Introduction. Hepatopulmonary syndrome (HPS) is characterized by a clinical triad of liver disease and/or portal hypertension, intrapulmonary vascular dilatation and abnormal arterial oxygenation. These conditions can worsen muscle strength, exercise capacity and functionality in the affected population.
Objective. The objective of this study was to compare exercise capacity, functional condition and respiratory muscle strength in cirrhotic patients diagnosed with HPS and cirrhotic patients without this diagnosis.
Material and methods. This cross-sectional study used a convenience sample consisting of 178 patients (92 patients with HPS and 86 patients without HPS) with a diagnosis of liver cirrhosis caused by either alcohol consumption or the hepatitis C virus (HCV). Peak oxygen consumption (VO2 peak) was used to verify exercise capacity, the six-minute walk test (6MWT) was used to test functionality, and manovacuometry was used to evaluate the strength of the respiratory muscles. The Kolmogorov-Smirnov test and Student’s t-test were used for the statistical analysis. The data were analyzed using SPSS 16.00, and p < 0.05 was considered significant.
Results. The group of patients with the diagnosis of HPS exhibited a lower VO2 peak (14.2 ± 2.3 vs. 17.6 ± 2.6, p < 0.001), shorter distance walked in the 6MWT (340.8 ± 50.9 vs. 416.5 ± 91.4, p < 0.001), lower maximal inspiratory pressure (-49.1 ± 9.8 vs. -74.2 ± 13.9, p = 0.001) and lower maximum expiratory pressure (60.1 ± 12.2 vs. 76.8 ± 14.7, p = 0.001).
Conclusion. The group of cirrhotic patients diagnosed with HPS exhibited lower values for VO2 peak, distance walked in the 6MWT and respiratory muscle strength than the cirrhotic patients not diagnosed with HPS.
Hepatic cirrhosis is characterized by the diffuse replacement of the normal liver structure by nodules with abnormal structure surrounded by fibrosis. It occurs in the final stage of a series of liver pathological processes due to various causes.1 Its complications include the metabolic changes associated with malnutrition in the patients, who lose large amounts of muscle mass and then exhibit changes in functionality and a condition of physical inactivity. The combination of all these factors negatively influences the Activities of Daily Living (ADL) and quality of life of this population.2–5
The treatment of patients with complicated cirrhosis is complex and necessarily broad, with poor longterm survival prospects. Liver transplantation (LTx) arguably allows a higher survival rate for these patients and also reduces the treatment cost.6–8 Thus, many candidates spend a long time on the waiting list, which enhances the risk of development of new complications that in turn worsen their functionality.
Although its association with the severity of liver disease is controversial, hepatopulmonary syndrome (HPS), which is characterized by a clinical triad involving liver disease and/or portal hypertension, intrapulmonary vascular dilatation and abnormal arterial oxygenation, is one of the complications associated with cirrhosis. It has a prevalence of 16 to 24% and presents with very unspecific signs and symptoms.9–13
The lack of studies addressing the physical aspects of HPS makes the identification of its impact on the natural history of liver disease more difficult. Changes in oxygenation and gas exchange may worsen the functionality and consequently the quality of life of the affected patients.
Therefore, the goal of this study is to compare the distance walked during the six-minute walk test (6MWT), oxygen consumption (VO2 peak) and respiratory muscle strength between cirrhotic patients on the LTx waiting list who have been diagnosed with HPS and cirrhotic patients on the LTx waiting list who have not been diagnosed with HPS and also to determine whether there is any association of the distance walked during the 6MWT and VO2 peak with respiratory muscle strength in cirrhotic patients.
Material and MethodsThis work was a cross-sectional study using a convenience sample consisting of 178 patients from a single center (92 patients with HPS and 86 without HPS) diagnosed with cirrhosis caused by either the hepatitis C virus (HCV) or alcohol consumption. All patients were part of a group of about six hundred cirrhotic patients who have monitoring at the Hepatic Transplant Service of the Holy House of Mercy Hospital Complex of Porto Alegre (Ambulatório de Transplante Hepático do Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Rio Grande do Sul state-Brazil, Rio Grande do Sul State - Brazil) and were potential candidates for liver transplantation, but were not hospitalized.
