Hepatic artery thrombosis (HAT) is relatively infrequent, but possibly a devastating complication of orthotopic liver transplantation (OLT). It often requires urgent retransplantation. Two main forms of HAT are recognized as early and late HAT (diagnosis within or after 30 days following LT). Early HAT typically results in graft failure. Late HAT features biliary obstruction, cholangitis, and hepatic abscess formation. We report here the case of a patient of Wilson’s disease who presented twelve years post-liver transplant symptoms typical of acute HAT and hepatic infarction. On diagnostic imaging, celiac axis and hepatic artery were thrombosed, resulting in ischemic necrosis of the left hepatic lobe. The resulting sepsis and transient hepatic insufficiency were managed conservatively, and repeat OLT was avoided. The patient remains stable more than one year later. To the best of our knowledge this case report is unique in the literature for the unusually long interval between OLT and late acute HAT, as well as celiac and portal vein occlusion. The acute presentation of sub massive hepatic necrosis is also uncharacteristic of late HAT and more typical of acute HAT. This report describes our experience in managing this and a literature review of the topic.
Hepatic artery thrombosis (HAT) is the most common vascular complication after liver transplantation.1 It often causes irreversible damage to the liver and represents one of the major causes of graft loss and liver transplant recipient mortality. The time point that divides early and late HAT is somewhat arbitrary and has not been agreed on but most authors consider late HAT to occur more than 4 weeks post orthotopic liver transplantation (OLT). The incidence of HAT after liver transplantation varies widely, with a reported incidence of 2.5-9%2 in adult recipients and 10-25% in the pediatric population.3 It comprises 60% of all post transplant vascular complications.4 Late HAT is usually less common than early HAT.3 However, in some centers, it was reported more commonly.5 HAT carries a mortality rate of 27% to 58%3.The mortality rate may increases to 73% if re-OLT is not performed.3 Late HAT shows lower mortality rates than early HAT. Graft failure leading to re-transplantation rate can be overall 50-80%.2,6
Most studies of late HAT in the literature report the diagnosis made within the first year post OLT, In a recent series, the median time of presentation was 6 months (range, 1.8 to 79 months) after OLT.3 Where early HAT may present with an acute fulminant clinical course, late HAT has a more insidious one and can be asymptomatic or produce initially minimal biochemical abnormalities, which can delay the time of the diagnosis.
We report here the case of an acute presentation of acute thrombosis of the celiac axis, hepatic artery (HAT) and portal vein featuring sub massive hepatic infarction and necrosis of the left lobe of the liver, 12 years following OLT. The longest previous interval reported in the literature for late HAT was 79 months.3 Our case is therefore unique and is the longest interval between OLT and presentation of late HAT, ever reported in the literature. This case is also unique because of the acute features of hepatic infarction and necrosis, which are classic for acute HAT but uncharacteristic of late HAT.
Case ReportA 34-year-old man had an initial deceased donor liver transplant in 1995 for acute Wilson’s disease. Although donor was ABO compatible but was not identical (Recipient B, Rh positive, Donor O, Rh positive). The patient was seronegative for cytomegalovirus (CMV) IgG, hepatitis A virus (HAV) IgM, hepatitis B virus (HBV) surface antigen (sAg), and hepatitis C virus (HCV) antibody. There were no extra hepatic Wilson’s features. His transplant was complicated by diffuse intrahepatic biliary strictures on the basis of chronic rejection, which was confirmed on percutaneous liver biopsy. He suffered from repeated and recurrent episodes of bacterial cholangitis until he received a second orthotopic deceased donor liver transplant in 1996. The surgical reconstruction was a biliary duct-to-duct anastomosis with a T-tube and the hepatic arterial reconstruction involved a Carrel patch that incorporated the splenic artery. There was no ABO and CMV mismatch. UW (University of Wisconsin) solution was used for preservation.
