Background. Minimal hepatic encephalopathy (MHE) has implications for health-related quality of life as well as for survival of cirrhotic patients, but a standardized diagnostic test is not available.
Objective. To determine the prevalence of MHE among cirrhotic patients by using the psychometric hepatic encephalopathy score (PHES) system and the critical flicker frequency (CFF) test to diagnose MHE and to identify factors that influence the results of these tests.
Material and methods. From April 2007 to March 2008, PHES and CFF tests were performed on patients with cirrhosis but no overt hepatic encephalopathy. Descriptive statistics were used to express the results and the Spearman correlation was used to evaluate CFF and PHES results according to age and education level.
Results. We studied 104 patients. The prevalence of MHE was 55.8% (n = 58) based on a positive result for either the PHES or the CFF test, 32.7% (n = 34) based on positive PHES results alone, 34.6% (n = 36) based on positive CFF test results alone and 11.5% (n = 12) based on a positive result for both tests. According to PHES, the incidence of MHE was correlated with education level (r = 0.333, p = 0.001), but not with age. According to CFF, the incidence of MHE was correlated with age (r = -0.93, p = 0.049), but not with education level.
Conclusion. The prevalence of MHE was similar to that previously reported. Patient literacy influences MHE diagnosis with PHES but not with CFF. CFF is a simple and feasible method that identifies patients with MHE who may benefit from treatment independently of their education level.
Liver disease constitutes one of the main causes of mortality worldwide.1 In Mexico, chronic liver disease was the second highest cause of mortality from 2000 to 2008 among the economically active population (15-64 years old), with an estimated incidence of 25.5 to 28.9 cases per 100,000 inhabitants.2 Hepatic encephalopathy (HE) constitutes one of the principal markers of survival among patients with cirrhosis. As hepatic reserve declines, the probability of acute HE episodes increases, thus reducing survival.3-4 Although it is part of the spectrum of HE, minimal hepatic encephalopathy (MHE) does not manifest clinically, as there are no overt signs or symptoms. The prevalence of MHE has been estimated to be between 20 and 74%, but a gold standard for diagnosis has not yet been developed.5-9
Diagnosing MHE is of great importance because of its effect on quality of life, that is, on the patient’s ability to tolerate adverse daily events,10-11 and its presence confers a higher overt HE.6-7 However, few experimental studies12-13 or clinical trials14-15 have been conducted to characterize the association between MHE and HE. A recent publication by the American Association for the Study of Liver Diseases recommends that MHE should be diagnosed and treated.16 Evidence from neurocognitive studies has concluded that MHE primarily affects areas related to the attention and visuospatial domains.17 Therefore, tests that assess the status of these domains should have good diagnostic reliability. In particular, the psychometric hepatic encephalopathy score (PHES) has proven to be useful for MHE diagnosis.18 In addition, the critical flicker frequency (CFF) test has been demonstrated to be a useful, reliable and easy-to-perform test for diagnosing MHE.19-21 CFF results have a strong correlation with PHES results,22 and do not require standardization for age or literacy, both of which are required for PHES assessment.23 We conducted this study because information on the prevalence of MHE among the Mexican population, which is currently lacking, would enable the quality of life of this group to be improved. We evaluated the PHES and the CFF test in terms of diagnostic accuracy for MHE and determined whether age or education level influences the results of these tests.
Material and MethodsPatient selectionFrom April 1, 2007, to March 31, 2008, we enrolled patients with a diagnosis of compensated cirrhosis that was confirmed by clinical or biochemical methods, radiological studies or a liver biopsy. We excluded patients with evident HE according to the West Haven Criteria24 or a history of previous decompensated liver disease (variceal bleeding, hepatorenal syndrome, hepatocellular carcinoma), as well as those who used psychoactive drugs (psychotropic, antiepileptic or illegal drugs, or alcohol). No patients were excluded because of portosystemic shunts.