The exclusion criteria were as follows: significant obstructive ventilatory impairment, defined by a Tiffeneau index lower than 0.70 with forced expiratory volume in one second (FEV1) lower than 80% predicted; a significant restrictive ventilatory defect defined by a forced vital capacity (FVC) lower than 70% predicted; severe hepatic encephalopathy (grade III and IV); degenerative neuromuscular disease; severe hemodynamic instability; presence of intracardiac shunt; or presence of hepatocellular carcinoma (HCC). All patients signed the free and informed consent form, and the project was approved by the Research Ethics Committee of the Holy House of Mercy Hospital Complex of Porto Alegre, under the opinion 331.068.
Hepatopulmonary syndrome-diagnosisThe diagnosis of HPS was determined according to pre-established criteria. Cirrhotic patients were submitted to a contrast echocardiogram (CE), where agitated saline solution was injected into circulation via the antecubital vein. The microbubbles resulting from this process have diameters ranging between 60 and 90 μm, which is larger than the diameter of the normal capillary bed (8 to 15 μm), and thus, they opacify only the right heart chambers. However, with the loss of the anatomic barrier resulting from the dilation of the intrapulmonary capillary bed, the microbubbles can reach the left heart chambers approximately 3-6 cycles after their appearance in the right chambers. Associated with CE, the gasometric parameters were evaluated, especially the alveolar-arterial oxygen gradient (P(A-a)O2). because analyzing the pressure of oxygen in arterial blood (PaO2) alone may underestimate the real level of hypoxemia. We use the criterion of Aguillar Porres, et al.14 Although the author suggests the presence of an alveolar-arterial gradient greater than or equal to 15 mmHg, we chose to use a value greater than or equal to 20 mmHg to avoid false positive diagnosis, and classify the syndrome according to the degree of hypoxemia.14,15
Oxygen consumptionVO2 peak was used to evaluate exercise capacity. In this evaluation, each patient was monitored with a three-channel electrocardiograph (Dixtal) coupled to an oscilloscope. Initially, a 15-min rhythm recording based on the derivation corresponding to D2 was obtained from the patient at rest. Subsequently, a heart rhythm recording (D2 derivation) and an electrocardiogram trace (derivation corresponding to V1, aVF, CM5) were simultaneously obtained from the patient during a 15-min exercise period. The modified Bruce protocol with gas exchange analysis was used. The exercise was interrupted if the patients had symptoms that would prevent its continuation and/or represent a risk, such as the appearance of complex ventricular arrhythmias, intraventricular and/or atrioventricular conduction disorders or even bradyarrhythmias. In the analysis, only tests in which the patients reached the anaerobic threshold (AT) were considered to ensure that everyone had reached a submaximal exercise level. The AT was expressed in relation to VO2 in mL/min (STPD, standard temperature and pressure, dry) and was identified by the VO2 value at which the respiratory exchange ratio (R=VcO2/Vo2) was equal to or greater than one and continued increasing in subsequent respiration cycles. The analysis of the occurrence of arrhythmias was especially valued, including the total number of ventricular extrasystoles, the number of pairs of ventricular extrasystoles and the number of episodes of sustained and non-sustained ventricular tachycardia both at rest and during exercise.16
