Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) has emerged as an alternative for patients with bilobar colorectal liver metastasis deemed unresectable due to inadequate future remnant liver (FRL). Nevertheless, high morbidity and mortality rates have been reported. In this setting, including hepatobiliary scintigraphy in the clinical and surgical management of patients offered ALPPS has been advocated to both assess eligibility for ALPPS stagel and suitable time for ALPPS stage2. Recently, it was stated that partial ALPPS with a liver split restricted to 50% of the transection line (or up to the middle hepatic vein in case of right extended hepatectomy) and a shortened stagel allows improving the postoperative course without precluding the inter-stages FRL hypertrophy. We describe a case series of p-ALPPS with stagel performed laparoscopically, including sequential assessments of the FRL volumes and functions via pre-stagel and pre-stage2 computed tomography volumetry and HIDA SPECT-scintigraphy. In five patients, laparoscopic p-ALPPS was associated with rapid and significant gain of remnant functional volume - much better than previously observed for ALPPS - facilitating early stage2 without inflammatory adherences. In conclusion, laparoscopic p-ALPPS is feasible and seems less aggressive than the original ALPPS technique with total transection. It may be an interesting alternative to the classical portal vein embolization (PVE) and two-stage hepatectomy strategy.
In a recent pilot study,1 we first warned surgeons about the drop in total liver function in the inter-stages period of the newly-developed ALPPS technique, which was in direct connection with the reportedly-high mor-bi-mortality rates reaching up to 13%.2 This was due to a loss of function in the excluded liver that was sharper than the function gain in the future remnant liver (FRL); this latter that was + 12.5% in average [4.2%-28.6%] was further delayed and lower than the FRL volumetric gain (+42.6% [18.3%-110.2%]). Despite the “auxiliary liver” role of the excluded segments, this resulted in some degree of liver failure in the inter-stages that exposed patients to fatale liver failure following the second stage of ALPPS, especially those with complicated inter-stages in agreement with literature data.2,3 The main hypotheses for this phenomenon were:
