Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer and the third leading cause of cancer related death worldwide. In recent years, the prevalence of HCC has increased in both developing and developed countries. Most HCC cases develop in the presence of advanced chronic liver disease related to viral hepatitis. In particular hepatitis B virus and hepatitis C virus infections are considered as major HCC risk factors worldwide. However, current studies provide strong evidence for increasing numbers of HCC in nonalcoholic fatty liver disease (NAFLD). NAFLD represents the hepatic manifestation of metabolic syndrome which is based on obesity and insulin resistance. Epidemiologic data clearly demonstrates that NAFLD and obesity-related disorders are significant risk factors for tumor development in general and HCC in particular. As a consequence of life style changes towards higher calorie intake and less exercise, obesity and metabolic syndrome are spreading all over the world. Due to this increase in obesity and metabolic syndrome NAFLD-related HCC will become a major health care problem in the future. In conclusion, better understanding of the impact of NAFLD and obesity in the development of HCC will improve our treatment strategies of HCC and allow preventive measures.
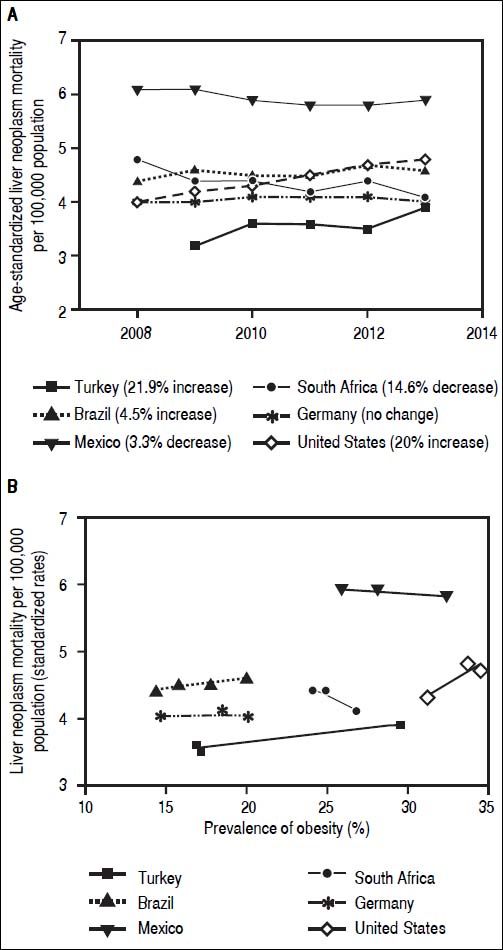
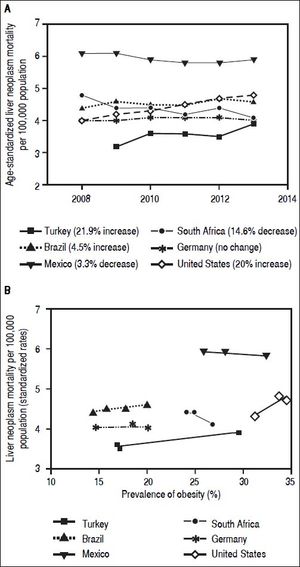
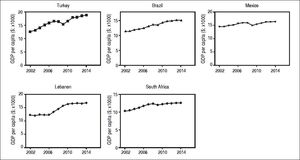
Hepatocellular carcinoma (HCC) constitutes approximately 80% of primary liver cancers worldwide. It is the fifth most common cause of cancer in men, the seventh in women (523,000 cases per year, 7.9% of all cancers; 226,000 cases per year, 6.5% of all cancers; respectively) and the third leading cause of cancer death.1 In development of HCC, several etiologic factors play a role. Causes of HCC are hepatitis B virus (HBV), hepatitis C virus (HCV) infections, alcoholic liver disease, nonalcoholic fatty liver disease (NAFLD), cryptogenic cirrhosis, aflatoxin B1, and chronic metabolic liver diseases.2 Prevalence and distribution of these risk factors are highly variable and depend on the geographic region and ethnic group.1,3 In recent years, the incidence of HCC has increased in many countries in North and South America, Europe and Asia. Moreover, HCC mortality rates have increased in USA as well as developing countries4 (Figure 1). Turkey, as one example for developing countries, exhibited growing rates of HCC mortality by 21.9% from 2009 to 2013 which is similar to the United States (20%) (Figure 1A). A Mexican study showed that the specific-cause mortality rate of HCC increased by 14% between 2000 and 2006,5 while it remained constant between 2008 and 2014. This might be due to already high mortality rates compared to other developing countries. Interestingly, malignant neoplasms of the liver decreased by 14.6% in South Africa from 2008 to 2014. Again there are significant differences geographically and regionally for growth rates and main etiologies of HCC.6,7Currently HBV is the main cause of HCC in developing countries, while HCV is the main cause in developed countries.5,7 Though, growing numbers of NAFLD and non-alcoholic steatohepatitis (NASH) prevalence lead to rising numbers of NASH-associated HCC, which in some studies has been shown to be the most prevalent etiology by now.8 Indeed in some countries parallel increases of liver neoplasm mortality and prevalence of obesity can be observed (Figure 1B). Due to a limited number of available datapoints these developments do not correlate significantly. An inverse association between liver neoplasm mortality and prevalence of obesity in few countries may be due to other etiologies for HCC being the main cause.
