.4 | 1.0 | 0.309 |
| > 50 | 364 | 61.5 | 0.81 (0.54–1.22) | |
| BMI (kg/m2) | ||||
| 25–29.9 | 239 | 69 | 1.55 (0.98–2.45) | 0.061 |
| > 30 | 148 | 56.1 | 0.88 (0.5–1.5) | 0.636 |
| 18.5–24.9 | 117 | 59 | 1.0 | |
| Diagnosis | ||||
| Chronic Hepatitis C | 72 | 83.3 | 3.4 (1.8-6.5) | < 0.001† |
| Cirrhosis | 432 | 59.5 | 1.0 | |
| HCV Genotype | ||||
| 2 | 75 | 78.7 | 2.44 (1.4–4.4) | 0.003† |
| 1 | 429 | 60.1 | 1.0 |
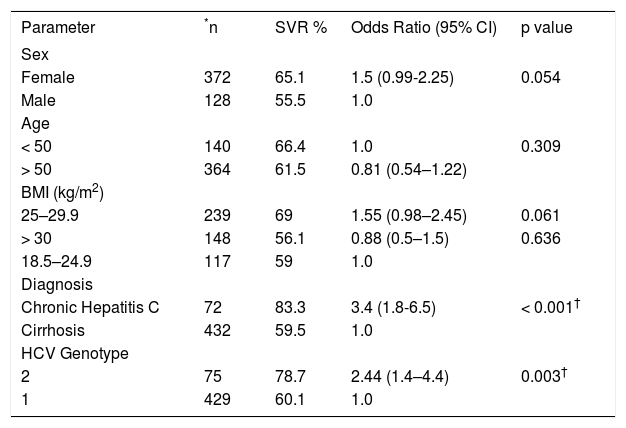
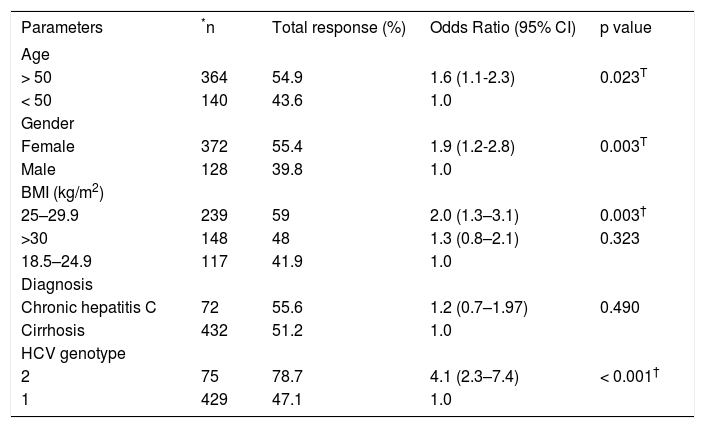
In the univariate analyses, significant predictors (e.g., age, gender, BMI, HCV genotype and enzymatic levels) were associated with SVR (Table 6). The probability of achieving a total response was significant in those patients with genotype non 1 (p < 0.001), OR = 4.1 (95% CI: 2.3; 7.4).
Predictors of total response two years after end of HVC treatment.
| Parameters | *n | Total response (%) | Odds Ratio (95% CI) | p value |
|---|---|---|---|---|
| Age | ||||
| > 50 | 364 | 54.9 | 1.6 (1.1-2.3) | 0.023T |
| < 50 | 140 | 43.6 | 1.0 | |
| Gender | ||||
| Female | 372 | 55.4 | 1.9 (1.2-2.8) | 0.003T |
| Male | 128 | 39.8 | 1.0 | |
| BMI (kg/m2) | ||||
| 25–29.9 | 239 | 59 | 2.0 (1.3–3.1) | 0.003† |
| >30 | 148 | 48 | 1.3 (0.8–2.1) | 0.323 |
| 18.5–24.9 | 117 | 41.9 | 1.0 | |
| Diagnosis | ||||
| Chronic hepatitis C | 72 | 55.6 | 1.2 (0.7–1.97) | 0.490 |
| Cirrhosis | 432 | 51.2 | 1.0 | |
| HCV genotype | ||||
| 2 | 75 | 78.7 | 4.1 (2.3–7.4) | < 0.001† |
| 1 | 429 | 47.1 | 1.0 |
Five out of 31 patients (16%) who received Dana-zol treatment and were HCV-negative 24 weeks after ending PEG-INF and Ribavirin treatment had detectable HCV RNA 2 years after the end of follow-up (data not shown).