A diagnosis of alcohol-related liver disease was made when daily alcohol consumption was > 80 g for men or > 30 g for women and the patients were negative for viral, metabolic and autoimmune markers.25 Diagnosis of hepatitis C or B virus-related liver disease was conducted using specific viral serology (HBsAg or anti-HCV). Autoimmune liver disease was diagnosed using specific autoimmune markers (antinuclear antibodies, anti-smooth muscle antibodies or liver-kidney antimicrosomal antibodies).26 Nonalcoholic liver disease was defined as the presence of metabolic syndrome in the absence of significant alcohol consumption (< 140 g/week) or was identified using histological methods.27 Patients whose diagnostic workup did not identify an etiology were classified as having cryptogenic cirrhosis.28 Education level was classified according to academic grades currently used by the public education system in Mexico.29
Neuropsychiatric evaluation- •
Psychometric hepatic encephalopathy score. The PHES battery was applied using the Spanish standardization, and results were corrected according to the normality tables for age and education level (available from: http://www.redEH.org) and were expressed in points. PHES was considered abnormal when the score was two standard deviations greater than the mean of the paired controls (score < 4).18
- •
Critical flicker frequency. To measure CFF, we used a portable Hepatonorm Analyzer® (R&R Medi-Business Freiburg GmbH, Freiburg, Germany).19,21-22 Measurements were conducted between 13:00 h and 16:00 h in a quiet, isolated and weakly illuminated room. CFF was considered abnormal when the value was < 38 Hz.
Data were expressed as frequencies and percentages according to the presence or absence of MHE. Continuous variables were expressed as the mean ± standard deviation. The relationships between PHES and CFF and age and education level were evaluated using Spearman’s rank correlation coefficient. Statistical analysis was performed using SPSS software for Windows, version 17.0 (SPSS, Chicago, IL).
Ethical considerationsEvery patient included in the study signed an informed consent form to undergo CFF and PHES testing. The study was approved by the Ethics Committee of the Hospital Universitario de Monterrey according to the Helsinki Declaration (1989) for human research.
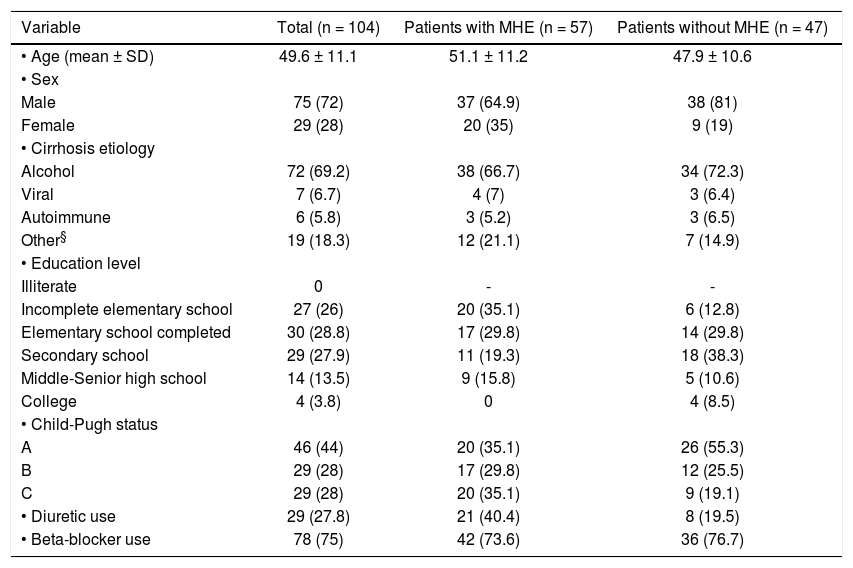
ResultsWe enrolled 104 patients who fulfilled the inclusion criteria. Complete follow-up for 2 years was achieved for all patients except those who died. Patient demographic and clinical characteristics are shown in table 1.
Demographic and clinical characteristics of patients enrolled in this study.
| Variable | Total (n = 104) | Patients with MHE (n = 57) | Patients without MHE (n = 47) |
|---|---|---|---|
| • Age (mean ± SD) | 49.6 ± 11.1 | 51.1 ± 11.2 | 47.9 ± 10.6 |
| • Sex | |||
| Male | 75 (72) | 37 (64.9) | 38 (81) |
| Female | 29 (28) | 20 (35) | 9 (19) |
| • Cirrhosis etiology | |||
| Alcohol | 72 (69.2) | 38 (66.7) | 34 (72.3) |
| Viral | 7 (6.7) | 4 (7) | 3 (6.4) |
| Autoimmune | 6 (5.8) | 3 (5.2) | 3 (6.5) |
| Other§ | 19 (18.3) | 12 (21.1) | 7 (14.9) |
| • Education level | |||
| Illiterate | 0 | - | - |
| Incomplete elementary school | 27 (26) | 20 (35.1) | 6 (12.8) |
| Elementary school completed | 30 (28.8) | 17 (29.8) | 14 (29.8) |
| Secondary school | 29 (27.9) | 11 (19.3) | 18 (38.3) |
| Middle-Senior high school | 14 (13.5) | 9 (15.8) | 5 (10.6) |
| College | 4 (3.8) | 0 | 4 (8.5) |
| • Child-Pugh status | |||
| A | 46 (44) | 20 (35.1) | 26 (55.3) |
| B | 29 (28) | 17 (29.8) | 12 (25.5) |
| C | 29 (28) | 20 (35.1) | 9 (19.1) |
| • Diuretic use | 29 (27.8) | 21 (40.4) | 8 (19.5) |
| • Beta-blocker use | 78 (75) | 42 (73.6) | 36 (76.7) |
The prevalence of MHE was 54.8% (n = 57) based on a positive result for either the PHES or the CFF test, 31.7% (n = 33) based on positive PHES results alone, 34.6% (n = 36) based on positive CFF test results alone and 11.5% (n = 12) based on a positive result for both tests. The prevalence of MHE according to Child-Pugh status is shown in figure 1. Note that the prevalence of MHE among Child-Pugh class C patients was 72.4% (n = 21).