- •
The occurrence of severe complications in the surgical site, mainly biliary fistula and/or infected peritoneal fluid, that could hinder the FRL from regenerating.2
- •
The proliferation of enlarged hepatocytes that are increased in size (explaining the FRL volume gain) but also immature and nonfunctional at the beginning of hepatocellular regeneration.4
All of these data have just been confirmed in a large multicentric study including 27 patients with systematic sequential scintigraphy (before stage1 and stage2).5
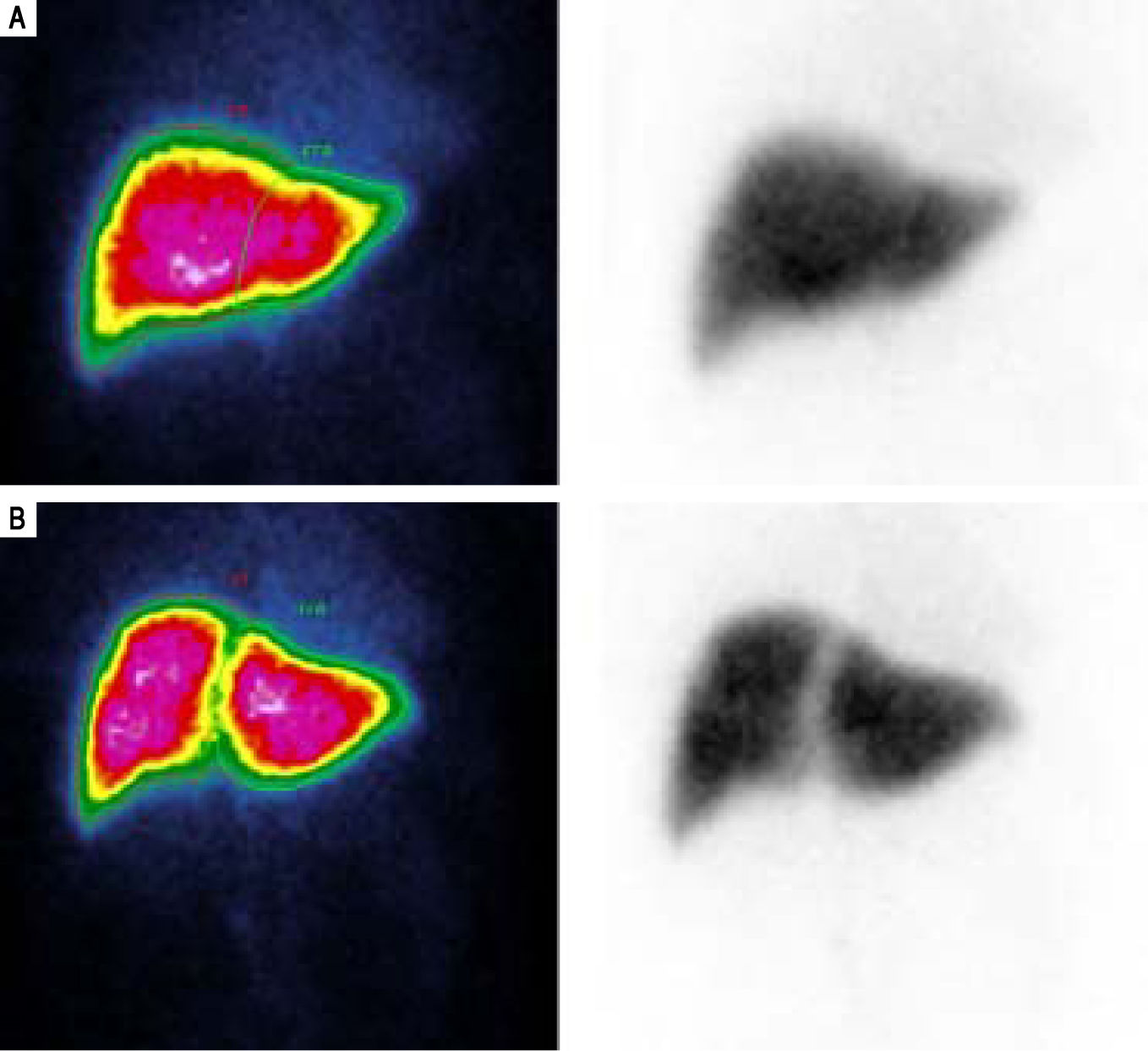
Recently, the high morbi-mortality rates of the original ALPPS technique have been significantly reduced thanks to better patient selection and many technical improvements.6,7 The main progress has come from the partial AL-PPS (p-ALPPS) technique that limits the deleterious congestion of the excluded segments and the segment IV necrosis by preserving their outflow via the middle hepatic vein, improving the postoperative outcome while achieving similar FRL rapid hypertrophy. Following such innovations and pursuing sequential scintigraphy (prestage! and pre-stage2) in our ALPPS patients, we wondered whether these technical improvements were also associated with an improved functional gain of the FRL in the inter-stages of ALPPS.
Case SeriesFive patients with colorectal liver metastases and a FRL volume deemed insufficient before a right extended hepatectomy had a p-ALPPS through a laparoscopic approach and standardized technique, consisting in:
- •
Intraoperative ligation of the right portal vein branch dissected electively (avoiding dissection of the remaining structures of the pedicle).
- •
Partial liver split along the umbilical fissure preserving the middle hepatic vein just upstream its confluence with the left hepatic vein.
