Background. Intestinal intussusception in adults is associated with chronic inflammatory bowel disease, coeliac disease, abdominal tumors or previous abdominal surgery but most often of unknown origin.
Aim. The aim of our study was to evaluate circumstances and identify risk factors for intussusceptions.
Methods. All 65,928 abdominal ultrasound examinations performed at our tertiary medical center between January 2001 and June 2008 were analyzed retrospectively for the diagnosis “intussusception”. After identifying individuals with sonographically proven intussusception we analyzed various patients’ characteristics including age, gender and underlying disease as well as sonographic findings such as localization of the intussusception, absence or presence of ascites and lymph nodes.
Results. We identified 32 cases of intussusceptions [mean age 45 years (range 18 to 88); 18 patients were male]. Twelve patients (38%) had a history of abdominal surgery including 8 patients who had undergone liver transplantation (2 patients with primary sclerosing cholangitis, 1 patient with cystic fibrosis, 1 patient with sarcoidosis, 1 patient with hepatocellular carcinoma and HCV infection, 1 patient with autoimmune hepatitis, 1 patient with Crigler-Najar-syndrome and one patient with echinococcus). A hepaticojejunostomy had been performed in 4 of the patients after liver transplantation. Liver transplanted patients were significantly overrepresented in the intussusception group compared with the overall cohort of patients undergoing abdominal ultrasound examination (25% vs. 8%, Chi-Square-test, p = 0.0023).
Conclusion. In our retrospective study liver transplantation, in particular with hepaticojejunostomy, was identified as a new major risk factor for intestinal intussusceptions.
Intestinal intussusception in adults as a cause of abdominal pain has been found in 0.53% of cases in a prospective study by Maconi, et al.1 Intestinal intussusception is frequently considered to being of idiopathic origin, In addition it has been associated with chronic inflammatory bowel disease, Meckel diverticula, prior abdominal surgery and gastrointestinal tumors.1-5 In children as well as in adults various infectious causes for intestinal intussusceptions have also been described. Adenoviruses, enteral tuberculosis, rotaviruses, Clostridium difficile infection or Yersiniosis6-11 have been associated with intussusceptions. Also vaccination against rotaviruses was associated with intestinal intussusception.9 Interestingly, biliary infection with adenoviruses is a typical reason for intussusceptions in childhood,6,12,13 but seems not important for intussusceptions in adults.
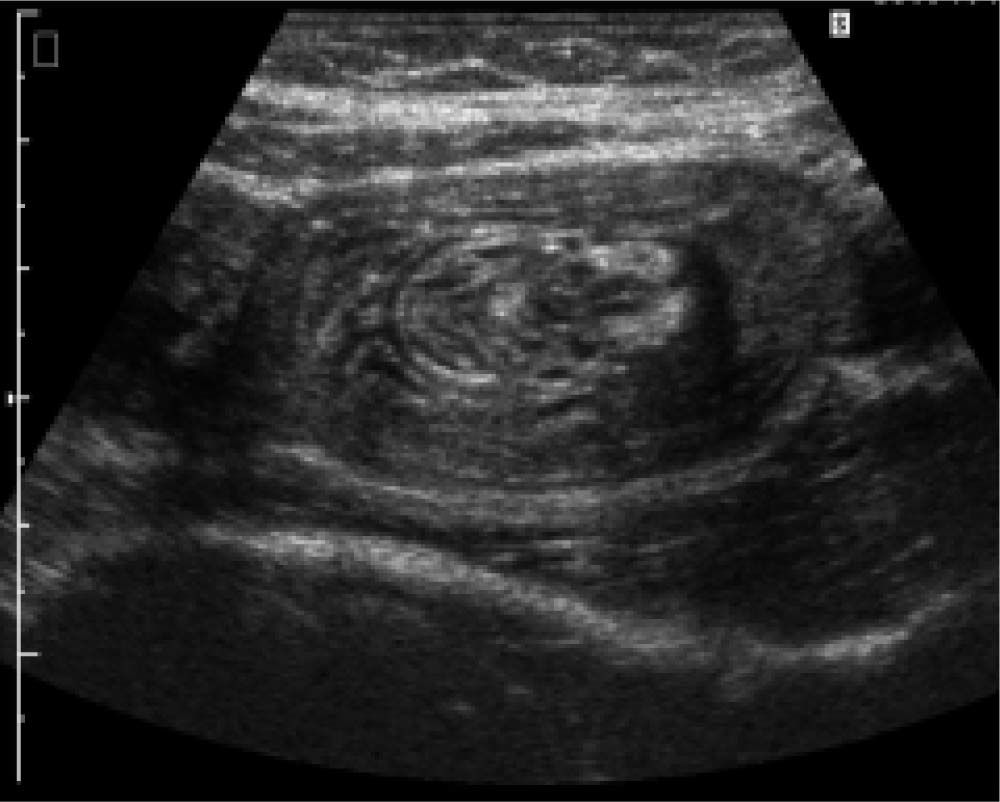
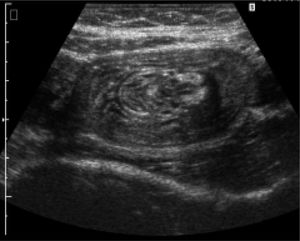
Most previous studies investigating risk factors for intestinal intussusceptions have been focused on surgical aspects of therapy.14,15 Studies analyzing the diagnostic use of ultrasound examinations are rare. A study of 41 cases of intussusception evaluated CT scans as the diagnostic gold standard for intestinal intussusception.16 However, in Europe ultrasound is regarded as the diagnostic tool of choice1 (Figure 1). Prerequisites for the reliable diagnosis of intussusceptions by ultrasound are that high-frequency-sonography probes with < 6 MHZ are used and that an experienced physician is performing the examination (e.g. DEGUM certificate Grad II).17 These prerequisites are based on the recommendations of the DEGUM, the German Society for Ultrasound in Medicine (www.degum.de).