Mortality rates of malignant liver neoplasm and their correlation with prevalence of obesity in developing and developed countries. A-B. Mortality rates from primary liver neoplasm are increasing in Turkey and Brazil over the last years, but slightly decreased in Mexico (which has relatively high rates), and South Africa. These rates are steady in Germany and United States as examples for industrialized countries. Source of data: OECD Health Statistics 2015 Database.38
Similar to many other developing countries few large population studies have been conducted on the epidemiology of HCC in Turkey. According to the Turkish Ministry of Health report in 2003, the incidence of HCC was 0.83/100,000. Several epidemiological studies between 2001-2014 suggested that the major risk factors of HCC in Turkey are HBV, HCV, and excessive alcohol consumption with ranges of44.4-65.7%, 15.0-28.6%, and 5.9-15.9 %, respectively. 9-15,57 Nevertheless, etiologic factors were not distributed homogenously between different regions of Turkey. Especially striking about these numbers is that 525% of HCC cases remain without a clear cause. Unfortunately, there is a lack of studies on HCC in Turkey taking NAFLD or NASH into account.
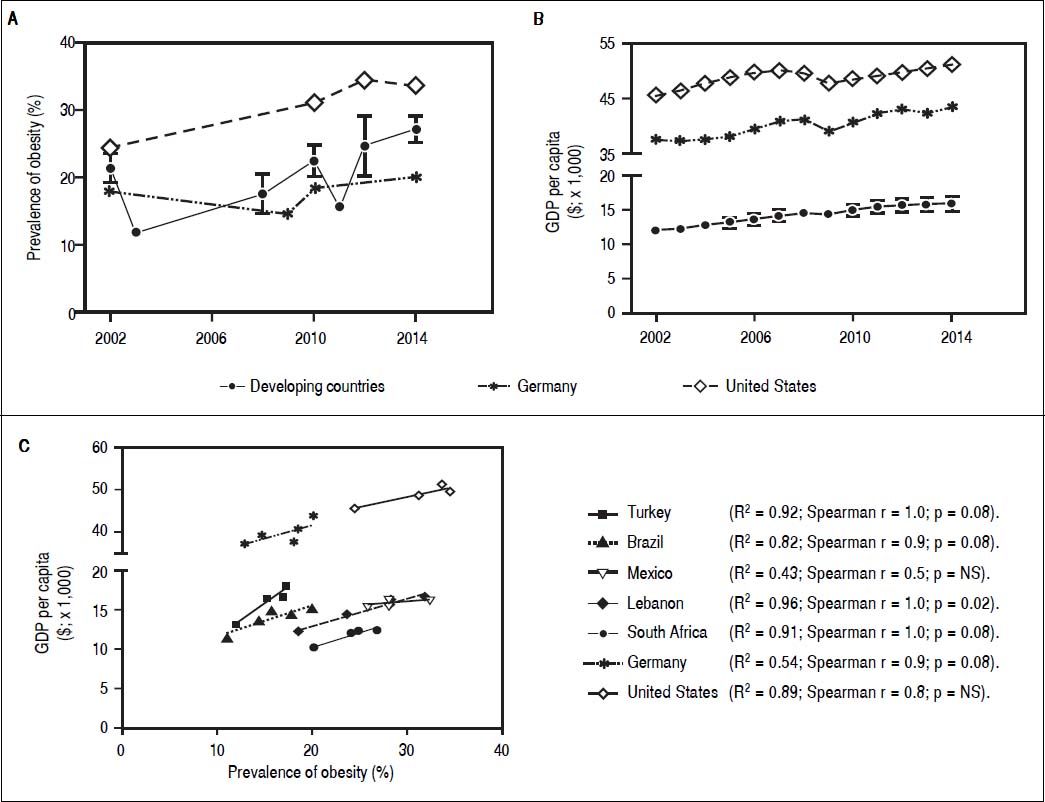
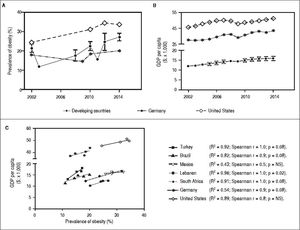
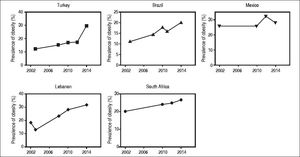
NAFLD encompasses a spectrum of disease states ranging from simple fatty liver (steatosis hepatitis, NAFL) to nonalcoholic steatohepatitis (NASH). Progressive NAFLD can result in fibrosis, cirrhosis, and HCC. NAFLD is recognized as the hepatic manifestation of the metabolic syndrome (MetS) which comprises obesity, type II diabetes mellitus (T2DM) or insulin resistance (IR), hypertension, and dyslipidemia.16 Obesity is defined as excessive fat accumulation as a result of excess calorie uptake17 and is probably the central risk factor and mechanism in development of IR and subsequently MetS. According to the World Health Organization (WHO), there are currently at least 1.4 billion adults (35% of adults) overweight of whom 500 million (13% of adults) are obese worldwide. The prevalence of obesity has increased in all over the world including developing countries as Brazil,18 Mexico,19 Turkey,20 Lebanon, and South Africa during the last decades. Mean prevalence of obesity for selected developing countries is in a similar range as in Germany and United States (Figure 2A, Supplementary figure 1). In Mexico the prevalence of obesity has only slightly increased on an already high proportion, with up to 25% obese in some regions of Mexico.19 A dramatic increase from 18.6% obesity in 1990 to 21.9% in 2000 was documented in Turkey.20 Current estimates range up to 35% obese individuals in Turkey, which exceeds latest numbers of central Europe (approximately 15.5% obese and 34.6% overweight with strong regional variation). Eventually, several population-based, epidemiological and clinical