Background. The epidemiology and clinical characteristics of nonalcoholic fatty liver disease (NAFLD) in South America are not well known. Brazil is a largest country in this part of the world and the present study aimed to contribute with this information.
Methods. This descriptive study included patients from medical centers around Brazil, who had diagnosis of NAFLD. They were selected from chart review and also prospectively in Hepatology out-clinics. Patients with history of alcohol intake and others liver diseases were excluded. Histological diagnosis included: steatosis or steatohepatitis (steatosis, ballooning of hepatocytes or fibrosis). The criteria to perform a liver biopsy was ALT or AST > 1.5 × normal levels.
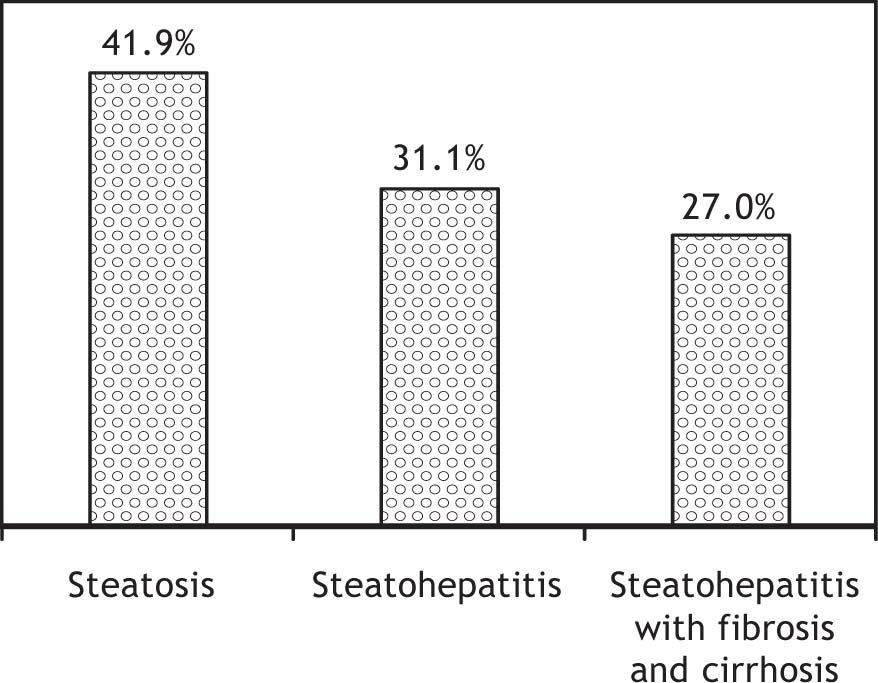
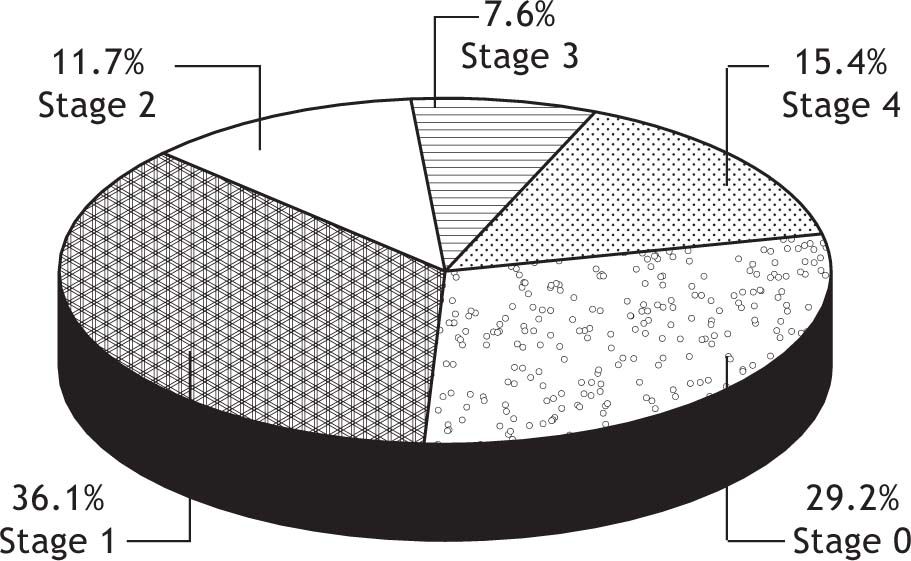
Results. A total of 1280 patients from 16 Brazilian centers and all five regions were included. The mean age was 49.68 ± 13.59 years; 53.3% were males and 85% were asymptomatic. Hyperlipidemia was observed in 66.8% cases, obesity in 44.7%, overweight in 44.4%, diabetes in 22.7%, and toxins exposure in 10%. Metabolic syndrome was observed in 41.3% cases. Elevated levels of ALT, AST and GGT were observed in 55.8%, 42.2% and 63.1% cases, respectively. Liver biopsy performed in 437 cases showed: isolate steatosis in 42% cases, steatohepatitis in 58% and 27% of them also presented fibrosis. Cirrhosis was observed in 15.4% and hepatocellular carcinoma in 0.7%.
