Background and aim: Non-alcoholic fatty liver disease (NAFLD) is a common cause of chronic liver disease and liver transplantation in western countries. Increasing incidence of NAFLD has been well documented from Asian countries like Japan and China. Diabetes mellitus (DM), obesity, hyperinsulinemia are predisposing factors for NAFLD. There is increase in incidence of DM, obesity and insulin resistance in India in last two decades. Hence it is logical to expect increase in incidence of NAFLD in India. There is limited data on the prevalence of NAFLD from India. Majority of data comes from hospital based studies including small number of patients. Therefore this study was planned to estimate the prevalence of NAFLD in general population. Material and methods: Residents of two Railway colonies were evaluated on history, clinical examination, anthropometric measurements, biochemical tests and abdominal ultrasound. Results: 1,168 participants were evaluated. Persons with any amount of alcohol consumption, HBs Ag positive, Anti HCV positive, persons with other known liver diseases and taking medications causing liver disease were excluded. Prevalence of NAFLD on ultrasound was 16.6%. Out of 730 subjects above the age of 20 years (341 male 384 female 389) mean age 39.08 ± 12.3 years, 4% had diabetes, 57% had central obesity. Prevalence of NAFLD based on the ultrasound above 20 years of age was 18.9%. NAFLD was more prevalent in male than female (24.6% vs 13.6%, p < 0.001). Risk factors associated with NAFLD were age more than 40 years, male gender, central obesity, high BMR > 25, elevated fasting blood sugar, raised AST and ALT. Conclusion: Prevalence of NAFLD in Indian population is comparable to the west.
Non-alcoholic fatty liver disease (NAFLD) is a common condition characterised by excess of fat in liver which ranges from simple steatosis to steatohepatitis, cirrhosis and hepatocellular carcinoma (HCC) in the absence of excessive alcohol intake.1 Metabolic syndrome and conditions associated with it like diabetes, obesity and dyslipidemia are predisposing factors of NAFLD.2 NAFLD is becoming a major public health problem due to rising incidence of obesity and type II diabetes.3 The overall prevalence of NAFLD is 15 to 40% in western countries while 9-40% in Asian countries.1 The data from Asian countries derived from various published series where there was no uniformity in definition of NAFLD and population studied. NAFLD is a common cause of chronic liver disease and liver transplantation in western countries.4 Increasing incidence of NAFLD has been well documented from Asian countries like Japan and China.5 Diabetes mellitus (DM), obesity, hyperinsulinemia are predisposing factors NAFLD. There is increase in incidence of DM, obesity and insulin resistance in India in last two decades.6,7 Hence it is logical to expect increase in incidence of NAFLD in India. There is limited data on the prevalence of NAFLD from India.8,9 Majority of data comes from hospital based studies including small number of patients. Therefore this study was planned to estimate the prevalence of NAFLD in general population.
Material and methodsStudy design; The population based study was performed at two different railway colonies in Central Mumbai India, (which is urban population), from December 2003 to January 2004. Study population was 1,168 residents of two colonies. Institutional review boards’ permission was obtained for the study. Written consent was obtained from all the residents. During two months time three medical gastroenterologist alongwith the resident doctors and staff nurses surveyed all the residents of these two colonies. Total of 1,168 subjects underwent complete history evaluation, physical examination and anthropometric measurements. Detailed history including history of alcohol consumption, usage of medication including alternative medication and food supplements was taken. Prior history of jaundice, liver disease, history of diabetes, hypertension, dyslepidemia, blood transfusion, tattooing, surgery, dental treatment was obtained. Interviewers checked medication consumed physically. Thorough clinical examination including height, weight waist and hip circumference was done. After 12 hours of fasting on the following day of interview participants were subjected to biochemical testing for serum aminotransferases, (Merk reagent), Hepatitis B surface antigen, antibodies to hepatitis C virus (third generation assay) (Abbott laboratories, Chicago. 2005) fasting blood glucose levels (Hexokinase). All biochemical assessments were performed in the same laboratory by standard laboratory methods by a single pathologist who was unaware of clinical findings.
Radiological examinationFatty liver was diagnosed by abdominal US using standardized criteria. US were performed in all subjects with the two equipment (ALOKA 500 and JUST VISION, TOSHIBA 2000 with a 3.5 MHz convex probe). Sonographic fatty liver was defined according to a combination of liver-kidney contrast (bright liver) with vascular blurring.10 Two sonologist, both of them were blinded to the clinical status of the individuals. Unfortunately, however, the interobserver reliability, designed to provide a measure of correlation between the observers rating, was not assessed prior to the inspection of the study.