In a recent case report we described the case of a liver transplanted patient with repeated intussusceptions in context of intestinal CMV-infection.18 However, the risk for liver transplanted patients to develop intussusceptions has never been examined systematically. Here, we examined the characteristics of patients with sonographically diagnosed intussusception in a retrospective analysis.
ObjectiveThe aim of our study was to identify risk factors associated with intestinal intussusception in adults.
Patients and MethodsThe study was performed at Hannover Medical School, a tertiary center with a large transplantation program, performing more than 140 liver transplantations per year over the last decade.19 Our liver transplant outpatient clinic follows nearly 2,000 liver transplanted patients. The section for ultrasound within the Department of Gastroenterology, Hepatology and Endocrinology at Hannover Medical School is a highly specialized unit performing around 8,000 ultrasound examinations each year.
For our analysis we searched a database of ultrasound examination reports for the term “intussusception” including every ultrasound examination report between January 1, 2001 and June 30, 2009. A total of 65,928 ultrasound examinations were investigated. Only cases with sonographically documented intussusception were included in this study. Required sonographic criteria for intussusception were:
- •
A multilayered lesion with concentric circles (onion sign) in the transversal plane.
- •
In case of involvement of the mesentery an echo-rich crescent open towards the ante-mesenteric side (donut sign).
- •
An echo-rich layer between two multilayered structures (the sandwich sign) in the longitudinal plane.20
Suspicious cases of intussusception without adequate sonographic proof of the disorder were excluded (n = 11).
For all patients with intussusceptions, the following characteristics were analyzed: age, gender, underlying disease, localization of intussusception, history and type of former abdominal surgery and/or former liver transplantation, the presence of ascites and enlarged intra-abdominal lymph nodes.
In total, 5,257 ultrasound examinations (~ 8%) were performed on patients after liver transplantation.19 In most of them liver transplantation included duct-to-duct biliary reconstruction, while approximately 8% of all liver transplanted patients had a primary hepaticojejunostomy due to primary sclerosing cholangitis (PSC). 3% of liver transplant recipients received a secondary hepaticojejunostomy due to bile duct stenosis. Overall, 11% of all liver transplanted patients at Hannover Medical School received a hepaticojejunostomy. In our study cohort we focussed on ultrasound records of the 982 examinations (1.5%) that have been performed on patients with a history of hepaticojejunostomy. 572 examinations (0.9%) were in patients with Whipple Operation, 538 (0.8%) in patients with a history of colonic resection and 295 (0.4%) in patients with gastrectomy.
Statistical analysis was performed by Chi-Square-test. A p-value of > 0.05 was considered to be statistically significant.
ResultsOf the 65,928 ultrasound examinations we identified 32 patients with sonographically proven intussusceptions. This represents 0.05% of all ultrasound examinations.
The mean age of the patients with intussusception was 45 years (range 18 to 88 years) and 18 patients were male. In 13 patients the intussusception was located at the ileocoecal region (41%). Six patients had multiple intussusceptions at more than one location (19%), four of these six patients also had enlarged lymph nodes. Two cases had the intussusception directly at the ileocoecal valve.