Six-minute walk test (6MWT)The 6MWT was used to assess the patients’ functional condition. This test was performed in a 30-meter flat, straight hallway that was free of any type of obstacles. Before starting the test, all patients were provided instructions by the evaluator; during the test, they received standardized verbal encouragement every minute to walk the longest distance possible. The distance walked was measured at the end of the test. The patients were monitored by respiratory rate, heart rate and peripheral oxygen saturation using a Nonin oximeter (9500, USA). The sensation of dyspnea and fatigue in the lower limbs was assessed using the modified Borg scale (0-10 scale) according to the American Thoracic Society. Except for the distance walked, all variables were collected both before the test and after the end of the test.17
Respiratory muscle strengthTo measure respiratory muscle strength, a digital manovacuometer (MVD 500, Globalmed®) was used, which was calibrated before each data collection session. To assess maximal inspiratory pressure (MIP), the patient was asked to perform a maximal expiration to the level of residual volume and, after the equipment was correctly positioned in the mouth, to achieve a maximum forced inspiration. To evaluate maximum expiratory pressure (MEP), the patient was asked to initiate the maneuver starting at total lung capacity, which was followed by a maximal forced expiration. To perform the maneuvers, the equipment was positioned correctly in the patient’s mouth. A nose clip was used to prevent air leaks, and the manovacuometer had a purge hole leak. The maneuver was required to be maintained for at least one second and to have a total time of at least two seconds to verify the peak pressure. The results were obtained after five maneuvers with an interval of at least one minute between them, when a minimum of three acceptable maneuvers had been performed, i.e., no more than 10% difference between their values. Then, the highest pressure in centimeters of water (cm H2O) was recorded, and the normal values recommended by the Brazilian Society of Pneumology and Tisiology (Sociedade Brasileira de Pneumologia e Tisiologia) were used.18,19
The Kolmogorov-Smirnov test was used to verify the normality of the sample. Student’s t-test was used to compare 6MWT performance, VO2 peak, MIP and MEP among the groups. Finally, the Pearson correlation coefficient was used to correlate 6MWT and VO2 peak with MIP and MEP.
The data were analyzed using SPSS 16.0 software. The level of significance was set at 5%, and p < 0.05 was considered significant.
ResultsThe clinical and anthropometric features of the population are described in table 1. There are no statistically significant differences between the two groups regarding age, height, weight, BMI, Model for End Stage Liver Disease (MELD) score, classification according to the Child Pugh score, etiology of cirrhosis or tobacco smoking, abdominal girth.
Anthropometric and clinical features of the sample.
| Variable | HPS (n = 92) | NHPS (n = 86) | p |
|---|---|---|---|
| Age (years) | 59.4 ± 7.10 | 57.7 ± 8.20 | 0.9 |
| Height (cm) | 169.7 ± 6.4 | 170.5 ± 7.1 | 0.8 |
| Weight (kg) | 71.6 ± 10.8 | 70.3 ± 9.7 | 0.9 |
| BMI | 25.6 ± 2.2 | 25 ± 2.5 | 0.9 |
| MELD | 17.2 ± 2.1 | 17.0 ± 3.0 | 0.9 |
| Tobacco smoking (n) | 7 | 11 | 0.8 |
| Abdominal girth | 86.3 ± 7.5 | 88.4 ± 9.1 | 0.6 |
| Child Pugh A (n) | 40 | 42 | 0.9 |
| Child Pugh B (n) | 39 | 35 | 0.9 |
| Child Pugh C (n) | 13 | 9 | 0.8 |
| HCV (n) | 62 | 59 | 0.8 |
| Alcoholic cirrhosis (n) | 30 | 27 | 0.8 |
HPS: group of patients with hepatopulmonary syndrome. NHPS: group of patients without hepatopulmonary syndrome. MELD: Model for End Stage Liver Disease. Child Pugh: Child Pugh Score A, B or C. HCV: cirrhosis caused by hepatitis C virus. BMI: body mass index.
The patients from the HPS group exhibited a lower PaO2 (68.9± 9.3 vs. 88.1 ± 10.1, p = 0.01) and a higher P(A-a)O2 (23.9 ± 1.72 vs. 13.4±1.65, p=0.01), and there was no difference between the two groups in echocardiographic and spirometric variables.
