Background and rationale. Cirrhosis is responsible for significant health-care costs and morbidity. This study aims to evaluate the burden of illness associated with cirrhosis, its impact on the universal coverage public health care system in Thailand.
Material and methods. We used data from the 2010 Nationwide Hospital Admission Data, the National Health Security Office (NHSO), Thailand. Their baseline characteristics, hospital costs, and outcomes were analyzed according to national health insurance categories including medical welfare scheme (MWFS), social security scheme (SSS) and civil servant medical benefit scheme (CSMBS).
Results. 92,301 admissions were eligible for analysis. The mean age was 55 ± 12.8 years, and 63.3% of patients were above 50 years old. The majority of patients (79%) belonged to the MWFS group. The MWFS group incurred the lowest medical expense and had the shortest hospital stay compared to the SSS and CSMBS groups. Overall in-hospital mortality was 10.7%. Cirrhosis complications include bleeding esophageal varices, spontaneous bacterial peritonitis, hepatic encephalopathy, hepatorenal syndrome, and hepatocellular carcinoma. These complications significantly increased mortality rates compared to patients without complications (26 vs. 8.9%, p < 0.001). In-hospital mortality of patients with cirrhosis complications did not differ among the three national health insurance groups. Respiratory failure and septicemia were associated with the highest risk of death (HR 5.4; 95% CI: 4.8-5.9 and HR 5.2; 95% CI: 4.9-5.6 respectively; P < 0.001).
Conclusions. Illness associated with cirrhosis is a significant public health problem in Thailand. Outcomes of cirrhosis complications did not differ between universal public health care coverage systems in Thailand.
Cirrhosis is the end-stage of every chronic liver disease. Its natural history is characterized by an asymptomatic phase followed by a rapidly progressive phase marked by the development of complications of portal hypertension and/or liver dysfunction.1 Various common chronic liver diseases such as alcohol consumption, metabolic syndromes related to overweight and obesity, viral hepatitis B and C have end results of liver cirrhosis and hepatocellular carcinoma.2 Reviewed data in Europe demonstrated that cirrhosis-associated mortality is at least comparable with other diseases that are considered to be of major public health concern, such as breast cancer, colon cancer, chronic lung disease and renal diseases.3 Liver-related mortality has been underestimated during the past two decades in the United States and Brazil.4,5 There are nearly as many mortality cases attributed to complications of cirrhosis as there are to diabetes, and more than are attributable to kidney diseases.6 Cirrhosis is also responsible for significant health-care costs and morbidity, and the incidence of hospitalizations due to cirrhosis complications is increasing.7–9 Besides cirrhosis complications, various co-morbidities such as diabetes, cardiovascular disease, and chronic kidney disease also affect the prognosis of cirrhosis patients.10 A study in chronic hepatitis B patients in Thailand showed that the yearly cost of treatment for patients with end-stage liver disease including cirrhosis was five times higher than chronic liver disease without cirrhosis.11 Previous reports of population-based prevalence rates of cirrhosis in Nakhon Nayok Province showed that standardized prevalence rates are 75.3 per 100,000, and prevalence is higher among males than females, particularly for alcoholic cirrhosis.12
Health-financing reforms in Southeast Asia have sought to reduce dependence on out-of-pocket payments, increase pooled health finance, and expand service use as steps towards universal coverage.13 Thailand developed a universal coverage public health care system in 2002.14,15 All citizens received individualized national insurance depending on work and public health classification to ensure basic health care services. Outcomes, economic burden, and the effect of the public health care system of cirrhosis in Thailand have not been well researched. We aim to evaluate the burden of illness associated with cirrhosis in Thailand and its effect on the national health insurance systems.
Material and MethodsData sourcesWe analyzed cirrhosis data among hospitalized patients in Thailand from the 2010 Nationwide Hospital Admission Data, the National Health Security Office (NHSO), Thailand. Data consisted of inpatient information from three health insurance coverage schemes (Medical Welfare Scheme, MWFS, Social Security Scheme, SSS, and Civil Servant Medical Benefit Scheme, CSMBS), which covered 77% (MWFS), 10% (SSS), and 13% (CSMBS) of all admissions. All patients with cirrhosis diagnosis (ICD10-K74) aged at least 19 years old were included. Their baseline characteristics, hospital costs, and outcomes were analyzed according to national health insurance category.
