Introduction. Alcoholic cirrhosis is one of the most common indications for liver transplantation (LT) in western countries. A major concern about transplant patients due to alcoholic liver disease (ALD) is alcoholic recidivism. Data concerning psycho-social characteristics of patients with 6 months of abstinence at initial evaluation for LT is scarce.
Objectives. The aims of this study were 1) To evaluate the psycho-social profile of a cohort of patients with alcoholic cirrhosis being evaluated for LT. 2) Determine factors associated with abstinence from alcohol at initial psycho-social evaluation for LT and 3) To evaluate the potential impact of alcohol-free beer consumption on 6-month abstinence.
Material and methods. Ninety patients referred to the Alcohol Unit of the Hospital Clínic of Barcelona (January 1995-December 1996) were included. Univariate and multivariate logistic regression analyses were used to identify the factors associated with cessation in alcohol consumption and with 6-month abstinence.
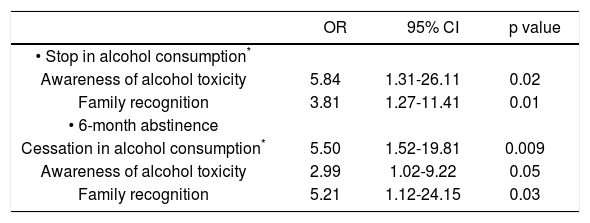
Results. Factors associated with cessation in alcohol consumption were awareness of alcohol toxicity (OR = 5.84, CI 1.31-26.11, p = 0.02) and family recognition (OR = 3.81, CI 1.27-11.41, p = 0.01). Cessation of alcohol consumption at knowledge of ALD (OR = 5.50, CI 1.52-19.81, p = 0.009), awareness of alcohol toxicity (OR = 2.99, CI 1.029.22, p = 0.05) and family recognition (OR = 5.21, CI 1.12-24.15, p = 0.03) were the independent factors associated with 6-month abstinence previous to psycho-social evaluation for LT.
Conclusion. In conclusion awareness of alcohol toxicity and family recognition are the independent factors that influence cessation in alcohol consumption and 6-month abstinence in patients evaluated for LT. The use of alcohol-free beer was associated with a higher rate of abstinence in patients without alcohol cessation.
Alcohol abuse is one of the main causes of preventable morbidity and mortality worldwide.1-5 Alcoholic liver disease (ALD) is the major cause of mortality among adult patients with alcohol abuse. Alcohol abuse is responsible for up to 50% of the cases of cirrhosis.4,6 As a consequence, alcoholic cirrhosis is one of the most common indications for liver transplantation (LT) in Europe and in North America.7-8 The workup of patients with ALD and cirrhosis undergoing evaluation of for LT is extensive and requires several steps and involves a proper evaluation by a multidisciplina-ry team in order to determine appropriateness of the procedure in any given candidate.9 Psychological assessment is a key element in the evaluation of patients with ALD and cirrhosis and is important for the transplant committee in deciding adequacy for LT.10,11 However, despite all these evaluations, some type of alcoholic recidivism after transplantation may occur in approximately 20-30% of patients, thus placing the patient and graft at risk of subsequent rejection or liver disease.12-13
The majority of liver transplant centers in the United States and Europe require a 6-month period of abstinence from alcohol as well as psychosocial clearance before acceptance in the LT list. Although this “6-month rule” of abstinence is considered arbitrary, it is associated with better post-LT outcomes in terms of less harmful-drinking and less relapse among patients who meet this criterion at initial evaluation.15,16 Other risk factors that identify those patients with a high risk of post-LT alcohol relapse are presence of mental illness, lack of family support, tobacco consumption, and lack of insight of alcohol as the cause of their disease at initial assessment.16-23 Currently, risk factors associated with failure to meet abstinence requirements for listing have not been adequately studied. In addition, information about the psycho-social characteristics of patients with 6 months of abstinence at initial evaluation for LT is scarce. Thus, the aim of this study was to evaluate the psycho-social profile of a cohort of patients with alcoholic cirrhosis being evaluated for LT and determine factors associated with abstinence from alcohol at the initial psycho-social evaluation for LT. Other aim was to evaluate the potential impact of alcohol-free beer consumption on 6-month abstinence.