studies, conducted in various geographic areas, have clearly demonstrated a significantly increased incidence of HCC in patients with diabetes, NAFLD and obesity, and it is expected that their incidence will continue to increase globally. Therefore, it is crucial to elaborate the role of NAFLD and obesity as risk factors of HCC. This review seeks to summarize the current status, epidemiology, and risk factors of HCC in developing countries. Furthermore it aims to provide an overview of the link between obesity, NAFLD and development of HCC as well as the economic effects of those. Awareness for this severe future health care problem in developing countries must be raised. Here we compared five developing countries, which are Mexico and Brazil (South America), Turkey (Europe-Asia), Lebanon (Middle East-Asia), and South Africa (Africa), to two developed countries, Germany and United States regarding liver malignancy and prevalence of obesity. As an example of developing countries on the verge of industrialization, a particular focus is on Turkey due to its specific socio-economic, educational and industrialized characteristics.
Parallel increase of obesity rates and GDP per capita PPP ($x1000) in developing countries. A. Development of obesity prevalence in developing countries (mean ± standard deviation for 5 developing countries; individua development for each country is shown in Supplementary figures 1A-1E) in comparison to USA and Germany as industrialized examples. Despite fluctuations and heterogeneous data sources a continuous increase of obesity prevalence in developing and industrialized countries can be observed. B. Development of gross domestic product (GDP)per capita in developing and industrialized countries. For developing countries the mean ± standard deviation for 5 examples countries is given (individua development for each country is shown in Supplementary figures 2A-2E). All developing countries and Germany and USA exhibit a continuous growth of GDP. For industrialized countries the increase is margina as GDP/ capita is already high. C. Correlation of obesity prevalence and GDP/capita in the 7 countries. For all countries, except Mexico, development of obesity and GDP/capita show high correlation coefficients, though without reaching signifcance. This is probably due to a low number of time points with reliable data for both parameters available. Sources of Obesity rates among adults, self-reported: Turkish Statistica Institute (TURKSTAT), Turkey Health Interview Survey (2008, 2010, 2012) and School of Public Health of the Ministry of Health, National Burden of Disease and Cost Effectiveness (2003). Data refer to population aged > 15 years old (2008, 2010, 2012), > 18 years old (2003) and World Health Organization (WHO) Global Health Observatory (GHO) data (2015). Source of GDP per capita: GDP per capita (constant 2011 international $, PPP, indicator code: NY.GDP.PCAP.PP.KD), World Bank.