Universal coverage public health care systemThailand adopted a universal public health care system in 2002, which is comprised of three national health insurance categories -Civil Servant Medical Benefit Scheme (CSMBS), Social Security Scheme (SSS), and Medical Welfare Scheme (MWFS). CSMBS includes all civil servant officers with close family which individually reimburses medical expenses from the Controller General’s Department. SSS includes all Thai employees who are registered to the National Social Security Fund. MWFS includes all the remaining Thai citizens in the national database, which can access public health services from public hospitals and private hospital registered with The National Health Security Office. All national health insurances cover basic healthcare services, however there are some differences between them. CSMBS covers some medications that are part of the National List of Essential Medicines, and liver transplant, whereas other schemes do not cover this. There are also some differences in hospital room fee reimbursement rules among these insurances.
In Thailand, government hospitals are classified into three levels, primary hospital is community hospital for primary healthcare, secondary hospital is a hospital for general healthcare, and tertiary hospital is a referral hospital for complicated diseases and specialized healthcare.
Statistical analysisAll statistical analyses were performed using SPSS version 13 (SPSS Inc., Chicago, IL). Continuous variables were compared between groups using unpaired t-test and one-way ANOVA. Categorical variables were compared between groups using χ 2/Fisher’s exact test. Multiple logistic regression analysis was used to adjust the odds ratio for the factors influencing mortality rate. The odds ratio and 95% CI of each factor are presented. P < 0.05 was considered statistically significant.
Ethical considerationThis study was done with approval from The Gastroenterological Association of Thailand in collaboration with The National Health Security Office, Thailand. The research protocol was approved by the Institutional Review Board, Faculty of Tropical Medicine, Mahidol University (MUTM 2014-056-01).
ResultsIn the year 2010, Thailand’s over 19-year-old population was 47.97 million, which accounted for 74% of the country’s population (64.7 million). The total number of adult inpatients was 3.87 million, who were admitted 4.86 million times, accounting for 71% of all inpatients. The diseases of digestive system were the third leading cause of hospitalization, which accounted for 379,532 admissions, or 10% of all admissions. Among admissions of digestive system, 92,301 admissions for cirrhosis (24.3%) were eligible for analysis.
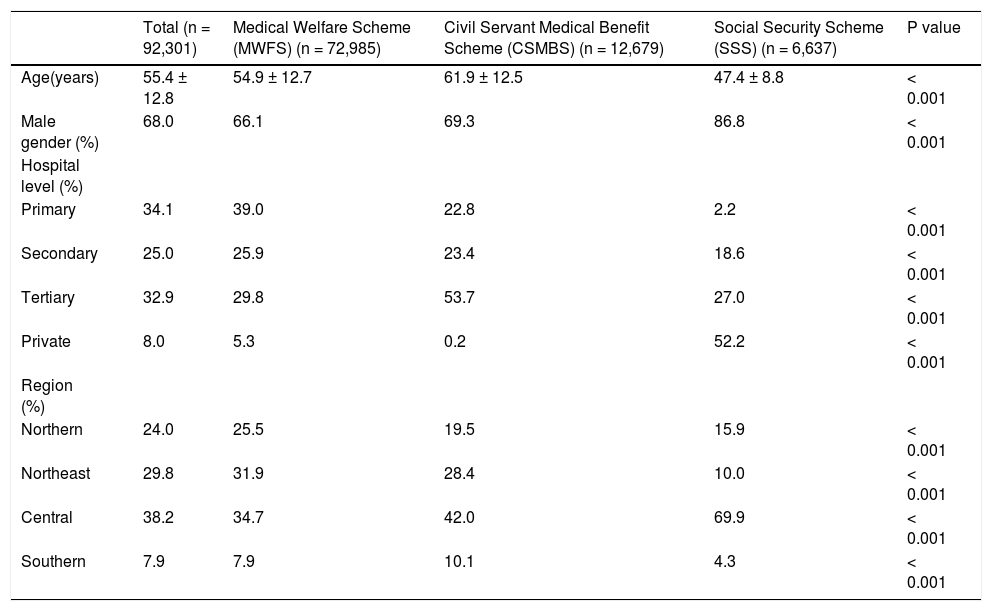
The mean age of patients admitted with cirrhosis was 55 ± 12.8 years and 63.3% of patients were above 50 years old. The male to female ratio was 2:1, most patients were hospitalized in primary level hospitals, and in the central part of Thailand. The majority of patients (79%) belonged to the group of MWFS (Table 1).