Material and MethodsPatients and data collectionPatients referred to the Alcohol Unit (AU) of the Hospital Clinic of Barcelona, between January 1995 and December 1996, were prospectively included. All patients had a diagnosis of alcoholic cirrhosis and were in the process for evaluation for LT. All psycho-social data were collected in the first visit to the AU as part of the psychiatric evaluation before LT. Patients with other causes of liver disease and addiction to other type of substances (i.e. cannabis, cocaine, heroin, etc.) were excluded. Clinical, epidemiological, analytical and psychological parameters were collected.
For the purpose of the study, different parameters at the initial psychiatric evaluation prior to listing were assessed. The AU has extensive experience in the field of psychology and psychiatry of liver transplant patients. Data about prior alcohol consumption, consumption of psychotropic drugs, alcohol abstinence, time since last alcohol consumption, alcohol-free beer consumption and the number of previous alcohol detoxifying treatments were carefully collected. Patient information was obtained through a systematic clinical interview. This interview is divided into different sections and was administered by a trained professional. The section of demographic and social data explores the personal and familiar, organic, psychiatric and toxicology background. Another section examines the current disease according to the DSM-IV criteria for diagnosis of dependence and psychiatric impairment associated with alcohol consumption.24 Alcohol intake was evaluated by the Systematic Interview of Alcohol Consumption (SIAC).25 Patient's attitude during the first psychiatric visit was evaluated clinically according to the Minnesota Multiphasic Personality Inventory (MMPI) questionnaire.26 All collected information (from patient and relatives) was always compared with the information provided to other medical staff of the LT program of our center.
Clinical, psychiatric and social evaluationThe diagnosis of ALD was based on history of routine and risk alcohol consumption associated with clinical, histological and laboratory findings of alcohol abuse (alcohol serum levels, elevated liver enzymes and/or typical histological features on liver biopsy). Before listing, all patients underwent standard medical, social and psychiatric workup. Based on the experience with this workup we have recently published the clinical guidelines of our center for the evaluation of LT candidates with addictions.27 For patients with alcoholic cirrhosis, the listing policy of our center requires at least 6 months of abstinence from alcohol along with persistent sobriety and a positive follow-up for psychiatric and psychological evaluations. Finally, before and after being accepted on the LT waiting list, patients were subjected to ongoing alcohol abstinence monitoring with urine and blood alcohol tests every week. In our centre patients are not disqualified for LT candidacy if they report to drink alcohol free-beer. Thus, they are considered to be admitted to the waiting list.
DefinitionsCessation in alcohol consumption was defined as the complete cessation of alcoholic beverages at the first knowledge of alcohol-related liver disease. 6-month abstinence was defined as the absence of alcoholic beverages consumption 6 months prior to the AU psycho-social evaluation. Alcohol-free beer consumption was allowed in patients undergoing LT evaluation and was not considered an alcoholic beverage. Duration of abstinence previous to AU visit was evaluated by self-reporting and by confrontation questionnaires with the patients’ near relatives. Patients were defined as fasting alcohol consumers if the first consumption of an alcoholic beverage was previous to their first meal of the day. Awareness of alcohol toxicity was defined as the ability of the patient to understand and accept the existence of a negative consequence (physical, behavioral, legal, social, and/or familiar) directly related with his/her alcohol consumption. Alcohol dependence (AD) was defined according to the DSM-IV criteria. The awareness of AD was defined as the capacity of a patient to understand and recognize his/her failure to control alcohol intake. In those patients with AD awareness the presence of alcohol toxicity awareness was assumed.