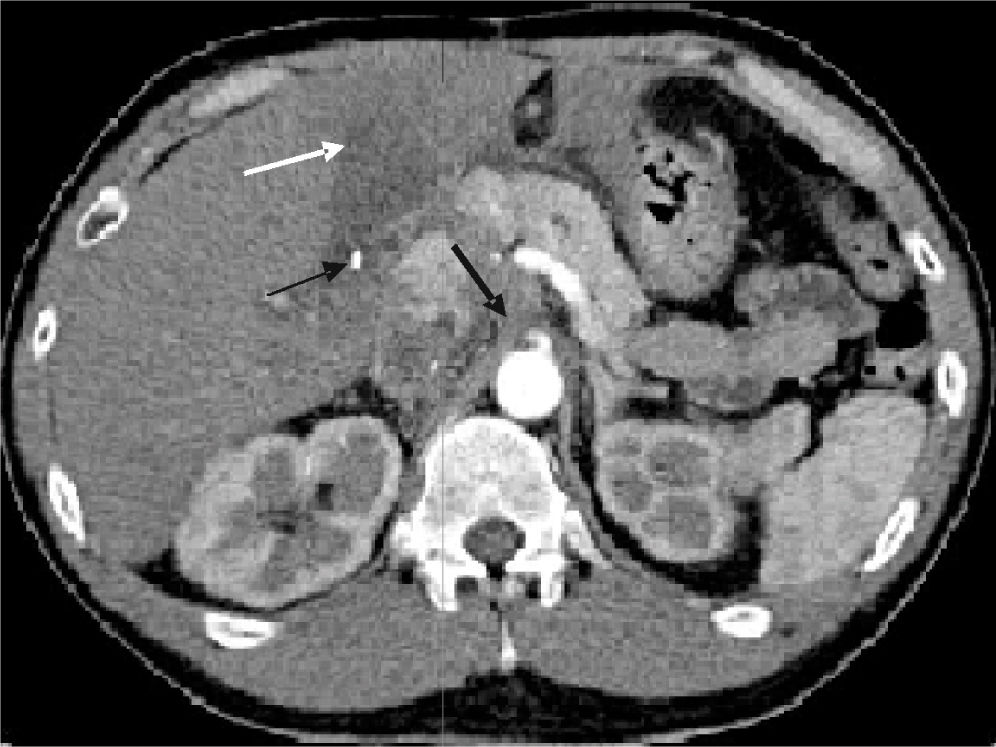
Apart from mild chronic renal insufficiency for which the immunosuppressant maintenance regimen consisted of MMF monotherapy, the patient was clinically stable with normal liver biochemistry. In 2008, exactly 12 years and one month after his second transplant, he presented to the Emergency Department with a short history of vague, mild epigastric pain, nausea, vomiting and high fever of 39 C. His initial laboratory investigations revealed an ALT of 1486 (laboratory normal < 80 U/L), AST 990 (normal < 65 U/L), total bilirubin 16 μmol/L (normal < than 22 amol/L), and an albumin of 34 g/L (normal 35-45 g/L). Serial blood cultures within the first 24 hours of admission were positive for enterococcus faecalis. An abdominal ultrasound showed a heterogeneous left lobe with a complex fluid collection measuring 4.9 X 3.9 X 1.0 cm and on doppler study; the hepatic artery could not be visualized. There was no evidence of intra or extra hepatic biliary dilatation seen. Late acute hepatic artery thrombosis was confirmed by subsequent CT scan (Figure 1), which revealed thrombosis of the celiac axis just distal to its origin and hepatic artery. There was also extensive thrombus within the native IVC and left renal vein. Large areas of the left lobe of the liver were shown to be infarcted. Treatment consisted of long term antibiotics (vancomycin followed by ampicillin for one year’s duration) were continued along with anticoagulation. Hematologic hypercoagulopathy investigations were negative. Family history for thrombotic episodes was non-contributory. Patient was a lifelong non-smoker. No history of CMV viremia observed. His one-year follow-up blood test shows white cell count S.O. AST 37 U/L, ALT 49 U/L, alkaline phosphatase 168 U/L, GGT 78 U/L, total bilirubin 9 μmol/L.
Contrast enhanced CT through the upper abdomen in the arterial phase following contrast injection showing occlusion of the celiac axis immediately distal to its origin (thick arrow), and occlusion of the hepatic artery. Area of low density in the left lobe of the liver compatible with area of infarction (white arrow). A surgical clip is present at the hepatic hilum (thin arrow).
He is clinically asymptomatic after more than one year of follow up and his US shows post-necrotic changes that remain stable, of the left lobe of the liver.
DiscussionHepatic artery thrombosis (HAT) after orthotopic liver transplantation (OLT) is a well-known and potentially life threatening complication. Early HAT is characterized by an acute severe clinical course. In contrast, in the rare case of late HAT, the presentation is usually associated with a milder clinical course and is often an incidental finding. Early vs. late HAT differ with regard to contributing factors and treatment plans.