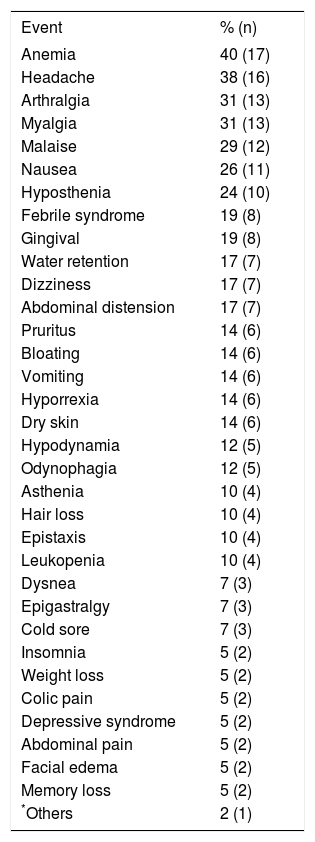
SafetyAll patients had at least one adverse event (AE) during treatment. Twenty-nine percent presented more than 10 AEs. Most treatment-related AEs were considered mild or moderate in terms of severity and were consistent with AEs reported for PEG-INF plus Ribavirin treatment as well as Da-nazol (e.g., headaches, arthritis and depression) (Table 7). Although all patients had AE, they tolerated Danazol treatment well until the end of follow-up.
Adverse events during treatment with Peg-INF, riba-virin and Danazol.
| Event | % (n) |
|---|---|
| Anemia | 40 (17) |
| Headache | 38 (16) |
| Arthralgia | 31 (13) |
| Myalgia | 31 (13) |
| Malaise | 29 (12) |
| Nausea | 26 (11) |
| Hyposthenia | 24 (10) |
| Febrile syndrome | 19 (8) |
| Gingival | 19 (8) |
| Water retention | 17 (7) |
| Dizziness | 17 (7) |
| Abdominal distension | 17 (7) |
| Pruritus | 14 (6) |
| Bloating | 14 (6) |
| Vomiting | 14 (6) |
| Hyporrexia | 14 (6) |
| Dry skin | 14 (6) |
| Hypodynamia | 12 (5) |
| Odynophagia | 12 (5) |
| Asthenia | 10 (4) |
| Hair loss | 10 (4) |
| Epistaxis | 10 (4) |
| Leukopenia | 10 (4) |
| Dysnea | 7 (3) |
| Epigastralgy | 7 (3) |
| Cold sore | 7 (3) |
| Insomnia | 5 (2) |
| Weight loss | 5 (2) |
| Colic pain | 5 (2) |
| Depressive syndrome | 5 (2) |
| Abdominal pain | 5 (2) |
| Facial edema | 5 (2) |
| Memory loss | 5 (2) |
| *Others | 2 (1) |
Others that were present in one patient include: hyperthermia, hyperpig-mented skin, chills, pallor, tremor, diarrhea syndrome, hives, jaundice, hypo-thyroidism, fatigue, constipation, pyrosis, ecchymosis, eye pain, variceal bleeding, neutropenia, otalgia, flu syndrome, hypersomnia, dermatopathies.
The main purpose of treating patients suffering from HCV infection with antiviral therapy is to attain total response or at least SVR and halt disease progression. The common medical management for thrombocytopenia associated to PEG-INF treatment for chronic HCV infection is to gradually reduce the dose of PEG-INF, but this hinders SVR and increases hepatocarcinoma risk for the patient. The present pilot clinical trial sought to evaluate the efficacy, tole-rability and safety of Danazol for increasing and maintaining platelet levels in chronic HCV patients receiving PEG-INF and ribavirin treatment.
In our cohort of 248 patients, 57 (22.9 %) presented thrombocytopenia and were at risk of having to modify their PEG-INF treatment, thus decreasing the probability SVR and total response. Thrombo-cytopenia is cited as a reason for reducing or suspending PEG-INF during treatment for hepatitis C in 3% of cases.5,7 In this pilot clinical trial, Danazol therapy was associated with stable platelet levels or a stop to platelet decrease. Patients treated with Da-nazol were less likely to require a reduction or temporal or definitive suspension of PEG-INF, which led to a high rate of SVR, fewer relapses, and high response rates. Patients treated with Danazol had a reduced risk of developing HCC. While Danazol treatment was associated with mild side effects, the proportion of patients without relapses was higher among those treated with Danazol than those who underwent a reduction in the dose of PEG-INF. Also, 6% of those who suffered a relapse after Dana-zol treatment responded after an additional course of therapy. HCV patients treated with PEG-INF, Riba-virin and Danazol showed an increase in platelet levels fibrinogen levels, as well as a decrease in ALT and AST activities. SVR was higher in patients with HCV genotype non-1 and in non-cirrhotic patients; it was attained in 67% of patients (33/49), while14% suffered relapses (7/49). Finally, we had a 53% rate of responders after two years of treatment (26/49). All these data suggest that PEG-INF therapy combined with Danazol could be used to effectively treat patients suffering from HCV-related thrombocytope-nia. This combined therapy avoids temporarily reducing or definitively stopping Peg-INF treatment and increases platelet levels.