The patients’ attitude was evaluated during the first visit to the AU. We stratified patients into three different subgroups: Honest attitude. Those patients with the capacity to understand and face the existence of medical and social problems related with the amount or frequency of alcohol consumption. Denial-defensive attitude. Patients with a tendency to minimize, deny or present a defensive behavior towards the evaluation of the different aspects of his/her medical problems, and Impaired attitude. Those with a denying/defensive attitude caused by a neuropsychological situation able to impair memory and cognitive functions affecting the understanding of problems related with alcohol consumption.
Detailed patient information about their family background and family active support were carefully measured by both a social worker and the AU team.
The main end-points for the study were cessation of alcohol consumption and alcohol abstinence ≥ 6 months prior to the psycho-social evaluation for LT.
Statistical analysisContinuous variables were described as median (25-75 interquartile range). Categorical variables were described by means of counts and percentages. Comparisons between groups were performed using the Student's t test or Mann-Whitney U test, depending on variable distribution. Differences between categorical variables were assessed by the chi-square test or Fisher's exact test, when necessary. To investigate variables with prognostic information for cessation of alcohol consumption and 6 months of abstinence at the psychiatrist's pre-transplant evaluation, those variables that were statistically significant (p ≤ 0.10), and those that were considered clinically relevant at the univariate analysis were entered into a backward stepwise elimination variable selection procedure (multivariate logistic regression) and then confirmed using a forward stepwise elimination variable selection procedure. The p-values for the univariate tests were not corrected for multiple testing, because those tests were taken as exploratory. The results of the multiva-riate logistic regression analysis (odds ratio –OR–) were considered to be the main result, as it determined those variables independently associated with the main outcome (after adjusting for time and the contributions of other variables). A p-value < 0.05 was required for significance. The SPSS statistical package (SPSS Inc., version 15.0, Chicago, IL.) was used for all analysis.
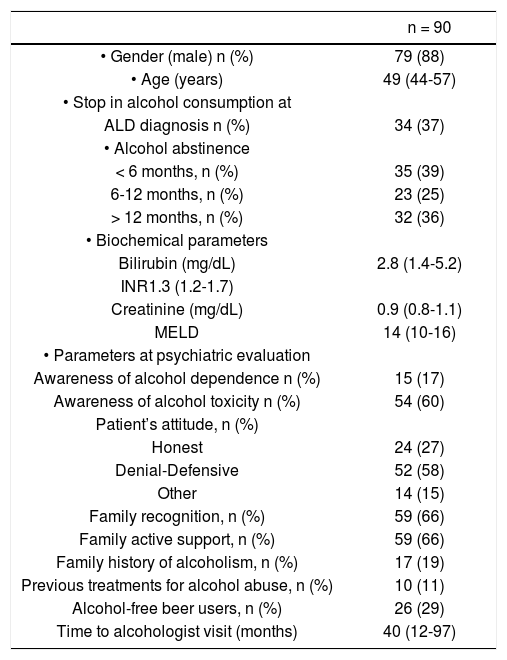
ResultsPatients’ characteristicsDuring the study period 90 patients were included. The baseline clinical, demographical and biochemical characteristics of the study cohort are depicted in table 1. 34 patients (37%) stopped their alcohol consumption at the moment of ALD diagnosis. 60% (55 out of 90 patients) arrived to first AU visit with 6 months of abstinence; among these, 58% (32 out of 55 patients) had at least 1-year abstinence. Regarding the characteristics of alcohol abuse and consumption pattern, 66% of the cohort were fasting alcohol consumers, 42% accepted to lose control when drinking and 30% were incapable to maintain 48 h of abstinence. Importantly, the median time between diagnosis of ALD and derivation to AU was 40 (12-97) months. 45 patients (50%) were successfully listed and transplanted. Half of the patients were not transplanted due to an inability to comply with listing requirements. Among these, 73% (33 out of 45 patients) had either a medical contraindication and/or died before LT listing. Four patients were not listed due to mental illness or psychiatric contraindication.