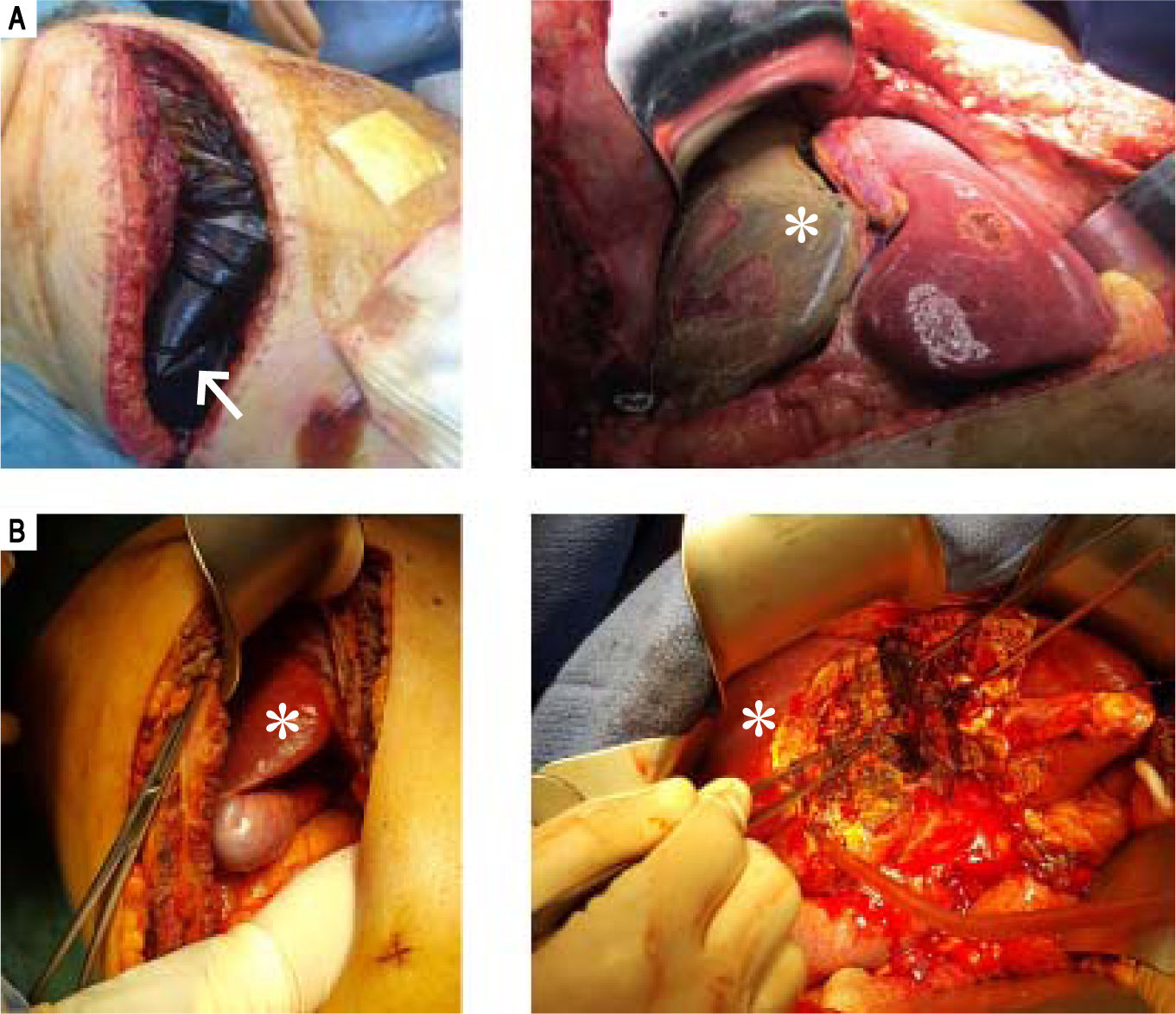
The p-ALPPS was performed upfront in 3 and as a rescue procedure after failed PVE in two at the discretion of the surgeon (Table 1). Three patients had undergone previous right colectomy for primary tumor by laparotomy (n = 2) or laparoscopy. Stagel could be performed laparoscopically in all cases, requiring in average 3 to 4 trocars to carry out - after a systematic intraoperative ultrasonography-the primary control and division of the right portal vein followed by parenchymal transection up to the middle hepatic vein using ultrasonic dissector; mobilization of the right liver was not done in order to minimize the first stage impact according to the concept of the mini-ALPPS technique,8 resulting in a short operative duration of 270 min [185395] and low blood losses of 250cc [100-500] (Table 1). In the inter-stages, no patients showed any surgical complication, in particular no bilious and/or infected peritoneal fluid was observed at laparotomy for stage2, and none met the ISGLS criteria of liver failure or MELD score above 10 - all of these factors being reportedly particularly worrying after stage1 as associated with a high risk of post-stage2 liver failure.2,3 Scintigraphy reevaluations after stage1 were carried out as previously reported4 on postoperative day (POD) 5 or 6 in all patients but one (POD12) who had partial liver split deemed less satisfactory due to severe post-colectomy adherences precluding transection up to the middle hepatic vein. We decided upfront to delay stage2 at POD14 for this latter patient who was thus discharged on POD5 after stage1. Contrasting with the above-mentioned weak functional gain of the original ALPPS technique with total transection, these 5 p-ALPPS patients showed a marked FRL