According to the criterion of Aguilar Porres, et al.14 twelve patients were classifed as mild (P(A-a)O2 ≥ 20 mmHg and PaO2 ≥ 80 mmHg), seventy-three were classified as moderate (P(A-a)O2 ≥ 20 mmHg and PaO2 ≥ 60 < 80 mmHg), 5 as severe (P(A-a)O2 ≥ 20 mmHg and PaO2 ≥ 50 < 60) and only two as very severe (P(A-a) O2 ≥ 20 mmHg and PaO2 < 50).
Table 2 compares VO2 peak, 6MWT and respiratory muscle strength between the groups. The HPS group exhibited a lower peak (14.2 ± 2.3 vs. 17.6 ± 2.6, p < 0.001), shorter distance walked in the 6MWT (340.8 ± 50.9 vs. 416.5 ± 91.4, p < 0.001), lower MIP (-49.1 ± 9.8 vs. -74.2 ± 13.9, p = 0.001) and lower MEP (60.1 ± 12.2 vs. 76.8 ± 14.7, p = 0.001) than the non-HPS group. In addition, both groups presented a lower performance than predicted for VO2 peak, 6MWT and respiratory muscle strength. The predicted value of the six-minute walk test is derived from the Paul LE, et al. equation.20
Comparison of the maximal oxygen consumption, six-minute walk test and respiratory muscle strength.
| Variable | HPS (n=92) | NHPS (n=86) | p |
|---|---|---|---|
| 6MWT (meters) | 340.8 ± 50.9 | 416.5 ± 91.4 | < 0.001 |
| VO2 peak (ml/kg) | 14.2 ± 2.3 | 17.6 ± 2.6 | <0.001 |
| MIP (cmH2O) | -49.1 ± 9.8 | - 74.2 ± 13.9 | 0.001 |
| MEP (cmH2O) | 60.1 ± 12.25 | 76.8 ± 14.7 | 0.001 |
| 6MWT predicted (meters) | 549.3±71 | 572.3±58 | 0.8 |