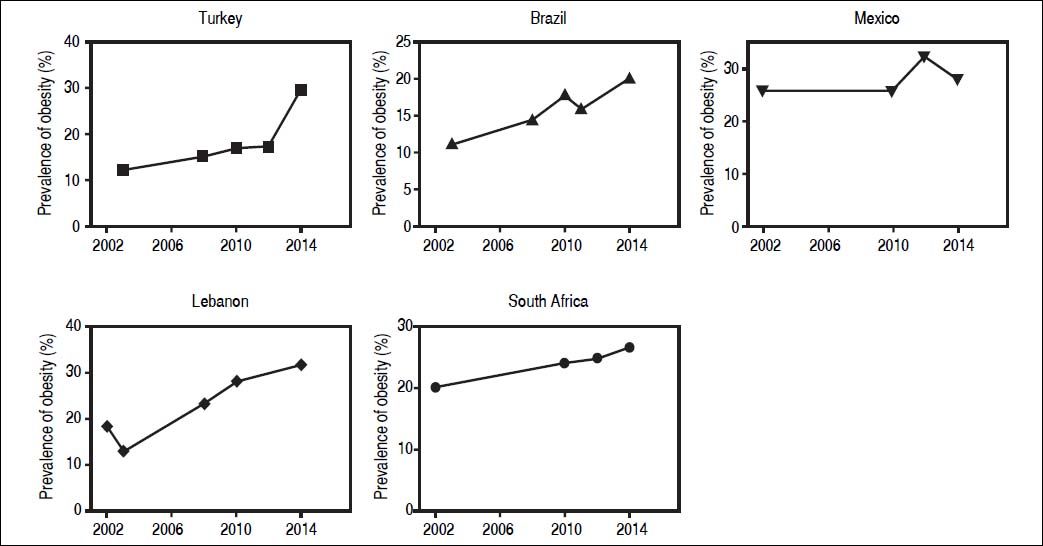
Obesity prevalence of selected developing countries over the last decade. Developing countries selected as examples exhibit increasing rates of obesity prevalence from 2002 to 2014. Mexico shows a relatively stable prevalence, although on an already high proportion. Sources of Obesity rates among adults, self-reported: Turkish Statistical Institute (TURKSTAT), Turkey Health Interview Survey (2008, 2010, 2012) and School of Public Health of the Ministry of Health, National Burden of Disease and Cost Effectiveness (2003). Data refer to population aged > 15 years old (2008, 2010, 2012), > 18 years old (2003) and World Health Organization (WHO) Global Heath Observatory (GHO) data (2015).
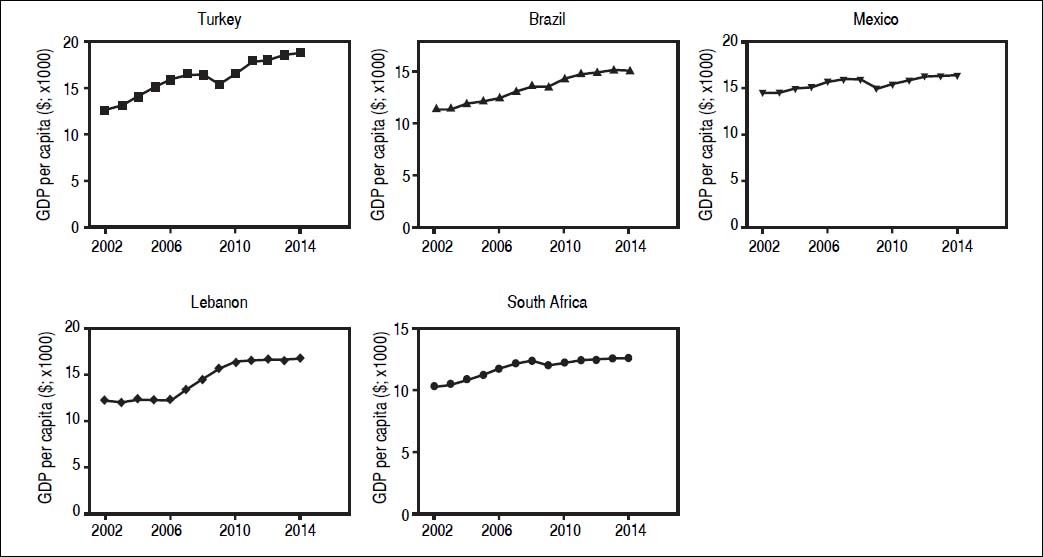
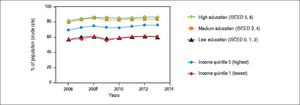
Obesity is defined as excessive fat accumulation (Body Mass Index [BMI] > 30 kg/m2) as a result of excess calorie uptake17 due to more easily available food with high calorie density and overconsumption, and/or insufficient activity and exercise. In recent years prevalence of obesity has increased dramatically worldwide ("obesity pandemic"). This is probably a result of a spreading "western" life style in industrialized countries, which is associated with readily available food with high sugar and fat content, and a more sedentary life style with less activity and exercise. It is assumed that approximately 3.3 billion adults (57.8%) will become overweight or obese by 2030, if the current trend is maintained.21-22 The prevalence of obesity has increased also in Turkey, with latest WHO verified data (2008) indicating 40.3% of the Turkish population as overweight (BMI 25-29.99 kg/m2) and 16.1% obese (BMI > 30 kg/m2). The follow up to the Turkish Diabetes Epidemiology Study (TURDEP-II) survey showed that the prevalence of obesity had increased from 22.3% to 36%.23 In other studies the mean prevalence of obesity ranged from 19.4% (14.4% in men; 24.6% in women)24 up to 35.1% in a large multicenter nationwide study (15,468 individuals; 14 centers in seven different regions of Turkey; conducted 2000-2002).25 Other large studies found a prevalence of obesity around 30%.26-27 Especially striking are consistently higher percentages for obesity in women in all studies. It has been proposed that this might be a consequence of the particular culture and life style, where outdoor activity and exercise are uncommon for women.28 Thus prevalence of obesity among women in Turkey (approximately 35%) is similar to countries with highest rates of obesity in the world such as South Africa, Chile, and Mexico, according to the Cancer Screening and Early Diagnosis Centers (KETEM) study (n = 74,492).29 According to WHO health statistics prevalence of obesity increased dramatically in most countries from 2002 to 2014. In Turkey the prevalence of obesity increased by 17.5%, in Brazil by 9%, in Lebanon by 13.3%, and by 6.8% in South Africa. These rates are similar to those observed in the United States (9.2%) from 2002 to 2014 (Figure 2; Supplementary figure 1). One factor promoting obesity is available or preferred food choice. Especially food with high