Statistical analysisAll data were analyzed on computer using SPSS version 11.5 package (Chicago, IL, USA). Continuous variables are presented as mean ± standard deviation (SD). Comparison of continuous variables was performed with the chi-square test. Data were rechecked and verified for accuracy and inconsistent values. The odds ratio (OR) and 95% confidence interval (CI) for NAFLD risk factors were calculated with a Chi-Square value (Continuity Correction) and The risk factors for NAFLD, was calculated by using the Pearson’s correlation Coefficient and Spearman Correlation Coefficient of variables. The cut off value for BMI were based on accepted criteria and obesity was labelled if the BMI • • 25 kg/m2. The cut off value for central obesity were waist circumference > 80 cm in women and > 90 cm in men.
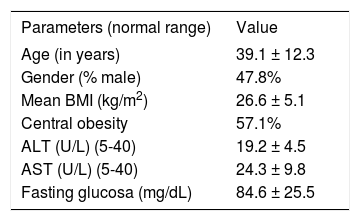
ResultsTotal of 1,168 individuals were evaluated completely. One hundred and forty five persons who consumed alcohol and 13 patients who were either HBsAg positive or anti HCV positive or consuming hepatotoxic drug were excluded from the analysis. The prevalence of NAFLD was highest in the age group of 40 to 60 years. It was more common in males than females. Out of 1,010 persons evaluated prevalence of risk factor and NAFLD was as follows : DM n = 94, (NAFLD 20%), over weight n = 180, (NAFLD 18%), obesity n = 327 (NAFLD 14.6%), central obesity n = 112 (NAFLD 15%). In patients with NAFLD 5% had hepatomegaly, 16% had SGPT more than upper limit of normal. (normal limits 15-40 Iu/mL), 9% had SGOT more than upper limit of (normal limits 15-40 Iu/mL). In patients with NAFLD 22% had diabetes, 52% had obesity and 38% had central obesity. Further analysis was done only for adult persons above the age of 20 years. This group included 730 subjects, 341 males, mean age 39.08 ± 12.23 years, diabetes was present in 4% (95% confidence interval, 0 to 7.8 %). Prevalence of central obesity measured by wait hip ratio more than 0.9 for male and more than 0.85 for women was seen in 62.8%. Central obesity measured by waist circumference more than 90 cm in men and 80 cm in women was present in 57.1%. All the investigations for diagnosing metabolic syndrome were not done in all patients. Characteristic features of metabolic syndrome like diabetes, central obesity have been shown in theTable I. Overall prevalence of metabolic syndrome in patients with NAFLD is more than 80% in Indian studies.9
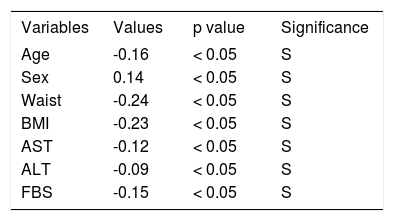
Pearson’s correlation coefficient of USG† fatty liver with following variables.
| Variables | Values | p value | Significance |
|---|---|---|---|
| Age | -0.16 | < 0.05 | S |
| Sex | 0.14 | < 0.05 | S |
| Waist | -0.24 | < 0.05 | S |
| BMI | -0.23 | < 0.05 | S |
| AST | -0.12 | < 0.05 | S |
| ALT | -0.09 | < 0.05 | S |
| FBS | -0.15 | < 0.05 | S |
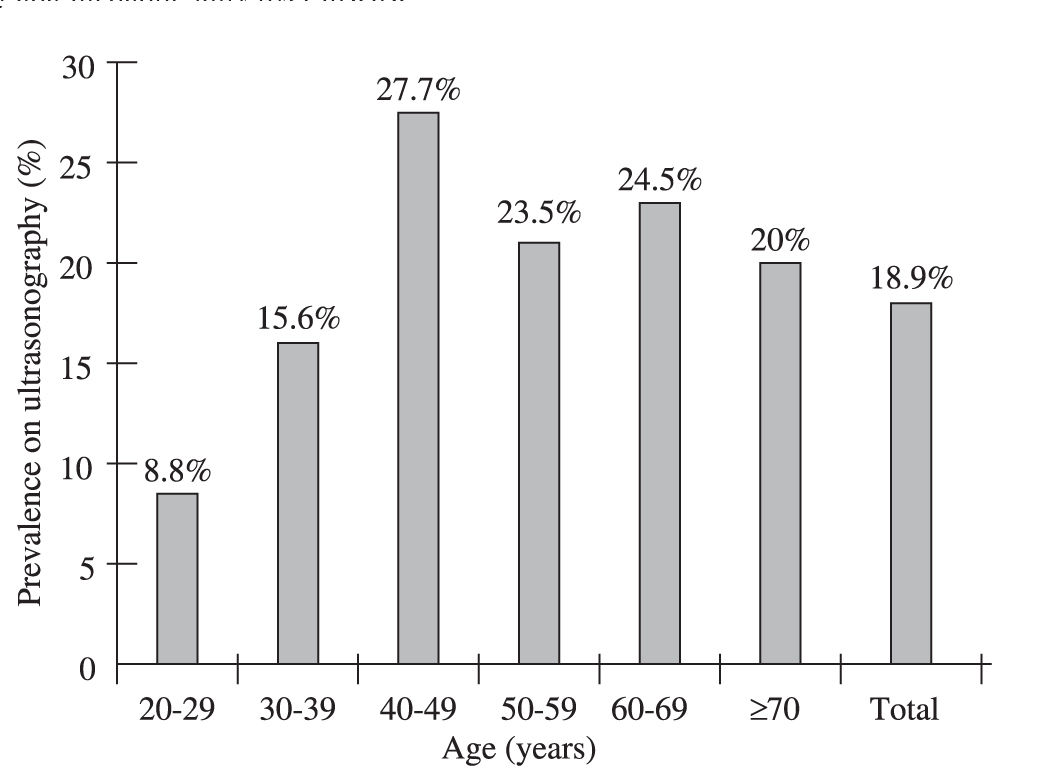