| VO2 peak predicted (mL/kg) | 17,7 | 20,3 | 0.8 |
| MIP predicted (cmH2O) | -162±57 | -165±54 | 0.9 |
| MEP predicted (cmH2O) | 254±61 | 259±53 | 0.8 |
HPS: Group of patients with hepatopulmonary syndrome; NHPS: Group of patients without hepatopulmonary syndrome, 6MWT: Distance walked in the six-minute walk test; VO2 peak: peak oxygen consumption; MIP: maximal inspiratory pressure; MEP: maximal expiratory pressure.
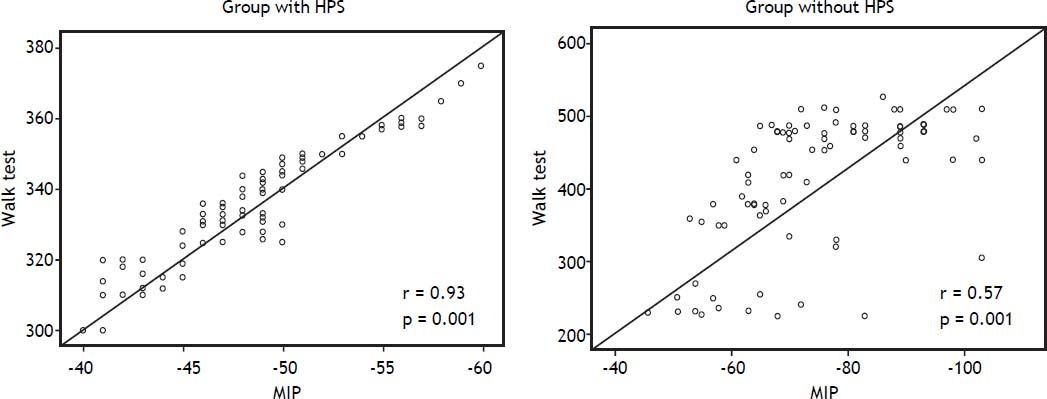
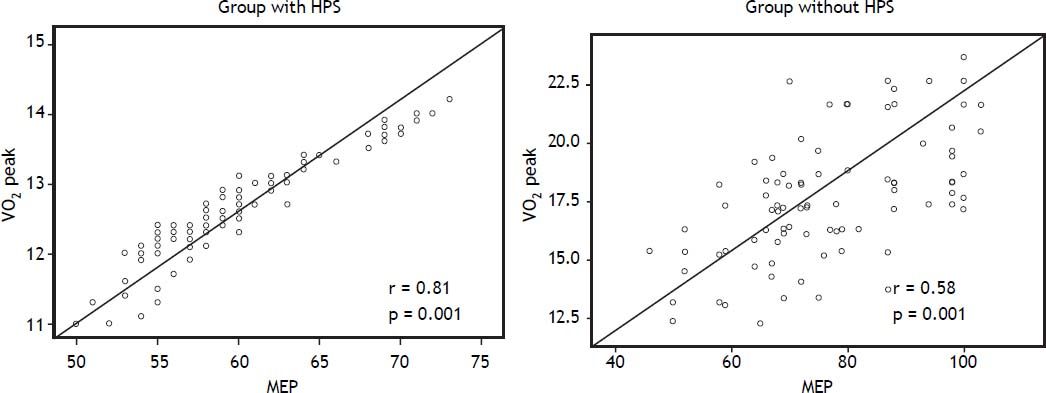
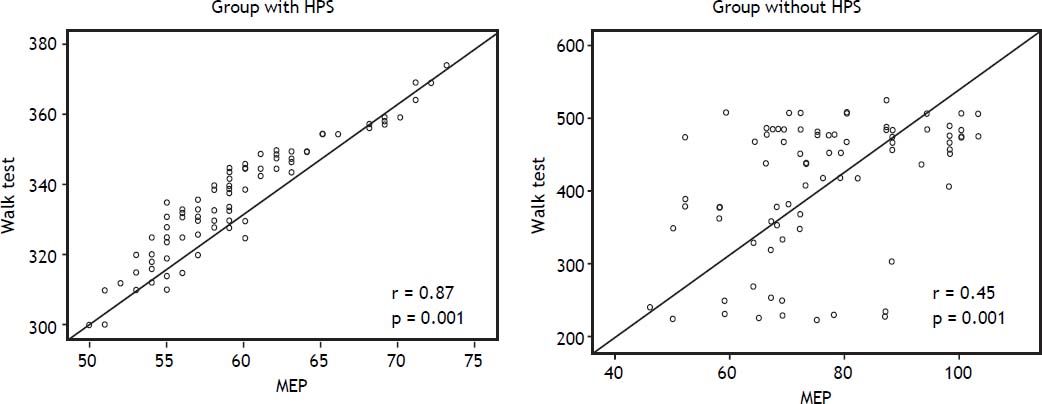
Figure 1 shows the correlation between VO2 peak and MIP in the group with HPS (r = 0.88 and p = 0.001) and in the group without HPS (r = 0.63 and p = 0.001). Figure 2 shows the correlation between 6MWT and MIP in the group with HPS (r = 0.93 and p = 0.001) and the group without HPS (r = 0.57 and p = 0.001). Figure 3 shows correlation between VO2 peak and MEP in the group with HPS (r = 0.81 and p = 0.001) and the group without HPS (r = 0.58 and p = 0.001). Figure 4 shows the correlation between 6MWT and MEP in the group with HPS (r = 0.87 and p = 0.001) and the group without HPS (r = 0.45 and p = 0.001).
This study is the first to address the impact of HPS on exercise capacity, functional condition and respiratory muscle strength in candidates for liver transplantation.