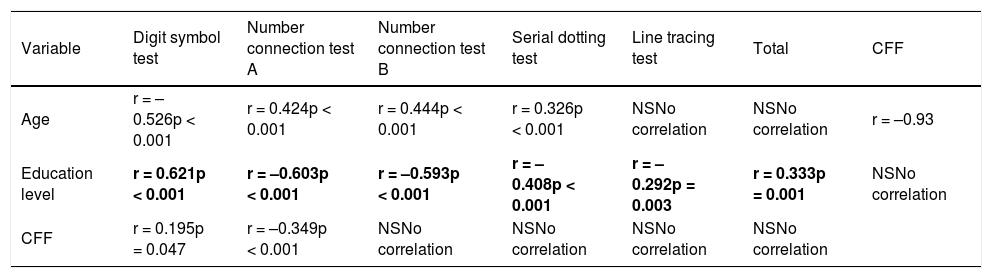
Correlation of PHES and CFF with age and education levelSpearman correlation analysis showed that PHES was correlated with education level (r = 0.333, p = 0.001) but not age (Table 2). Conversely, CFF was correlated with age (r = -0.93, p = 0.049) but not education level (Table 2 last column).
Correlations between age, education level, CFF and PHES.
| Variable | Digit symbol test | Number connection test A | Number connection test B | Serial dotting test | Line tracing test | Total | CFF |
|---|---|---|---|---|---|---|---|
| Age | r = –0.526p < 0.001 | r = 0.424p < 0.001 | r = 0.444p < 0.001 | r = 0.326p < 0.001 | NSNo correlation | NSNo correlation | r = –0.93 |
| Education level | r = 0.621p < 0.001 | r = –0.603p < 0.001 | r = –0.593p < 0.001 | r = –0.408p < 0.001 | r = –0.292p = 0.003 | r = 0.333p = 0.001 | NSNo correlation |
| CFF | r = 0.195p = 0.047 | r = –0.349p < 0.001 | NSNo correlation | NSNo correlation | NSNo correlation | NSNo correlation |
PHES: Psychometric hepatic encephalopathy score. CFF: Critical Flicker Frequency Test.
The prevalence of MHE among our population of cirrhotic patients according to a positive PHES or CFF test result was 54.8%, which is among the highest prevalence rates reported in the literature.6-7,9,11,30 MHE is associated with subjacent liver reserve, as demonstrated by a high frequency among Child-Pugh class C patients (72.4%, n = 21) (Figure 1), as has been reported previously.6,31 The most common etiology was excessive alcohol consumption, which concurs with the epidemiology of chronic liver disease in Mexico.32
For MHE diagnosis, neurofunctional tests for cirrhotic patients should ideally assess various aspects of cerebral function. In this study, we employed the PHES battery, which assesses the abstract and psychomotor domains and can identify subtle alterations in neuronal coordination of the encephalon18,23 as well as extrapyramidal alterations.33 The CFF test enables assessment of alterations in the visuospatial domain via stimulation of retinal neurons (Müller glial cells),34 the conduction of which is affected by low-grade edema and thus MHE. Data from PHES assessments are usually standardized according to age and literacy. Our results demonstrate that education level affects the diagnostic accuracy of PHES for MHE, even though the Spanish reference tables were used.18,23 This phenomenon was not observed for CFF, but its diagnostic accuracy was affected by age. Further study of the effect of age on the diagnostic accuracy of CFF for MHE is warranted.
ConclusionThe prevalence of MHE was high in our study population. MHE can be diagnosed using either the PHES or CFF test, but the diagnostic accuracy of PHES may be affected by literacy. Although age affected the diagnostic accuracy of CFF, this effect may be associated with neuronal degeneration and should be confirmed by larger controlled trials. Nonetheless, CFF remains a useful method in the diagnostic workup for MHE.