In the majority of patients with intussusception (22/32, 69%) enlarged abdominal lymph nodes could be identified.15 of them were located in the mesenterium (47%) and 9 at the hepatoduodenal ligament (28%). Two patients had enlarged lymph nodes at both locations and one had enlarged lymph nodes at the ligamentum hepatoduodenale as well as along the abdominal part of the aorta.
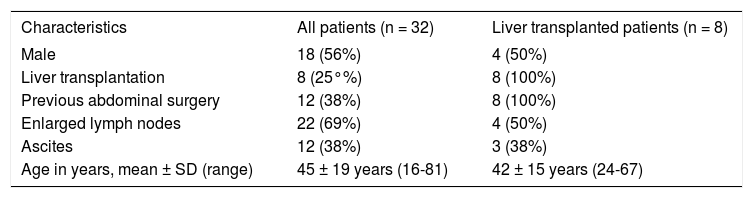
There was no statistically significant gender difference with regard to intestinal intussusceptions in our cohort. Eighteen male and 14 female patients presented with intussusceptions. Both sexes were represented evenly in our group of liver transplanted patients which included 4 men and 4 women (Table 1).
Characteristics of 32 patients with ultrasound-proven intussusception.
| Characteristics | All patients (n = 32) | Liver transplanted patients (n = 8) |
|---|---|---|
| Male | 18 (56%) | 4 (50%) |
| Liver transplantation | 8 (25°%) | 8 (100%) |
| Previous abdominal surgery | 12 (38%) | 8 (100%) |
| Enlarged lymph nodes | 22 (69%) | 4 (50%) |
| Ascites | 12 (38%) | 3 (38%) |
| Age in years, mean ± SD (range) | 45 ± 19 years (16-81) | 42 ± 15 years (24-67) |
In twelve patients with intussusception (38%) ultrasound examination revealed ascites, predominantly located between parts of the colon (n = 10) but also diffusely distributed in the whole abdomen (n = 1) and perihepatically (n = 1).The patient with perihepatic ascites presented with sarcoma and pleural carcinomatosis.
Seven patients had neither detectable lymph nodes nor ascites. Four of these had been liver transplanted, two had Crohn’s disease and one patient had acute pancreatitis. Three of the four liver transplanted patients had no history of hepaticojejunostomy, the remaining patient had a primary hepaticojejunostomy due to the preexisting PSC.
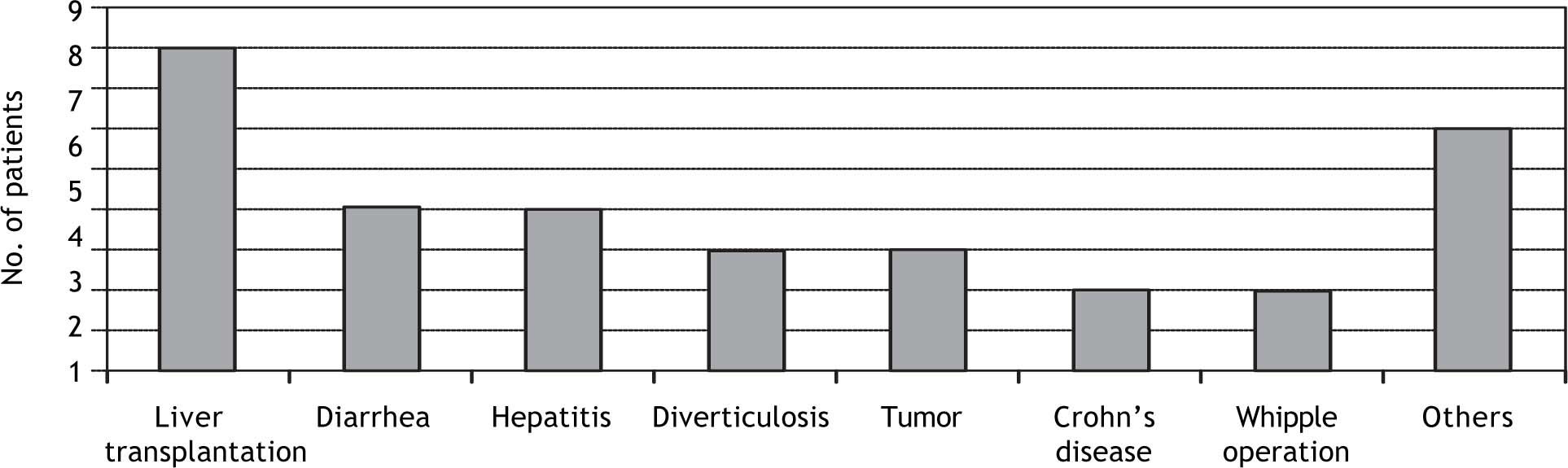
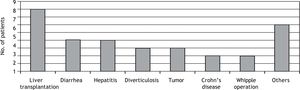
Patients with intussusception had different underlying diseases and previous surgical interventions as shown in figure 2.