Several researchers have previously demonstrated the impact of liver disease on exercise capacity, functional condition and even respiratory muscle strength. Dharancy, et al. found that only 11.9% of candidates for liver transplantation exhibit a normal VO2 max and that patients who exhibit values lower than 60% of the predicted value had higher mortality than patients with values greater than or equal to 60% of the predicted value.21 Likewise, Galant, et al. found that individuals with alcoholic cirrhosis who exhibited a VO2 max lower than 14 mL/kg had a mortality rate of 60% in three years, while patients who exhibited a VO2 max above this value had a mortality rate of 20% over the same period.22
Regarding the functional condition measured by the 6MWT, the results also show impairment in the cirrhotic patients. Carey, et al. found that candidates for liver transplantation who walked less than 250 m in the test presented higher mortality than patients who walked more than 350 m.23 Furthermore, previous studies have demonstrated that the progress of liver disease with clinical worsening of the patients, as evidenced by the Child Pugh score, correlates with reduction in the distance walked in the 6MWT.24
Because the correlation between the distance walked in the 6MWT and VO2 peak is well described in the literature,25–27 we considered it unnecessary to search for an association between the two variables.
Although there have been no studies specifying how liver disease affects the respiratory muscles, whether through a global mechanism that involves depletion of glycogen synthesis, decreased muscle contractility with the consequent adaptation of muscle fibers and increased lactate accumulation that would damage the muscles or through refractory ascites that can impair the length/tension relationships of the diaphragm muscle, it is known that such damage occurs.28 Carvalho, et al. found that individuals with higher mortality on the LTx waiting list presented lower MIP values compared to the control group.29 In previous studies by our group, we also found that the clinical worsening of these patients is reflected in the worsening of respiratory muscle strength, and its correlation with exercise capacity and functional condition may indicate an overall muscle impairment.24
Previous studies have already demonstrated an association of functional capacity and exercise capacity with respiratory muscle strength, and these findings corroborate our findings.22,28 Regarding this association, the results obtained in this study for cirrhotic patients diagnosed with HPS were even more significant, and there are no previous data in the literature for comparison to this finding.
In seems clear that advanced liver disease contributes substantially to reducing the physical condition, which may negatively affect the quality of life of this population and consequently the survival after transplantation. However, there are no studies in the literature analyzing the influence of HPS on exercise capacity, functional condition and respiratory muscle strength. Fallon et al. compared cirrhotic patients with HPS to cirrhotic patients without HPS and, through a specific questionnaire, verified a worsened quality of life, especially regarding the aspects of overall health and lower survival rate after LTx in patients diagnosed with HPS.30
Our data suggest that HPS can affect exercise capacity and functionality through the changes in oxygenation and gas exchange, and this effect can worsen during the waiting time for LTx, which contributes to the lower survival rate of these patients reported in other studies. This result reinforces the idea that a more specific rehabilitation program needs to be developed for this population, which could help to reduce the physical inactivity and improve the results after transplantation.
The current study has several limitations, such as the lack of a second 6MWT to exclude the learning effect and a lack of other studies to better contextualize the results. However, this study’s results reinforce the need for further investigations to increase knowledge regarding the physical aspects of hepatic disease.
The cirrhotic patients with a diagnosis of HPS exhibited lower values for exercise capacity, functional condition and respiratory muscle strength than the cirrhotic patients without a diagnosis of HPS. We also found a positive correlation of the 6MWT and VO2 peak with respiratory muscle strength in the cirrhotic patients.
Abbreviations- •
6MWT: six-minute walk test.
- •
ADL: activities of daily living.
- •
AT: anaerobic threshold.
- •
CE: contrast echocardiogram.
- •
cmH2O: centimeters of water.
- •
FEV1: forced expiratory volume in one second.
- •
FVC: forced vital capacity.
- •
HCC: hepatocellular carcinoma.
- •
HCV: hepatitis C virus.
- •
HPS: hepatopulmonary syndrome.
- •
LTx: liver transplantation.
- •
MELD: Model for End Stage Liver Disease.
- •
MEP: maximum expiratory pressure.
- •
MIP: maximal inspiratory pressure.
- •
P(A-a)O2: alveolar-arterial oxygen gradient.
- •
PaO2: pressure of oxygen in arterial blood.
- •
VO2 peak: peak oxygen consumption.