sugar/carbohydrate and high fat content (high calorie density) may facilitate weight gain. According to the Turkish Ministry of Health, 44.0% of daily energy is sourced through bread only while 58.0% is sourced from bread and other grain derivatives. The consumption of fruit and vegetables is not sufficient and there is a tendency towards higher fast food consumption in urban areas of Turkey. Overall, current nutritional habits in Turkey seem to promote weight gain. In developed countries (i.e. Australia, Canada, USA, England, France), obesity is more common among people with lower socio-economic status and there is a negative correlation between obesity and education.30 In a recent systematic review it has been shown that low prevalence of obesity was recorded in low-income countries (i.e. Bangladesh, India, Vietnam) while high prevalence of obesity was reported in upper-middle-income countries (i.e. Russia, Poland, Seychelles).31 Moreover, a high prevalence of obesity has been shown among individuals with lower socioeconomic status in middle-income countries. Though, high obesity rates shift to lower income groups in high-income countries [gross domestic product (GDP per capita > US $12,275)].27 The reversal hypothesis describes a differential influence of income and/education on obesity depending on the GDP.32 A recent study including data from 70 countries, the reversal hypothesis was supported, suggesting that obesity is more prevalent among well-educated individuals in low income countries but becomes more prevalent in uneducated individuals in middle to high income countries.33 In developing countries such as Turkey, Brazil, Lebanon and South Africa, obesity rates among adults show a strong correlation (r2 is between 0.8-0.96) with a growing GDP per capita (constant 2011 international $ purchasing power parity; indicator code NY.GDP.PCAP.PP.KD) (Figures 2B-2C; Supplementary figure 2). In Turkey, as example of developing countries, perceived health status is lower in lowest income and low education groups (Supplementary figure 3). This would suggest that Turkey, Brazil, and Lebanon are on the track of many developing countries with increasing GDP and a parallel rise in obesity rates among less educated parts of the population. This emphasizes the importance of information and education regarding nutrient consumption and physical activity for the population in developing countries. Another important factor for development of obesity is physical activity and exercise. There is no representative data on physical activity (during leisure time) in Turkey. One study suggests, that activity and exercise are very uncommon in Turkey, with more than 50% participants stating to perform no physical activities in their spare time.34 Taken together there is a quite large population overweight or obese in Turkey with percentages reaching proportions of the USA. These numbers seem to be continuously growing and the common culture and life style (general food choices, urbanization with increased consumption of fast food, low physical activity in large parts of the population) in developing countries seem to further promote this problem.