Eight of them were liver transplanted patients (25%). The age range in the group of liver transplanted patients with intussusception was 22 and 58 years (mean 36 years).
Four patients had repeated episodes of diarrhea, three also showed signs of sigmadiverticulosis and two patients each have been diagnosed with Crohn’s disease, hepatitis of unknown origin, chronic Hepatitis C Virus (HCV) infections or previous Whipple operations. There were single cases with pancreatitis, primary sclerosing cholangitis (PSC), meteorism, hepatocellular carcinoma (HCC), anemia of unknown origin, sarcoma, previous lung transplantation and suspicion of pancreatic cancer.
In relation to the percentage of liver transplanted patients who underwent ultrasound examination (8%) the percentage of those with proven intussusception was higher (25%) suggesting that liver transplantation might be a new risk factor for intestinal intussusception (p = 0.002). 4 of these 8 patients were patients with a hepaticojejunostomy (50%).
The frequency of patients with previous Whipple operation and proven intussusception compared with frequency of patients with intussusceptions in the whole study collective was not significant in Chi-Square-test (p = 0.177). Even the comparison with the total cohort of patients with gastrectomy or colonic resection was not significant in Chi-Square-test (p = 0.705 and p = 0.609).
DiscussionAnalysing at total of < 65.000 ultrasound examinations at our department, sonographic evidence of intestinal intussusception was found in only 0.05% of all ultrasound investigations. Interestingly, a recent Italian study by Maconi, et al., found that intussusceptions were more frequent in that cohort.1 However, the Italian cohort differed significantly from ours since it included only patients presenting with abdominal pain and it was a prospective study with examinators focused on intussusceptions. Our study in contrary included retrospectively all abdominal ultrasound examinations independent of the clinical indication (Figure 1).
It is well known that intestinal intussusception in adults is a rare disorder in the general population. It becomes a more frequent diagnosis if the cohort is narrowed to patients with abdominal pain. It has also been shown that intussusceptions are more common in HIV-infected patients21 and patients with intestinal Karposi-sarcoma,22,23 Burkitt-Lymphoma24 or infections.25 Patients with a history of abdominal operations are at an increased risk for intussusceptions. Recently, we described a case of a liver transplanted patient with repeated intussusceptions in context of an intestinal CMV-infection.18 In the present study we could identify liver transplantation as a potential risk factor for intestinal intussusception. 25% of patients with intussusception were liver transplant recipients in our series.
Possible mechanisms causative for this correlation could be exposition to the immunosuppressive drugs or the prior abdominal surgery. While in previous studies intestinal intussusception in adults is predominantly linked to benign or malign tumors,3,16,26 in our study patients with tumor were the minority. A possible explanation for this discrepancy might be that while most other studies focussed on clinically severe cases of intussusception with subsequent surgery, the present study included all sonographically proven intussusceptions with and without clinical symptoms.
The frequent presence of enlarged lymph nodes and ascites can be explained as symptom of an underlying enteric infection. This was described previously for mesenterial lymph nodes in children with transient intussusceptions in the context of gastroenteritis.27 In addition to infectious causes, mechanic or inflammatory processes might also lead to intussusception.5,14,15,25
Patients with former gastrectomy or colonic resection were not overrepresented in our group of intussusceptions. This could be explained by the rather special study population, recruited at Hannover Medical School, a tertiary transplant center.
From the analysis of our cohort, hepaticojejunostomy seems to be another risk factor for intussusception. This surgical procedure was more frequent, but needs to be confirmed in future prospective studies.
Obviously, our study has several limitations. First, the number of patients identified with an intussusception was still relatively small. Second, the retrospective design of our study needs to be considered. Third, no complete data set for all parameters analyzed was available for each single individual and the control cohort which did not allow us to perform a better designed case-control study. Thus, future studies should aim to prospectively investigate the frequency of intussusseceptions in liver transplant patients in general and especially in those with hepaticojejunostomy.
ConclusionIn summary, we suggest for the first time that previous liver transplantation is a special risk factor for intussusceptions, in particular when a hepaticojejunostomy has been performed. The frequently found enlarged lymph nodes in patients with intussusception indicate the possible role of intussusception triggered by infection, especially in immunosuppressed patients like liver transplant recipients.