functional gain ranging between + 37% and +64% (median of +47%; Figure 1). These significant FRL functional gains were not so far from the increase in FRL volume (median of +60%; ranges: + 18.6% to +108.1%), allowing performing the ALPPS stage2 early on POD 6 to 7 in all patients except the above-mentioned patient who had postponing of stage 2 onPOD13. For the latter, the volume gain was +18.6% only on POD13, but with a functional gain of +63.6% allowing stage2. In all cases, the stage2 that was done by laparotomy was facilitated by the absence of severe adhesions thanks to the laparoscopic approach for stage1 (Figure 2). Also contrasting with the original ALPPS technique, there was no necrosis of the segment IV despite complete interruption of its afferent vascular pedicles. The median stage2 operative duration was 190min [153-259] and blood losses 550cc [100-1400]. Following stage2, 2 patients showed a Clavien grade III complication (percutaneous drainage for biliary fistula and for suspicion of subphrenic biloma that was in fact sterile ascites in one patient each), while another showed biliary fistula by surgical drain with spontaneous healing. There was no liver failure or death despite a FRL function as low as 1.8%/min/m2 in 2 p-ALPPS patients, far below the cutoff of 2.7%/min/m2 advocated by the Amsterdam’s team9 as the minimum functional FRL tolerable for major liver resection but with so far no clear cut-off for ALPPS(5); these 2 patients displayed significant inter-stages function gain (> 50%) prompting us to maintain early stage2. The overall median total hospitalization time was 18 [13-25] days (7 [5-9] days for stage1 and 11 [6-18] days for stage2; Table 1).
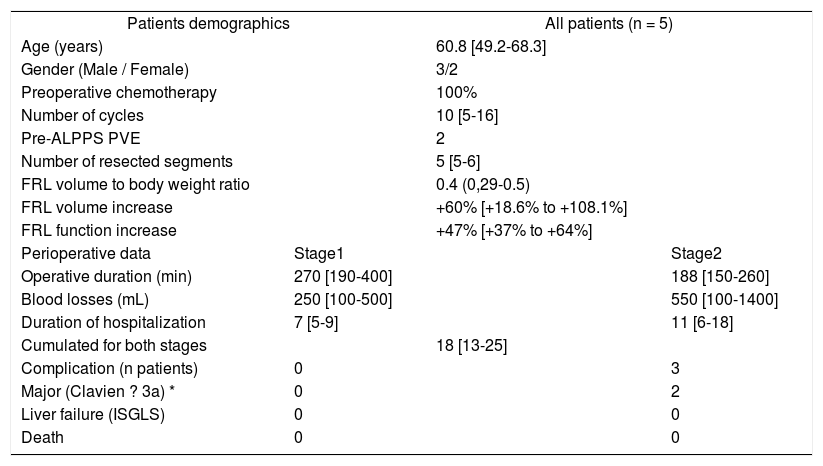
Main patients’ characteristics and perioperative data.