In the non-transplant setting, the native human liver usually tolerates HAT, or even acute ligation well because of its abundant collateral arterial sources, which preserve it from ischemia. Total hepatectomy at OLT disrupts these collaterals; however, the allograft may survive on portal flow only while arterial collaterals develop. Collateral arterial flows to the graft are absent in the first weeks after OLT. The occlusion of the hepatic artery during this time period can produce irreversible ischemic damage to the liver, leading to hepatic necrosis and failure. Usual collaterals that may develop late after OLT are through peridiaphragmatic vessels7 or through the Roux limb in case of choledochojejunostomy.8 Unlike in a native non-transplanted liver, the bile ducts in a liver transplant, are dependent purely on the arterial blood supply from the hepatic artery. Biliary duct ischemia caused by decreased or absent hepatic artery flow can lead to focal areas of intrahepatic biliary dilatation separated by focal strictures and biliary sludge. Thus careful radiologic evaluation of hepatic arterial flow is necessary in the case of anatomical biliary abnormalities seen in liver transplant patients.
Early HAT may be associated with technical or nontechnical risk factors. Technical risk factors include aberrant allograft anatomy, a small caliber hepatic artery, multiple arterial anastomoses, anastamotic technique, use of an interposition graft with aortic implantation,2 biliary reconstruction by hepaticojejunostomy,9 biliary anastamotic leaks and arcuate ligament syndrome. Nontechnical risk factors10 attributed in different case series are previous OLT, high intraoperative transfusion requirements for packed red blood cells (pRBC) or fresh frozen plasma (FFP), infection, hypercoagulable states, or acute rejection), cytomegalovirus (CMV)-positive donor with CMV-negative recipient(CMV mismatch),11 cigarette smoking,12 and one or more episodes of acute rejection.
The presentation of early HAT is that of rising serum transaminase levels, fever, bacteremia possible graft failure, and may involve disintegration of the biliary anastomosis. The diagnosis is usually made by Doppler US or CT angiography. Doppler US carries a sensitivity approaching 100% for early HAT however, it becomes less sensitive as the interval between transplantation and diagnosis of hepatic artery thrombosis increases due to collateral arterial flow.13 Rarely, early HAT can be effectively managed by catheter-directed thrombolysis, or surgical embolectomy and revision of the arterial anastamosis5 but more commonly, urgent retransplantation is required usually (reOLT). Despite refinements of operative technique over the past two decades that have seen a significant reduction in the incidence of early HAT, the mortality rate still remains significant (50%).3
Risk factors for late HAT is not always identifiable and they may include multiple episodes of acute rejection, chronic rejection, cigarette smoking, postoperative CMV hepatitis3,11 and hepatitis C virus (HCV) reinfection of the allograft. The presentation of late HAT typically follows a more benign course and often does not require retransplantation. It usually involves the onset of biochemical and clinical features of ischemic injury to the biliary tree many weeks or months post OLT, with progressive biliary strictures and obstruction, episodes of cholangitis, and hepatic abscess formation. Late HAT is preceded in some cases by progressive hepatic artery intimal hyperplasia and the development of arterial collaterals that compensate for late HAT when it finally occurs. Rarely, the presentation of late HAT may be acute. The clinical course of late HAT is reportedly less morbid than that of early HAT, and can in some cases be managed conservatively. Bhattacharya, et al.14 reported a total of 33% survival of late HAT in the long-term without a second transplant. Treatment modalities can vary from surveillance with long-term antibiotics to interventional radiological or surgical modalities like recombinant plasminogen lysis with hepaticojejunostomy, surgical thrombectomy.2 Therapy of liver abscess may require antibiotics, abscess drainage, or partial hepatectomy.15 Biliary tract complications can be successfully treated long term endoscopically by internal drainage or subsequent hepaticojejunostomy.14
Our patient’s clinical presentation was identical to that of typical acute early HAT except that liver transplantation occurred 12 years previously and is the longest post-transplant case to ever have been reported. In our patient’s situation, HAT of the left hepatic artery was associated with co-incidental thrombosis of the celiac axis, left portal vein and portal vein. Although the etiology remains elusive, we suspect that it was multifactorial: possible volume depletion (the episode occurred in the summer), possible acute viral/bacterial infection (non-specific gastrointestinal symptoms) in combination with a possible primary hypercoagulable condition that remains undiagnosed. Our experience suggests that acute HAT with or without other acute vascular abnormalities must always be considered in any liver transplant recipient with a similar presentation no matter how many post-transplant years may have passed. Collateral circulation may not be adequate despite the fact that many years may have passed after transplant surgery.