Baseline clinical and psychiatric characteristics of patients.
| n = 90 | |
|---|---|
| • Gender (male) n (%) | 79 (88) |
| • Age (years) | 49 (44-57) |
| • Stop in alcohol consumption at | |
| ALD diagnosis n (%) | 34 (37) |
| • Alcohol abstinence | |
| < 6 months, n (%) | 35 (39) |
| 6-12 months, n (%) | 23 (25) |
| > 12 months, n (%) | 32 (36) |
| • Biochemical parameters | |
| Bilirubin (mg/dL) | 2.8 (1.4-5.2) |
| INR1.3 (1.2-1.7) | |
| Creatinine (mg/dL) | 0.9 (0.8-1.1) |
| MELD | 14 (10-16) |
| • Parameters at psychiatric evaluation | |
| Awareness of alcohol dependence n (%) | 15 (17) |
| Awareness of alcohol toxicity n (%) | 54 (60) |
| Patient’s attitude, n (%) | |
| Honest | 24 (27) |
| Denial-Defensive | 52 (58) |
| Other | 14 (15) |
| Family recognition, n (%) | 59 (66) |
| Family active support, n (%) | 59 (66) |
| Family history of alcoholism, n (%) | 17 (19) |
| Previous treatments for alcohol abuse, n (%) | 10 (11) |
| Alcohol-free beer users, n (%) | 26 (29) |
| Time to alcohologist visit (months) | 40 (12-97) |
ALD: alcoholic liver disease. INR: international normalized ratio. MELD: model for end-stage liver disease.
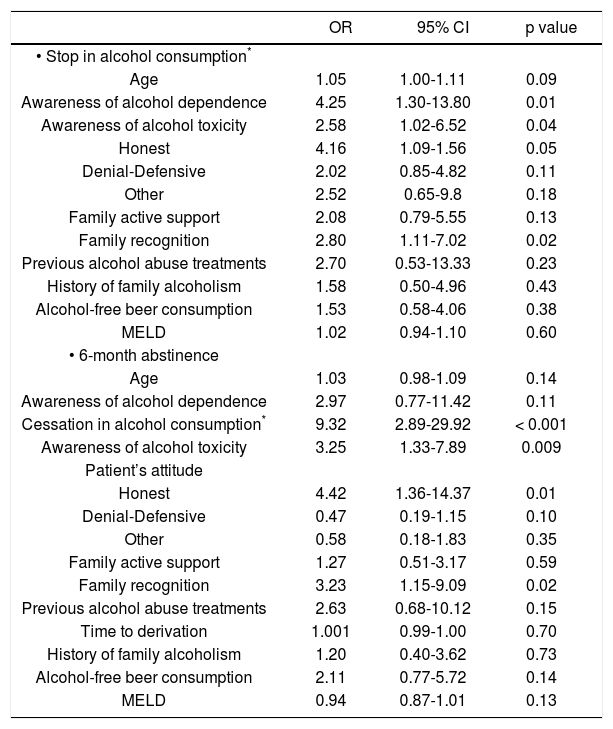
We first investigated the parameters associated with alcohol cessation after the diagnosis of ALD. Table 2shows the results of the univariate analysis performed in order to identify the variables associated with cessation of alcohol consumption. The factors significantly associated with alcohol cessation were:
- •
Awareness of AD (OR = 4.25, CI 1.30-13.80, p = 0.01).
- •
Awareness of alcohol toxicity (OR = 2.58, CI 1.02-6.52, p = 0.04).
- •
The patient’s honest attitude towards alcohol dependence and related toxicity (OR = 4.16, CI 1.09-1.56, p = 0.05) and family recognition of the problem (OR = 2.80, CI 1.11-7.02, p = 0.02).