| Patients demographics | All patients (n = 5) | ||
| Age (years) | 60.8 [49.2-68.3] | ||
| Gender (Male / Female) | 3/2 | ||
| Preoperative chemotherapy | 100% | ||
| Number of cycles | 10 [5-16] | ||
| Pre-ALPPS PVE | 2 | ||
| Number of resected segments | 5 [5-6] | ||
| FRL volume to body weight ratio | 0.4 (0,29-0.5) | ||
| FRL volume increase | +60% [+18.6% to +108.1%] | ||
| FRL function increase | +47% [+37% to +64%] | ||
| Perioperative data | Stage1 | Stage2 | |
| Operative duration (min) | 270 [190-400] | 188 [150-260] | |
| Blood losses (mL) | 250 [100-500] | 550 [100-1400] | |
| Duration of hospitalization | 7 [5-9] | 11 [6-18] | |
| Cumulated for both stages | 18 [13-25] | ||
| Complication (n patients) | 0 | 3 | |
| Major (Clavien ? 3a) * | 0 | 2 | |
| Liver failure (ISGLS) | 0 | 0 | |
| Death | 0 | 0 | |
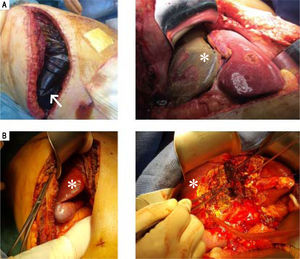
Laparotomy for stage2 of ALPPS along the umbilical fissure (A) with total parenchymal transection at the onset of ALPPS technique, showing bilious fluid within the perihepatic plastic bag (white arrow) and necrosis of the segment IV (white asterix) (B) by partial ALPPS performed laparoscopically, with no peritoneal fluid at laparotomy on POD6, no adhesion, and no necrosis of the segment IV (white asterix) despite interruption of its afferent pedicles.
Overall, this was the first time that we observed such high rates of functional gain in the inter-stages of ALPPS procedures improved as p-ALPPS with stage1 done laparoscopically. Moreover these functional gains were extremely rapid as occurring as soon as POD5 in most patients, allowing performing the stage2 on POD 6 or 7 in these cases. The main hypotheses for this beneficial effect of p-ALPPS are the low rate of inter-stages local and systemic complications thanks to a less aggressive stage1 according to the concept of “mini-ALPPS” technique8 and to preservation of the excluded segments outflow avoiding the deleterious necrosis of the segment IV and presumably a decreased cytokines and inflammatory storm. This may be especially true when the stage1 can be done during a short standardized laparoscopic procedure; by magnifying the operative view, the laparoscopic approach allowed a direct dissection to the right portal vein branch and its elective ligation (with “no touch” to the remnant pedicle); the appearance of inter-stages adhesions was limited by the laparoscopic approach itself but also by the offered possibility to perform stage2 early as a result of substantial functional gain. The main difficulty came from the challenging partial liver split along the umbilical fissure entailing a risk for iatrogenic lesion to the bile ducts of the segments II-III or IV (as previously-described for the original ALPPS technique), though potentially reduced thanks to laparoscopic magnification; moreover the avoidance of segment IV necrosis decreased the incidence of biliary leak or infected abdominal fluid. Overall, this standardized laparoscopic approach for the first step is certainly a good option for colorectal metastases indication, but it may also have an increasing role in the treatment of hepatocellular carcinoma.10 The choice for a laparoscopic approach with portal vein branch ligation and limited transection, leading to a less morbid stage1, may also open the concept and key-research of a new equilibrium between inflammatory and growth factors enhancing or limiting liver regeneration. These data have now to be confirmed in larger series of modified ALPPS procedures, as well as the potential oncological benefit of these less complicated procedures with probably lower immunosuppressive effect. In the future, the respective role of p-ALPPS vs. PVE (or double embolization of the ipsilateral portal and hepatic vein) in patients scheduled for extended hepatectomy will have to be determined.
Abbreviations- •
ALPPS: Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy.
- •
FRL: future remnant liver.
- •
p-ALPPS: partial ALPPS.
- •
POD: postoperative day.
- •
PVE: portal vein embolization.
- •
SPECT: single photon emission computed tomography.
The authors declares that there is no conflict of interest regarding the publication of this article.
Authors’ ContributionConception and design: Truant S, Baillet C, Lecolle K. Analysis and interpretation: Baillet C, Huglo D, Ernst O. Data collection: Lecolle K, El Amrani M, Ploquin A, Ernst O. Writing the article: Truant S, Ploquin A, Pruvot FR. Critical revision of the article and obtaining funding: Pruvot FR, Hebbar M.
Financial DisclosuresNone.