Gross domestic product of selected developing countries over the last decade. Gross domestic product (GDP) per capita in all examples of developing countries has increased over the last decade. GDP per capita (constant 2011 international $, PPP, indicator code: NY.GDP.PCAP.PP.KD), World Bank.
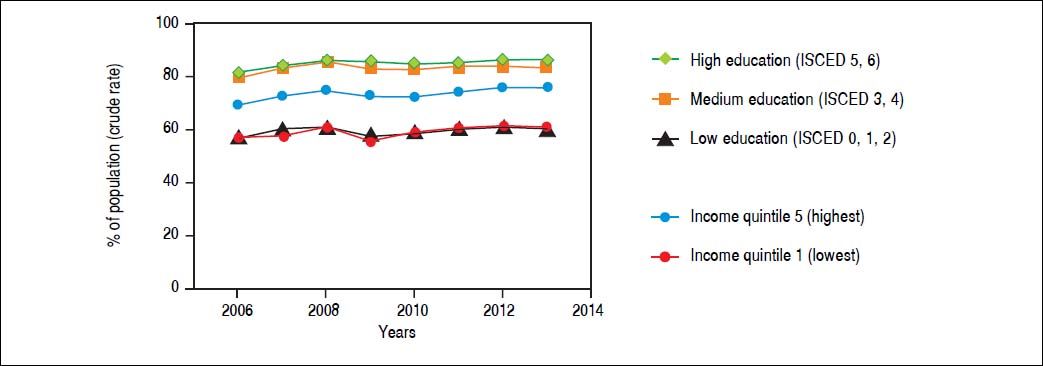
Perceived health status by socio-economic status in Turkey. Data refers to percentage of the population in good/very good health. Source of data: OECD Health Statistics 2015 Database.38
The increasing rate of obesity causes rising health care expenses and accordingly a massive economic burden in USA and UK.35 Studies in western countries show that the economic cost of obesity increases over time and expenses of the health care system for obesity was already over 2% in France in 1995.36 In Australia (a country with relatively low prevalence of obesity among industrialized societies), the total annual direct cost of overweight and obesity was $21 billion in 2005.37 According to the Centers for Disease Control and Prevention, National Public Health Institute of the United States, obese individuals cause 42% more healthcare costs than normal weight individuals. A study from England predicted that about 50-60% of the people by 2050 could be clinically obese and estimated cost of obesity per year would be £49.9 billion, if there is no precaution against obesity trends.39 Strikingly a parallel increase of obesity and liver related mortality has already been observed in Brazil from 2001 to 2009.18 In developing countries, obesity is becoming a more important problem continuously and will represent a serious health problem with drastically increased health care costs in the future.38 Preventive measures, especially education programs to limit further growth of the obesity pandemic and associated health care costs are urgently needed for developing countries.