A few studies have assessed the efficacy and safety of the antiviral treatment in cirrhotic patients. Available information shows SVR rates are between 20 and 40% lower with decompensated disease.17,18 The SVR rate in cirrhotic patients with portal hypertension was of 22%; it was 12.5% in patients with genotype 1 and 66.7% in those with genotypes 2 and 3 after PEG-IFN alpha-2b and ribavirin therapy.19 Our results show that cirrhotic patients had a lower chance of attaining SVR, but SVR rates were still higher, almost 60% higher overall.
Ours is the first study on Danazol efficacy and safety in a population of almost fifty patients where SRV rates were significantly higher than expected. The higher SVR rates seen in this study are not solely due to the permanence of the antiviral therapy. Previous studies by this group have shown that Da-nazol improves liver injury in rats, improving liver function and decreasing fibrosis.14
The present study shows that patients responded successfully to Danazol therapy without cessation of PEG-IFN and ribavirin therapy, even though some required prolonged treatment. The fact that Danazol therapy stopped the tendency toward platelet reduction and either maintained the count or produced a small increase suggests that this drug might inhibit platelet destruction. These results also suggest that thrombocytopenia has, at least in part, an autoimmune origin in these types of patients.20–22
Although, in the past, many therapeutic strategies have been employed to treat HCV-related thrombocytopenia (e.g. interferon dose reductions, oral steroids, intravenous immunoglobulins, sple-nectomy, etc.), the success rates have been variable and not always reproducible. The introduction of non-immunogenic second-generation thrombopoie-tin-mimetics (Eltrombopag and Romiplostim) has opened up a novel way to treat HCV-related throm-bocytopenia.23 However, rather than prevent platelet destruction, these agents have increased the production of platelets, presumably overwhelming the immune system and resulting in normal platelet counts in individuals refractory to or dependent on other therapies.24 For example, Eltrombopag therapy successfully achieved the primary endpoint platelet counts of > 50,000/μL in phase II & III, randomized, double-blind, placebo-controlled trials.25 McHutchison, et al. stated that the use Eltrombo-pag increased the platelet counts in a dose-dependent manner in patients with thrombocytopenia due to HCV-related cirrhosis, allowing for the beginning of antiviral therapy.26 In our study, Danazol treatment was given to patients already receiving Peg-IFN and ribavirin treatment. This maintained platelet levels in 42 patients (85.8%) and allowed the continuation of treatment and a high rate of SVR.
Meta-analysis of host related factors has shown that patient age could be associated to SVR rate, since patients < 50 had a better SVR rate.5,27 Our re-sults show that patients < 50 were slightly more likely to attain antiviral treatment response, but there were no differences in SVR. In addition, dose reductions appeared to have negative SVR impact in elderly patients. It is therefore important to minimize PEG-IFN and Ribavirin dose reductions by effectively managing treatment-related adverse events in elderly patients.
Little is known about the real impact of gender on the characteristics that influence the effectiveness and safety of antiviral treatment for HCC patients. Results from some studies suggest that women and men react differently to combined therapy.
These differences do not influence SVR in young men but do so in the case of elderly ones with decreased SVR rates.2,28 Our results show there are no differences between women and men regarding SVR, but women are twice as likely to respond.