Conclusions. NAFLD in Brazil is more frequent in asymptomatic males; steatohepatitis with fibrosis and cirrhosis were a significant diagnosis. The genetic predisposition and lifestyle should be influenced in the spectrum; however these findings deserve a future investigation.
Nonalcoholic fatty liver disease (NAFLD) may affect any age, ethnic group or country. The prevalence estimated of NAFLD in the general population ranges from 3 to 24%.1,2 This liver disease appears to be most strongly associated with obesity and insulin resistance states including diabetes and with other features of the metabolic syndrome, such as high triglycerides and low HDL. It appears to be more common in men, and it increases with increasing age and after menopause in women. More advanced stages of NAFLD are associated with older age, higher body mass index, diabetes, hypertension, high triglycerides, and/or insulin resistance.3,4
The high frequency of NAFLD was described in Mexican Americans when it was compared with African Americans and non-Hispanic Caucasian.5 The higher incidence of metabolic syndrome also has been described in Amerindian populations,2 and it may suggest that NAFLD also is common throughout Latin America.
This high prevalence of NAFLD, however, is not exclusive to the Caucasian western population. NAFLD among healthy Japanese adults has reached epidemic proportions in different populations around the world.6 In the South Asian Indian some studies have shown that this population also is at high risk for development of metabolic syndrome, type 2 diabetes and cardiovascular disease, suggesting the possibility of gene variants that impact shared molecular pathways amongst these clinic entities.7,8
In Brazil, over the last two decades, changes in human behavior and lifestyle have resulted in a dramatic increase in the prevalence of obesity. According the last Census by Brazilian Institute of Geography 40% of Brazilian adult population is overweight and 8.9% males and 13% of females were obese.9,10
ObjectiveThe present study aimed to describe the clinical and histological aspects of NAFLD in Brazil and to contribute with information about characteristics of NAFLD in this part of South America.
Patients and MethodsStudy design and patients selectionThis descriptive study included patients with NAFLD diagnosis from the five regions and sixteen centers around Brazil. They came from states of South (Rio Grande do Sul and Paraná), North (Pará), Northeast (Paraiba, Pernambuco and Bahia), Southeast (Säo Paulo, Rio de Janeiro e Minas Gerais) and Center (Federal District-Brasilia). The patients were selected from chart review and prospectively from hepatology out-clinics.
The study was approved by the Ethics Committee for Medical Research-Programa de Pós Graduaçâo em Medicina e Saúde-Universidade Federal da Bahia, Brazil and in all centers that the patients were included.
NAFLD criteriaPatients were included when they presented the following criteria: presence of steatosis on abdominal ultrasound and alterations of hepatic enzymes (ALT/ALT); history of alcohol intake ≤ 20 g/day; exclusion of others liver diseases (B and C virus infection, haemochromatosis, Wilson’s disease and autoimmune hepatitis).
The pattern of alcohol consumption was obtained from medical consultations with physicians and inter-views with patient relatives.
Patients evaluationA questionnaire was used to obtain medical history, demographic data, to evaluate alcohol consumption, and the use of medications. Data of physical exam, laboratory tests and abdominal ultrasound were included.
- •
Anthropometry. Body mass index (BMI) was calculated as body weight (kg)/height (m2) and patients were categorized as normal weight (< 25.0 kg/m2), overweight (≥ 25.0 and ≤ 29.9 kg/ m2) and obese (≥ 30.0 kg/m2). The obesity was classified in grade I (30.0-34.9 kg/m2), grade II (35.0-39.9 kg/m2) and grade III (≥ 40.0 kg/ m2).11
- •
Laboratory tests. ALT, AST, GGT, fasting glucose, insulin, and a lipid profile (triglycerides, total cholesterol, HDL-C (high-density lipoprotein), LDL-C (low-density lipoprotein), serological tests for hepatitis B and C, ferritin and transferin saturation.
Insulin resistance (IR) was evaluated by calculating the Homeostasis Model Assessment of Insulin Resistance (HOMA-IR).12 To apply HOMA-IR to the insulin resistance index, HOMA-IR ≥ 3 was used.13
Metabolic syndrome was evaluated in all cases and defined as ATP III criteria.14
Liver biopsy and histological diagnosisCriteria for liver biopsy included serum ALT/AST determinations greater than 1.5 the normal level in more than two occasions, separate by at least 1 month.