Factors associated with stop in alcohol consumption* and 6-month abstinence in the univariate analysis.
| OR | 95% CI | p value | |
|---|---|---|---|
| • Stop in alcohol consumption* | |||
| Age | 1.05 | 1.00-1.11 | 0.09 |
| Awareness of alcohol dependence | 4.25 | 1.30-13.80 | 0.01 |
| Awareness of alcohol toxicity | 2.58 | 1.02-6.52 | 0.04 |
| Honest | 4.16 | 1.09-1.56 | 0.05 |
| Denial-Defensive | 2.02 | 0.85-4.82 | 0.11 |
| Other | 2.52 | 0.65-9.8 | 0.18 |
| Family active support | 2.08 | 0.79-5.55 | 0.13 |
| Family recognition | 2.80 | 1.11-7.02 | 0.02 |
| Previous alcohol abuse treatments | 2.70 | 0.53-13.33 | 0.23 |
| History of family alcoholism | 1.58 | 0.50-4.96 | 0.43 |
| Alcohol-free beer consumption | 1.53 | 0.58-4.06 | 0.38 |
| MELD | 1.02 | 0.94-1.10 | 0.60 |
| • 6-month abstinence | |||
| Age | 1.03 | 0.98-1.09 | 0.14 |
| Awareness of alcohol dependence | 2.97 | 0.77-11.42 | 0.11 |
| Cessation in alcohol consumption* | 9.32 | 2.89-29.92 | < 0.001 |
| Awareness of alcohol toxicity | 3.25 | 1.33-7.89 | 0.009 |
| Patient’s attitude | |||
| Honest | 4.42 | 1.36-14.37 | 0.01 |
| Denial-Defensive | 0.47 | 0.19-1.15 | 0.10 |
| Other | 0.58 | 0.18-1.83 | 0.35 |
| Family active support | 1.27 | 0.51-3.17 | 0.59 |
| Family recognition | 3.23 | 1.15-9.09 | 0.02 |
| Previous alcohol abuse treatments | 2.63 | 0.68-10.12 | 0.15 |
| Time to derivation | 1.001 | 0.99-1.00 | 0.70 |
| History of family alcoholism | 1.20 | 0.40-3.62 | 0.73 |
| Alcohol-free beer consumption | 2.11 | 0.77-5.72 | 0.14 |
| MELD | 0.94 | 0.87-1.01 | 0.13 |
OR: odds ratio. CI: confidence interval.
When including the MELD score in the univa-riate analysis we did not find any association to cessation in alcohol consumption. After entering those variables that were statistically significant in the univariate model and those clinically relevant in a multivariate analysis, only awareness of alcohol toxicity (OR = 5.84, CI 1.31-26.11, p = 0.02) and family recognition (OR = 3.81, CI 1.27-11.41, p = 0.01) remained statistically significant (Table 3). Awareness of alcohol dependence, previous alcohol abuse treatments and patient’s attitude were not significantly associated with cessation of alcohol consumption.
Factors associated with stop in alcohol consumption* and 6-month abstinence in the multivariate analysis.
| OR | 95% CI | p value | |
|---|---|---|---|
| • Stop in alcohol consumption* | |||
| Awareness of alcohol toxicity | 5.84 | 1.31-26.11 | 0.02 |
| Family recognition | 3.81 | 1.27-11.41 | 0.01 |
| • 6-month abstinence | |||
| Cessation in alcohol consumption* | 5.50 | 1.52-19.81 | 0.009 |
| Awareness of alcohol toxicity | 2.99 | 1.02-9.22 | 0.05 |
| Family recognition | 5.21 | 1.12-24.15 | 0.03 |
OR: Odds ratio. CI: confidence interval.