Baseline characteristics, hospital level and geographic distribution of cases were classified according to their national health insurance.*
| Total (n = 92,301) | Medical Welfare Scheme (MWFS) (n = 72,985) | Civil Servant Medical Benefit Scheme (CSMBS) (n = 12,679) | Social Security Scheme (SSS) (n = 6,637) | P value | |
|---|---|---|---|---|---|
| Age(years) | 55.4 ± 12.8 | 54.9 ± 12.7 | 61.9 ± 12.5 | 47.4 ± 8.8 | < 0.001 |
| Male gender (%) | 68.0 | 66.1 | 69.3 | 86.8 | < 0.001 |
| Hospital level (%) | |||||
| Primary | 34.1 | 39.0 | 22.8 | 2.2 | < 0.001 |
| Secondary | 25.0 | 25.9 | 23.4 | 18.6 | < 0.001 |
| Tertiary | 32.9 | 29.8 | 53.7 | 27.0 | < 0.001 |
| Private | 8.0 | 5.3 | 0.2 | 52.2 | < 0.001 |
| Region (%) | |||||
| Northern | 24.0 | 25.5 | 19.5 | 15.9 | < 0.001 |
| Northeast | 29.8 | 31.9 | 28.4 | 10.0 | < 0.001 |
| Central | 38.2 | 34.7 | 42.0 | 69.9 | < 0.001 |
| Southern | 7.9 | 7.9 | 10.1 | 4.3 | < 0.001 |
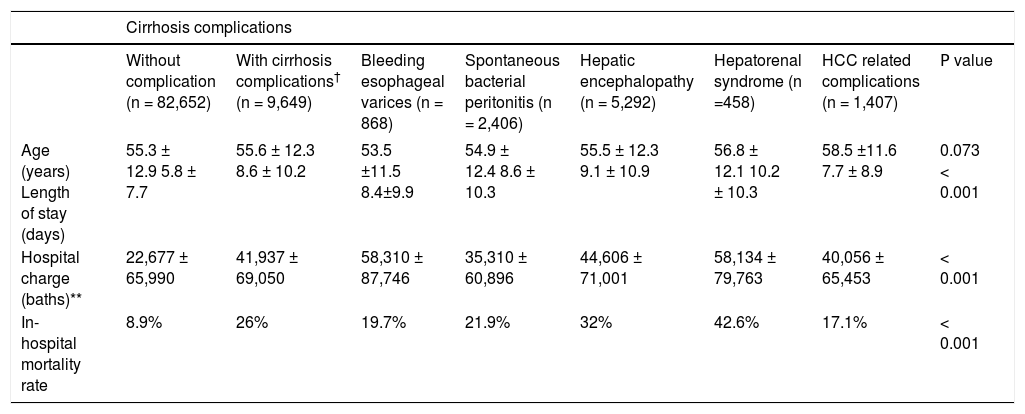
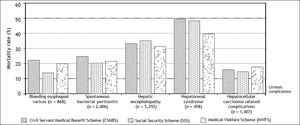
The overall in-hospital mortality was 10.7%. Cirrhotic patients with complications including bleeding esophageal varices, spontaneous bacterial peritonitis, hepatic encephalopathy, hepatorenal syndrome, and hepatocellular carcinoma-related complications had significantly higher mortality rate than those patients without complications (26 vs. 8.9%, p < 0.001). The overall mean length of hospital stay was 5.8 days in cirrhosis patients. Longer durations, up to 8.6 days, were observed in patients with cirrhosis complications. Hepatorenal syndrome was the complication that caused the longest admission period, up to 10.2 days, and the highest mortality rate, up to 42.6% (Table 2).