Liver tissue was fixed in 4% formol saline, processed in an auto-technicon apparatus and stained with hematoxylin-eosin (HE) and Masson’s trichrome. The following histological variables were analyzed: macro-and microvacuolar fatty change, zonal distribution, foci of necrosis, portal and perivenular fibrosis, and inflammatory and fibrotic infiltrate with zonal distribution. All specimens were scored by a liver pathologist with expertise in NAFLD.
A preview protocol to histological diagnosis was done and sent for all Brazilian pathologists, and the participant’s centers have used the same histological score.
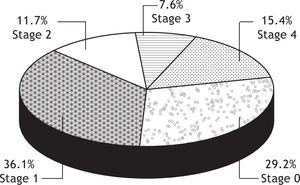
The patients were classified as having steatosis; steatohepatitis (steatosis, ballooning of hepatocytes, and inflammatory infiltrated with or without fibrosis). Fibrosis was classified into 5 stages:
- •
S 0: Without fibrosis.
- •
S 1: Fibrosis limited to the perivenular or per sinusoidal area in zone 3.
- •
S 2: Perivenular and per sinusoidal fibrosis with portal fibrosis.
- •
S 3: Bridging fibrosis.
- •
S 4: Cirrhosis.15
- •
Statistical analysis. The Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA, and Release 16.0.2, 2008) and Prism (Graph Pad Inc., San Diego, CA, USA, Release 5.01) software program, version 12.0, was used to analyze the data in this study.
The study included 1280 patients with diagnosis of NAFLD around Brazil. The mean age of the patients was 49.68 ± 13.59 years, 53.3% were males and 85% were asymptomatic. The evaluation of the risk factors showed: hyperlipidemia in 66.8% cases, obesity in 44.7%, overweight in 44.4% and diabetes in 22.7%. Toxins exposure was related for 10% of the cases. Metabolic Syndrome was observed in 41.3% cases.
Elevated levels of ALT, AST and GGT were observed in 55.8%, 42.2% and 63.1% cases, respectively.
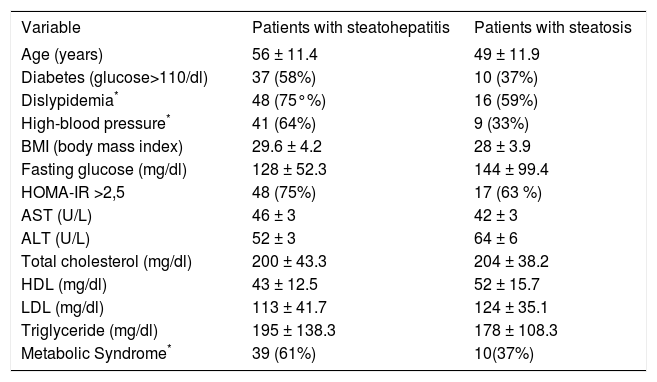
The table 1 shows demographic, clinical and biochemical parameters in patients with isolate steatosis and NASH. Some differences was observed in age and BMI when compared patients with NASH and steatosis. NASH patients also presented increased liver enzymes (AST and GGT), higher HOMA-IR index and lower HDL-cholesterol. However, statistical significance was not achieved.
Demographic, clinical and biochemical data of patients with histological diagnosis of steatosis and steatohepatitis (NASH) (n = 1280).
| Variable | Patients with steatohepatitis | Patients with steatosis |
|---|---|---|
| Age (years) | 56 ± 11.4 | 49 ± 11.9 |
| Diabetes (glucose>110/dl) | 37 (58%) | 10 (37%) |
| Dislypidemia* | 48 (75°%) | 16 (59%) |
| High-blood pressure* | 41 (64%) | 9 (33%) |
| BMI (body mass index) | 29.6 ± 4.2 | 28 ± 3.9 |
| Fasting glucose (mg/dl) | 128 ± 52.3 | 144 ± 99.4 |
| HOMA-IR >2,5 | 48 (75%) | 17 (63 %) |
| AST (U/L) | 46 ± 3 | 42 ± 3 |
| ALT (U/L) | 52 ± 3 | 64 ± 6 |
| Total cholesterol (mg/dl) | 200 ± 43.3 | 204 ± 38.2 |
| HDL (mg/dl) | 43 ± 12.5 | 52 ± 15.7 |
| LDL (mg/dl) | 113 ± 41.7 | 124 ± 35.1 |
| Triglyceride (mg/dl) | 195 ± 138.3 | 178 ± 108.3 |
| Metabolic Syndrome* | 39 (61%) | 10(37%) |
Liver biopsy was performed in 437 cases of 1280 patients included. Isolate steatosis was observed in 41.7%, steatohepatitis without fibrosis in 31.1% and steatohepatitis with fibrosis in 27% (total of NASH-58%) (Figure 1). Stages of fibrosis: S zero: 29.2%, S1: 36.1%, S2 in 11.7%, S3 in 7.6%, cirrhosis in 15.4% (Figure 2) and three of them have hepatocellular carcinoma (HCC).