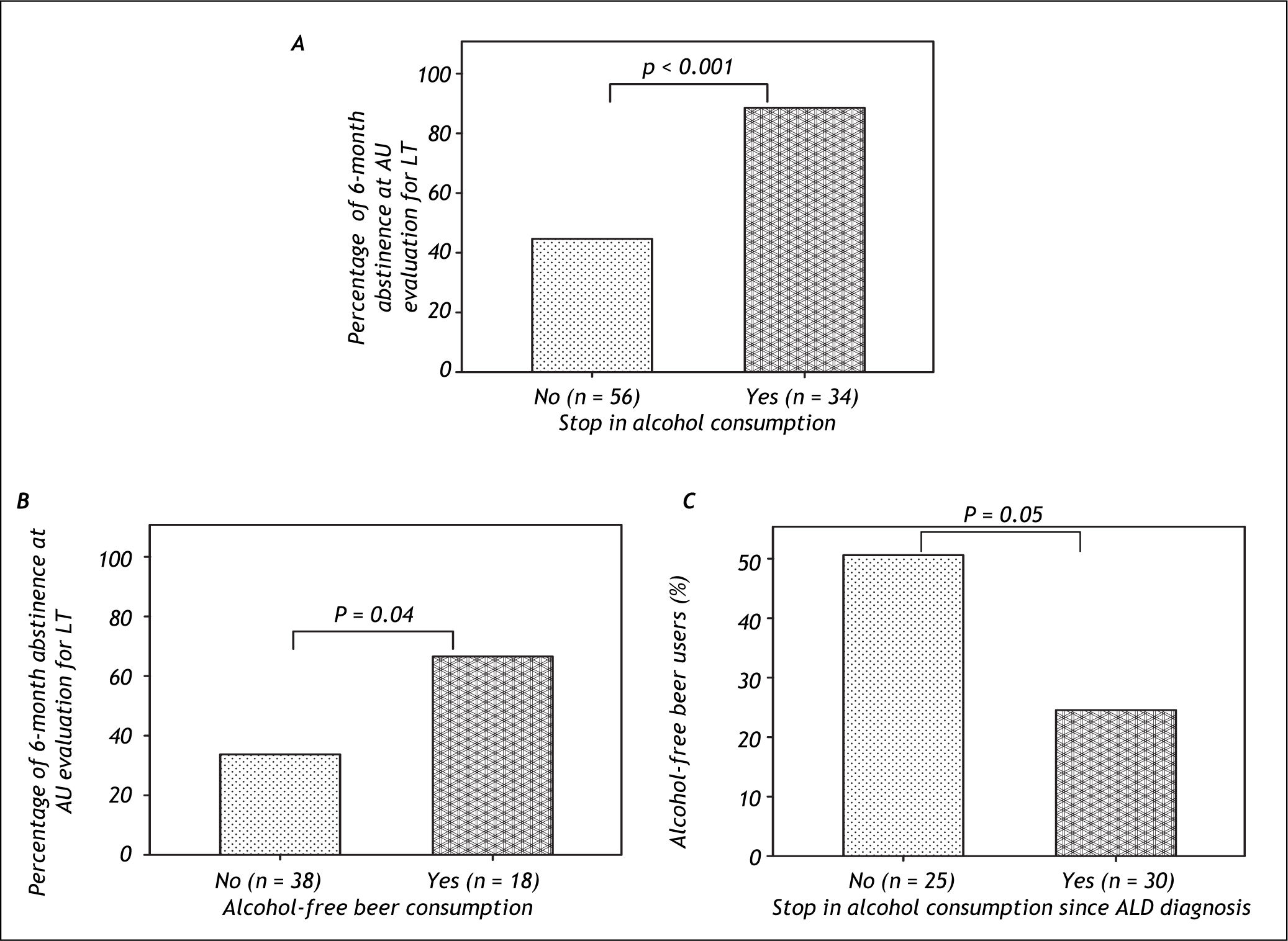
A univariate analysis was performed In order to identify the factors associated with 6-months of abstinence previous to the psycho-social evaluation (Table 2). Cessation in alcohol consumption at knowledge of alcohol-related liver disease (OR = 9.32, CI 2.89-29.92, p < 0.001), awareness of alcohol toxicity (OR = 3.25, CI 1.33-7.89, p = 0.009), patient’s honest attitude (OR = 4.42, CI 1.36-14.37, p = 0.01) and family recognition (OR = 3.23, CI 1.15-9.09, p = 0.02) were significantly associated with maintenance of abstinence. When including the MELD score in the univariate analysis we did not find any association to 6-months abstinence. To further analyze the variables predicting 6-months of abstinence, statistically significant and clinically relevant variables were entered in a multivariate model. Cessation of alcohol consumption at knowledge of alcohol-related liver disease (OR = 5.50, CI 1.52-19.81, p = 0.009), awareness of alcohol toxicity (OR = 2.99, CI 1.02-9.22, p = 0.05) and family recognition (OR = 5.21, CI 1.12-24.15, p = 0.03) were the only variables that showed a statistically significant association (Table 3). Awareness of alcohol dependence, patient’s attitude and alcohol-free beer consumption did not significantly predict maintenance of abstinence. Importantly, patients who stopped alcohol consumption at ALD diagnosis showed higher rates of 6 months of abstinence compared to those who did not stop alcohol (88 vs. 44%, respectively; p < 0.001) (Figure 1A).