Prevalence of Insulin Resistance, Diabetes and Metabolic Syndrome in Turkey as an Example of Developing CountriesFollowing the obesity pandemic the prevalence of insulin resistance has increased globally in the recent years. In US, it is estimated that the prevalence of pre-diabetic patients has risen from 29% in 2000 to 38.5% in 2012.40 According to the TURDEP II study the prevalence of prediabetic patients increased by 106% from 2002 to 2013 and reached 30.8% in Turkey.23
Diabetes mellitus (DM) has become the leading cause of death in the most countries worldwide.41 The prevalence of DM in USA is 14.3% and in European countries it is almost 8.5%, with the lowest in Moldova with 2.4% and the highest in Turkey with 14.9%.42,43 Almost 33,000 deaths were attributed to DM in Turkey annually.44 A population based study revealed that the prevalence of DM increased by 90% in Turkey within 12 years.23 Moreover, it was projected that the prevalence of DM will reach to 31.5% in Turkey by the year 2025.44 Another projection model reached a similar proportion with a predicted prevalence of DM of at least 28.3% by 2030.45
In the last decade all components of metabolic syndrome have increased dramatically all over the world.46Thus, there is an overall trend of uncontrollable increase in the prevalence of metabolic syndrome.47 In the USA the prevalence of MetS increased from 32.9% in 2003-2004 to 34.7% in 2011-2012.48 In the Turkish adult population, according to Adult Treatment Panel III criteria, the overall prevalence of MetS was estimated to be near 28.8% in the Mediterranean region of Turkey and 26.9% in the Northern region.49,50 However, it reached up to 43.2% among elderly subjects in the same regions and up to 61.7% in the central part of Turkey.50,51
There is a clear connection between insulin resistance and NAFLD.52,53 Generally, hyperinsulinemia is a frequent feature of chronic liver diseases regardless of etiology.54 Moreover, higher levels of serum insulin are a significant risk factor for HCC progression not only in NAFLD, but also in chronic viral and alcoholic hepatitis patients.54 Besides HCC, hyperinsulinemia was attributed as risk factor for solid organ tumors in non-diabetic subjects.55,56
Taken together prevalence of insulin resistance and MetS in Turkey is as high as in industrialized countries, similar to the rates of overweight and obesity. Furthermore, there is a trend of continuing increase of this risk factor for multiple co-morbidities and elevated mortality in Turkey.
Prevalence of Nonalcoholic Fatty Liver Disease in Developing CountriesAs described above NAFLD represents the liver manifestation of the metabolic syndrome and is closely associated to obesity and T2DM.57 Progression of NAFLD to NASH, cirrhosis, and HCC causes liver-related morbidity and mortality.17 In parallel to the worldwide obesity pandemic, NAFLD rates are increasing in industrialized countries and those adopting the "western" life style. Prevalence of NAFLD is ranging from 20% to 50% depending on definition criteria and diagnostic methods used in most studies. It is estimated that prevalence of NAFLD is between 10-46% in the USA, 15-40% in European countries, and 9-40% in the Asian population.58,59 Prevalence rates of NAFLD are higher with increasing BMI16 and can reach proportions of 5080% in obese.60 Approximately 90% of patients with NAFLD have at least one feature of MetS61,62 and NAFLD may be involved in the pathogenesis of insulin resistance and MetS.63 In developing countries, there are limited data regarding the prevalence of NAFLD. It seems that awareness for the risks of obesity and NAFLD are not very high in those countries, as the focus in liver disease pathologies is still mostly on viral hepatitides. Nevertheless, based on the above discussed numbers of obesity and diabetes in populations of developing countries, it is highly probable that a significant number of individuals have undiagnosed NAFLD. Studies in other populations have shown that roughly two thirds of diabetic patients may have NAFLD.64,65 Prevalence of NAFLD is increasing not only in adults but also in obese children and varies between 2.6% and 9.6% associated with sex, age, and ethnicity of children.66 In several studies among children, prevalence of NAFLD ranged between 13% and 80% and was correlated to obesity rates.63 In another study MetS, defined according to modified WHO criteria adapted for children, was found in 27.2% of young people, with a significantly higher rate among obese adolescents aged 12-18 years (37.6%) than among obese children aged 7-11 years (20%).67 Furthermore, in one study from Turkey prevalence of MetS in obese children with NAFLD was significantly higher than in those without liver disorders (54.8% vs. 14.9%, respectively).61 Despite a lack of current data on NAFLD in developing countries, obesity and diabetes rates suggest a significant proportion of individuals may be affected, which will further increase due to growing numbers of child and adolescent obesity.
Nafld as a Growing Cause of HCCIn recent years, especially in developed and many industrialized countries, NAFLD is considered the most common underlying HCC risk factor (59%) followed by diabetes (36%) and HCV infection (22%).3,68NAFLD has been described as the sole growing chronic liver disease in the USA, while all other chronic liver diseases remained at a stable proportion.69 In a German single center study, the proportion of NASH-associated HCC was 24% and NASH represented the leading cause of HCC in this study.8 Since then a growing body of evidence has demonstrated that NAFLD is an important risk factor for HCC development3 and that HCC may occur in NAFLD even without cirrhotic al-terations.8,70-71 On a global scale the decrease of HCV prevalence with a parallel increase of obesity and subsequently NAFLD will lead to a shift toward higher rates of NAFLD-associated HCC. While this has been recognized by most industrialized countries, in many developing countries or those with currently still high HCV rates, this gradual shift seems to go largely unnoticed.