DiscussionThe present study involves a large series of patients with NAFLD in Brazil and represents a contribution to describe a profile of these patients in South America, where there are no much information about this liver disease.
Among the 1280 cases of the NAFLD evaluated, the majority of them were asymptomatic male; with mean age of fifty years, and the most frequent risk factor to NAFLD were hyperlipidemia, obesity or overweight. Metabolic Syndrome (ATP III) was observed in 41.3% cases. All these features in Brazilians NAFLD patients are similar to other countries.15 A population-based study performed in the USA demonstrates that up to 34% of the adult general population has excessive fat accumulation in the liver, mostly unrelated to alcohol abuse.17 This high prevalence of NAFLD is most likely a result of the increasing prevalence of obesity, type 2 diabetes and metabolic syndrome in the general US population.3
In Japan, the results of a series of cross-sectional data obtained from patients presenting for a health checkup demonstrated that the prevalence of fatty liver on ultrasound increased from 12.6% in 1989, peaked at 30.3% in 1998, and was 28.4% in 2000.6 Furthermore, unless uniform data are available over the time period, the prevalence estimates of NAFLD could also be affected by a change in ascertainment based on increased awareness. Nevertheless, because of the marked increase in the prevalence of both obesity and type 2 diabetes, it is assumed that the prevalence of NAFLD is increasing as well.16
All these studies have suggested that ethnic differences may have a role in susceptibility to NAFLD, especially the progressive disease that cannot be explained simply on the basis of diet or socioeconomic differences. The higher incidence of NASH in US populations of Hispanic origin relative to Caucasian, and a lower incidence in African-Americans, despite a higher rate of obesity have suggested it.17,18
This Brazilian study showed that the majority of patients were males, with mean age of fifty years. This result are similar a population-based studies,19,20 however it is different of others studies also performed in patients selected of out-clinics, that have shown cases of NAFLD most common in middle-aged women.
The ethnic differences were not studied in this simple. In Brazil, the mixed racial heritage is recognized and it is an important subject to be investigated. It would be useful in future to identify them more precisely using accepted racial origin genetic markers, and it will be relevant to be used to set public policy in regards to population screening and/or public health intervention strategies.
Steatohepatitis with fibrosis and cirrhosis was frequent in patients, who underwent liver biopsy and three of hepatocellular carcinoma was observed. These results showed that NAFLD has a high potential of progression in this population. The mechanism of this progression is complex and remains to be understood. It clearly is multifactorial. Many cases are related to a lifestyle; however, it is likely that genetic predisposition plays an important role in determining which individuals have increased risk for development of cirrhosis and HCC in patients with NAFLD.
ConclusionThe study contributes with information about characteristics of NAFLD in South America. It describes the profile of NAFLD in Brazil, the largest country in South America. The patients did not present symptoms, however, the most frequent histological diagnosis in these simple was steatohepatitis with fibrosis and a significant number of cases already presented cirrhosis. These findings deserve a future investigation. Although the present study did not aim to evaluate pathogenic mechanisms, the genetic predisposition and lifestyle should be influenced in the spectrum of NAFLD in Brazil and the high frequency of severe disease in this population.
Abbreviations- •
NAFLD: Nonalcoholic Fatty Liver Disease.
- •
NASH: Nonalcoholic Steatohepatitis.
- •
MS: Metabolic Syndrome.
- •
BMI: Body Mass Index.
- •
IR: Insulin Resistance.
- •
ALT: Alanine aminotransferase.
- •
AST: Aspartate aminotransferase.
- •
GGT: Gamma Glutamyl Transpeptidase.
- •
HDL-C: High-density lipoprotein cholesterol.
- •
LDL-C: Low-density lipoprotein cholesterol.
- •
HOMA-IR-IR: Homeostasis Model Assessment of Insulin Resistance.
- •
SPSS: Statistical Package for Social Sciences.
The authors are grateful to the Brazilian Hepatologists Groups, to Dr. Luiz Antonio de Freitas and Dr. Venâncio Alves for the support on the protocol to histological diagnosis, and to the Sociedade Brasileira de Hepatologia.