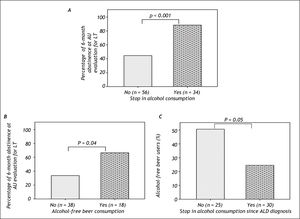
A. 6-month abstinence according to the presence of stop in alcohol consumption since ALD diagnosis. B. Rate of alcohol free-beer use according to the presence of stop in alcohol consumption after ALD among patients who arrive with 6-month abstinence to LT evaluation. C. 6-month abstinence rate according to the presence of alcohol-free beer consumption among patients without stop in alcohol consumption.
A total of 26 patients (29%) began using alcohol-free beer after knowledge of their ALD. 34% of patients (19 out of 55) with 6 months of abstinence and 20% (7 out of 35) without 6 months of abstinence were alcohol-free beer consumers (p = 0.12). Among patients that reached 6-month abstinence at initial AU evaluation the proportion of alcohol-free beer consumption was significantly higher in those who did not stop alcohol consumption at diagnosis of ALD (Figure 1B). We next compared the use of alcohol-free beer and the rate of 6 months of abstinence in both, patients with and without cessation of alcohol consumption at diagnosis of ALD. Among those who did not stop alcohol consumption, the use of alcohol-free beer was associated with a higher rate of 6-month abstinence (67 vs. 34%, p = 0.04) (Figure 1C). This association was not observed among patients that quit alcohol consumption at ALD diagnosis.
DiscussionALD is one of the commonest causes of cirrhosis and is also a frequent indication for LT. After early uncertainty, it is now widely accepted that the overall clinical outcomes of LT for carefully selected patients with ALD are similar to other causes of liver disease.28 A period of 6 months of abstinence has been widely adopted as it provides adequate time to demonstrate cessation of alcohol use and also provides the opportunity for many patients to recover adequately so as to no longer require LT. In addition, patients that achieve this “6-month rule” are less likely to incur in “problem drinking” after LT and it is a standard requisite in the vast majority, if not all, LT programs.14,27,29 On the other hand, the assessment of the psycho-social status of patients with ALD undergoing LT identifies those patients at particular risk to return to harmful consumption of alcohol post-LT.14,29,30 The psycho-social factors related with relapse are insight into alcohol etiology, family or friends’ active support, lack of mental illness, and a stable relationship.19-20,22,23,31
However, less has been described about the factors associated to 6-month abstinence at first evaluation for LT.
The results of our study demonstrate that more than 50% of patients were categorized as having toxicity awareness and only 17% were aware of their dependence on alcohol. As expected, almost 60% of patients showed a defensive-denial attitude. This type of attitude is not surprising and expected in patients with ALD since the appearance of the negative physical consequences associated with alcohol use usually triggers ambivalent situations about such consumption and a defensive and negative position towards medical and family warnings.32 Moreover, these attitudes could also be explained by the fact that during the course of LT psycho-social evaluation patients may find themselves living two distressing situations: sense of imminent death; or rebirth through the transplant.