Obesity and Nafld as Underlying Cause of HCCAs described above a global rise of NAFLD following the obesity epidemic is expected and already visible in industrialized countries. In consequence of this development HCC-incidence due to NAFLD will increase with a delay of a few years. By now a significantly increased incidence of HCC in obese patients has been documented in various regions.72 In a cohort of 900,000 American adults, the risk of dying from liver cancer was 4.5 times higher in obese men compared to a control group.3 Epidemiologic data demonstrates a parallel rise in prevalence of obesity, NAFLD, and HCC. A meta-analysis from Europe, the USA, and Asia showed that relative risks to develop HCC were 1.17 for overweight and 1.89 for obese individuals.22Diabetes increases risk of HCC three-fold, according to an American-population-based study.73 NAFLD, which is present in up to 90% of all obese persons and up to 70% of T2DM patients, appears to play a key role in HCC development. In Mexico a parallel increase of liver cancer mortality and obesity in the population have been described, confirming associations of metabolic syndrome and HCC.5 Unfortunately in most studies on HCC from other developing countries, NAFLD and NASH as cause for liver tumors are neglected, while still high rates of HCV and HBV associated HCC are presented. Most studies performed in developing countries do not discuss NAFLD in the setting of HCC. In parallel 5-25% of HCC cases remain as cryptogenic or "idiopathic". In one study from Turkey the proportion of NASH-associated HCC was given as 3.5% in 2010.14 Compared to the proportion of the population overweight or diabetic in developing countries, especially in Turkey, this ratio seems rather low. There are several factors that may complicate this issue and could lead to erroneous numbers. The main risk factors for HCC recognized in developing countries still are viral hepatitides. Once a viral cause has been established as diagnosis, other risk factors as obesity or diabetes are not tested for (at least they are not presented in the described studies). In addition many "idiopathic cases" can be found in the studies on HCC, while it has long been established that NAFLD may be the real cause of cryp-togenic HCC.74 Finally NAFLD or even obesity alone may aggravate any chronic liver disease (including viral hepatitides) and could thus further promote tumor development in HCV or HBV. This might be the case in Turkey and other developing countries, although no data is available on metabolic risk factors in common descriptions of HCC cohorts.
Currently data on NAFLD-associated HCC is extremely scarce in developing countries. Awareness for NAFLD in obese and/or diabetic patients and associated risks for the liver has to be increased in clinicians in these regions. Moreover the serious health risks of NAFLD, including development of HCC from non-cirrhotic livers, should be considered.
ConclusionsNAFLD is the most common cause for chronic liver disease in developed countries which is closely associated with obesity. In developing countries obesity rates are similar to those in the USA, though prevalence of NAFLD is presented as low or widely unknown. Increasing prevalence of NAFLD-associated HCC globally results from improved prevention of HCV/HBV infections in developing countries on the one hand and rising numbers of NAFLD following the obesity pandemic. Higher income and a change of life style towards "western" habits may further aggravate the obesity problem in developing countries. Prevention of obesity and NAFLD remain the best long-term strategy to avoid serious health care problems in the near future. Turkey is in a unique situation among developing countries on the verge of industrialization and there is already a large proportion of the population overweight or obese. Obesity associated co-morbidities of the liver seem to be far less common than in other industrialized nations. Quick action to counter the trend of continuing weight gain and spread of the obesity epidemic might safe developing countries from a massive health care problem. As no treatment for NAFLD is available, yet, an effort should be made to expand general education on a healthy life style to avert a drastic increase of NAFLD-related morbidity, in particular from HCC.
Abbreviations- •
BMI: body mass index.
- •
HBV: hepatitis B virus.
- •
HCC: hepatocellular carcinoma.
- •
HCV: hepatitis C virus.
- •
KETEM: Turkey Cancer Screening and Early Diagnosis Centers.
- •
MetS: metabolic syndrome.
- •
NAFLD: nonalcoholic fatty liver disease.
- •
NASH: nonalcoholic steatohepatitis.
- •
T2DM: type 2 diabetes mellitus.
- •
WHO: World Health Organization.
The authors have no competing interests to disclose. No writing assistance was utilized in the production of this manuscript.
Financial SupportsSupported by the Wilhelm Laupitz Foundation (A.C.) and by the TUBITAK-2219 Post-doc research scholarship program (A.A.).