Study characteristic of adult patients with NAFLD is shown inTable II. Age specific prevalence of NAFLD in adult population is shown inFigure 1. Binary logistic regression model was constructed for prediction of NAFLD with the help of age, sex, central obesity, obesity, BMI, diabetes, AST, ALT. The analysis revealed that the central obesity, diabetes, BMI and male gender were statistically important in predicting the NAFLD. Pearson’s correlation coefficient of fatty liver on ultrasound was significant for following variables. Age more than 40 years, male sex, waist circumference more than 90 cm in male and more than 80 cm in female. BMI more than 25, AST, ALT more than 40 Iu/ML and fasting blood sugar more than 126 mg/dL(Table I).
Characteristics of the study population (means ± SD)
| Parameters (normal range) | Value |
|---|---|
| Age (in years) | 39.1 ± 12.3 |
| Gender (% male) | 47.8% |
| Mean BMI (kg/m2) | 26.6 ± 5.1 |
| Central obesity | 57.1% |
| ALT (U/L) (5-40) | 19.2 ± 4.5 |
| AST (U/L) (5-40) | 24.3 ± 9.8 |
| Fasting glucosa (mg/dL) | 84.6 ± 25.5 |
ALT, alanine aminotransferase; AST, aspartate aminotransferase, BMI, body mass index.
This is the first population based study from India which shows overall prevalence of NAFLD is 9% and it is around 19% in adult population. NAFLD is more common in men. Risk factors for NAFLD are similar to reported from the rest of the world. Some of the studies from India have suggested NAFLD in lean patients.11-13 In our study prevalence of obesity or central obesity was more than 60%. The mean BMI in our study 26.6%/-5%. Recent study from Delhi also has found similar observation, mean BMI patients with NAFLD was 26.7% and almost 70% of the patients had obesity as defined by the Asian pacific criteria.13 Similarly in our previous study on biopsy proved NAFLD patients, we found 92% prevalence of obesity by using Asian pacific criteria.14
The strength of the present study is that it included a large population. Limitation of the study was that. Inter observer reliability designed to provide a major of correlation between the observers rating for ultrasonographic evaluation was not done. Still today gold standard for diagnosis of NAFLD is histological evaluation. Ultrasonography can not differentiate NAFLD and NASH.11 Positive predictive value of ultrasound is only 34%.15 We could not validate ultrasound finding in some of the patients with histology. In our previous study on diabetics we have demonstrated more than 90% sensitivity of ultrasound in predicting NAFLD when compared with the histological evaluation.16
ConclusionThe results of the present study clearly demonstrate that the prevalence of NAFLD in Indian adults have some definite risk factors like advance age, sex difference and central obesity which leads to increasing burdens to chronic liver disease in Indian population.