During this phase, patients often doubtful feel anxiety, ambivalence, fears and frustration, all of these potential causes of the patient’s challenging attitude. In our series, almost 70% of the patient’s families recognized the problem and were actively supporting the patient. These figures are in keeping with previous studies.30-31,33 Additionally, we found a median of 40 (IQR 12-97) months between first diagnosis of ALD and first visit to AU. This last observation leads us to raise the concern on the urgent need for better care and better algorithms for referral to specialized AU centers not only when OLT is the last option for their treatment. This mean time to first visit to AU can be mostly explained due to the lack of consciousness of most of the first attention units in the opportune derivation of patients with ALD no matter what stage of the disease are the patients coursing. We think that early derivation of patients with ALD to AU could positively impact in their long term prognosis.
An interesting finding of our study was the recognition of factors related to stopping alcohol and 6 months of abstinence prior to LT evaluation. We found the presence of alcohol toxicity awareness and family recognition as the independent factors associated with cessation of alcohol consumption (Figure 1). These are important observations in order to identify those patients with a high probability of meeting the alcohol abstinence criteria needed for listing at the first AU visit. Variables independently associated with 6-month abstinence were cessation of alcohol consumption, alcohol toxicity awareness and family recognition. Thus, these results indicate such patients (e.g. patients without alcohol cessation after ALD diagnosis) could benefit from early interventions in specialized addictions units. These results also support the notion that the process, by which a person transitions from active addiction to sustained recovery, is actually based on a progressive awareness process.34
Finally, we focused on the potential association of the use of alcohol-free beer and 6 months of abstinence. Among patients without cessation of alcohol consumption at first knowledge of alcohol-related liver disease, we found that the use of alcohol-free beer consumption was significantly associated with higher rates of 6-months of abstinence (Figure 1C). Importantly, when analyzing those patients who arrive at LT evaluation with 6 months of abstinence we found that the rate of alcohol-free beer use was more frequent among those patients that did not stop alcohol since ALD diagnosis (Figure 1B). Although interesting, these last observations should be taken with caution for several reasons. First, although alcohol-free beer use may not have a deleterious impact from a strictly organic and toxicological point of view given the low alcohol component of the beverage, it does have a great impact from the psychological perspective. The existing psychological component of addiction takes special importance in this case. The consumption of a drink with identical stimulation features (e.g. similar taste, presentation, color, and drinking situation) may lead to similar expectations, thus disable the patient to acquire alcohol dependence awareness which is a major contributor to sustained abstinence. Second, only a small portion of patients initiate the use of alcohol-free beer after ALD diagnosis (29%) so this observation is based in small group of patients.
Our study has strengths and limitations. One of the strengths is that psycho-social evaluations were evaluated by means of a comprehensive structured interview applied by experienced personnel in addictions. On the other hand, few studies have evaluated the risk factors for failure to meet listing requirements in liver transplant candidates with alcoholic cirrhosis. In our study we evaluated factors associated with stopping alcohol consumption and 6-months of abstinence. Another original point in this study was the evaluation of the use of alcohol-free beer among patients evaluated for liver transplantation. Then main limitation of the study is the retrospective nature and lack of follow-after LT, thus variables regarding relapse in the post LT period could not be evaluated.
In summary, the factors that influence both cessation in alcohol consumption and sustained alcohol abstinence (6 months or more) in ALD patients evaluated for LT are the awareness of alcohol toxicity and family recognition of the problem. The use of alcohol-free beer was associated with a higher rate of 6-months of abstinence in the subgroup of patients who did not stop alcohol intake at ALD diagnosis. Future studies are required to validate this last observation.
Acknowledgments & Grant SupportThis work was supported by grants from Fondo de Investigacion Sanitaria (FIS PI080237 and FIS PS09/01164 to RB and JC). JA has a grant from Fundacion Banco Bilbao Vizcaya Argentaria (FBBVA) and is enrolled in the Master on Research in Liver Diseases of the Universitat de Barcelona. CIBERehd is funded by the Instituto de Salud Carlos III.
Abbreviations- •
ALD: Alcoholic liver disease.
- •
LT: Liver transplantation.