Thrombocytopenia (platelet count < 150,000/ mm3) is a common complication in patients with chronic liver disease (CLD); it has been observed in up to 76% of patients and contributes significantly to the cost of managing this disease. There are currently no therapeutic agents specifically designed to treat CLD-associated thrombocytopenia. The few therapeutic options that currently exist include: platelet transfusion, splenectomy, splenic embolization and splenic irradiation. Most of these are associated with significant limitations such as short-term or unpredictable efficacy, development of refractoriness, and serious adverse events (including infection, sepsis, abscesses or death). Because of that, some studies on the efficacy and safety of PEG-INF and ribavirin do not include patients with thrombocyto-penia of 100,000 or lower.29
Multiple mechanisms can contribute to the development of thrombocytopenia, including splenic platelet sequestration, bone marrow suppression, and reductions in the level or activity of the hematopoie-tic growth factor thrombopoietin (TPO).30 The development of thrombocytopenia among patients with chronic HCV infection may predict higher risks of future complications and comorbidity. In a retrospective analysis of 60,000 patients with CLD, it was found that 3.86% of those with HCV had thrombocytopenia. Among thrombocytopenic patients with hepatitis C, 27% had bleeding events and required platelet transfusions.31
The use of Peg-INF in the treatment of patients with cirrhosis has been limited because of its adverse effects, particularly on bone marrow. PEG-IFN treatment can lead to development of thrombocytope-nia due to an inhibition of the proliferation and differentiation of stem cells in the bone.1,32 Furthermore, PEG-IFN can induce the production of anti-platelet antibodies as an adverse event. Usually, bone marrow examinations of patients treated with PEG-IFN show abundant megakaryocytes and apparently normal thrombocyte differentiation without significant disruption of megakaryocyte maturation. Davis, et al.33 studied chronic HCV infection patients without hypersplenism or evidence of platelet autoantibodies and found these patients showed a significant increase in platelet count following successful viral load reduction with interferon-a (IFN-a) treatment. The authors suggested the virus had a direct effect on platelet production and that IFN-α therapy indirectly promoted platelet production by suppressing HCV. However, IFN-α itself has myelosuppressive effects that may independently lower the platelet count to thrombocytopenic levels.34 Thrombocytopenia itself endangers the life of the patient. Furthermore, dose modification of IFN due to thrombocytopenia and other hematological complications may result in a reduction in SVR.35
Few studies have explored strategies to stimulate megakaryocyte production and maturation in bone marrow mediated by cytokines or growth factors. There is one report about the use of recombinant human interleukin-11, which acts as a thrombopoie-tic growth factor; however, no improvement in platelet levels was observed and patients suffered side effects associated to interleukin therapy.6,12
This study demonstrates the efficacy and safety of Danazol therapy (200 to 600 mg/day) in patients with HCV infection undergoing PEG-IFN treatment. The effectiveness of Danazol therapy allowed patients to continue PEG-IFN and ribavirin treatment without decreasing doses or temporally or definitively suspending therapy, additionally obtaining 71% of SVR. There are some reports regarding the hepatotoxic effects of Danazol after more than two years of use,8,36 but no reports of AEs during short-time periods have been found. Present results showed that Danazol treatment (6-11 months) was safe for chronic HCV patients undergoing PEG-IFN and ribavirin treatment and suffering from compensated cirrhosis Child-Pugh A or B.
The prevention of HCC recurrence, or tertiary prevention, is currently one of the most challenging tasks in hepatology. Several cohort studies conducted in the 1990s unanimously concluded that patients who achieved SVR or persistent normalization of ALT had a lower risk of developing HCC.37 It is now known that modifications in the dosage of PEG-IFN can effectively restore platelet counts, but this approach is limited because it negatively impacts the efficacy of antiviral therapy. Dose modification has been shown to jeopardize SVR in patients with chronic hepatitis C. A study involving chronic hepatitis C patients receiving PEG-IFN plus ribavirin treatment found that a reduction of 20% in PEG-IFN, especially during the first 12 weeks of treatment, reduced its efficacy.38 It is therefore important to avoid dose reductions of PEG-IFN and ribavirin to increase SVR.3 PEG-IFN and ribavirin comprise the standard treatment for chronic HCV. However, as is the case with any other disease, optimal results require an individual approach in order to minimize relapses. Patients suffering from cirrhosis, insulin resistance/diabetes, or who are > 50 present challenging cases because they have a higher risk of reduced SVR or relapse. To prevent dose reductions and finish therapy, disabling side-effects must be counteracted and this includes a judicious use of Danazol for se-vere thrombocytopenia.
ConclusionDanazol could be an alternative therapeutic remedy for PEG-INF and ribavirin treatment-associated thrombocytopenia in chronic HVC patients. Present results show that Danazol is effective, safe and well tolerated. Further studies are needed to elucidate this drug’s mechanism of action in chronic HCV.
Abbreviations- •
HCV: Hepatitis C virus infection.
- •
INF-α: Interferon-α.
- •
PEG-INF: Peginterferon alfa-2a.
- •
CLD: Chronic liver disease.
- •
TPO: Thrombopoietin.
- •
ITP: Idiophatic thrombocytopenic purpura.
- •
ANA: Antinuclear antibodies.
- •
SVR: Sustained virological response.
- •
ALT: Alanine aminotransferase.
- •
AST: Aspartate aminotransferase.
- •
BMI: Body mass index.
- •
AE: Adverse event.
- •
AP: Alkaline phosphatase.
- •
TB: Total bilirubin.
- •
PEG-INF: Pegylated interferon.
- •
HCC: Hepatocellular carcinoma.