Baseline characteristic, duration of hospital stay, cost of hospitalization, and mortality rate classified according to complications directly related with cirrhosis.*
| Cirrhosis complications | ||||||||
|---|---|---|---|---|---|---|---|---|
| Without complication (n = 82,652) | With cirrhosis complications† (n = 9,649) | Bleeding esophageal varices (n = 868) | Spontaneous bacterial peritonitis (n = 2,406) | Hepatic encephalopathy (n = 5,292) | Hepatorenal syndrome (n =458) | HCC related complications (n = 1,407) | Ρ value | |
| Age (years) Length of stay (days) | 55.3 ± 12.9 5.8 ± 7.7 | 55.6 ± 12.3 8.6 ± 10.2 | 53.5 ±11.5 8.4±9.9 | 54.9 ± 12.4 8.6 ± 10.3 | 55.5 ± 12.3 9.1 ± 10.9 | 56.8 ± 12.1 10.2 ± 10.3 | 58.5 ±11.6 7.7 ± 8.9 | 0.073 < 0.001 |
| Hospital charge (baths)** | 22,677 ± 65,990 | 41,937 ± 69,050 | 58,310 ± 87,746 | 35,310 ± 60,896 | 44,606 ± 71,001 | 58,134 ± 79,763 | 40,056 ± 65,453 | < 0.001 |
| In-hospital mortality rate | 8.9% | 26% | 19.7% | 21.9% | 32% | 42.6% | 17.1% | < 0.001 |
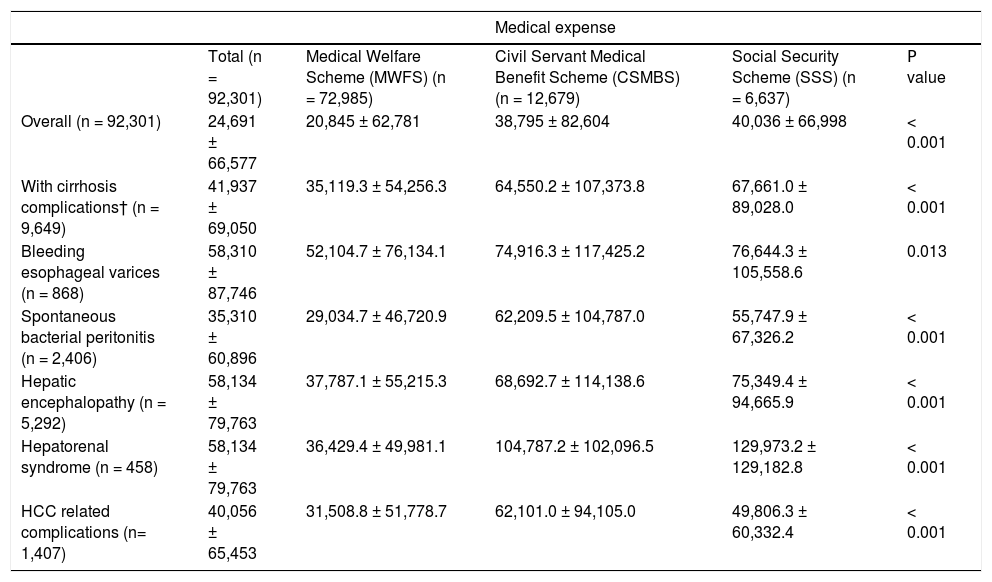
Cirrhosis patients in the group of MWFS incurred the least medical expense compared to those in the SSS and CSMBS groups - both for patients with and without complications. After categorizing according to cirrhosis complications including bleeding esophageal varices, spontaneous bacterial peritonitis, hepatic encephalopathy, hepatorenal syndrome and hepatocellular carcinoma-related complications, the MWFS group still incurred a significantly lower medical expense (Table 3).
Medical expenses classified by cirrhosis complications and national health insurance.*
| Medical expense | |||||
|---|---|---|---|---|---|
| Total (n = 92,301) | Medical Welfare Scheme (MWFS) (n = 72,985) | Civil Servant Medical Benefit Scheme (CSMBS) (n = 12,679) | Social Security Scheme (SSS) (n = 6,637) | Ρ value | |
| Overall (n = 92,301) | 24,691 ± 66,577 | 20,845 ± 62,781 | 38,795 ± 82,604 | 40,036 ± 66,998 | < 0.001 |
| With cirrhosis complications† (n = 9,649) | 41,937 ± 69,050 | 35,119.3 ± 54,256.3 | 64,550.2 ± 107,373.8 | 67,661.0 ± 89,028.0 | < 0.001 |
| Bleeding esophageal varices (n = 868) | 58,310 ± 87,746 | 52,104.7 ± 76,134.1 | 74,916.3 ± 117,425.2 | 76,644.3 ± 105,558.6 | 0.013 |
| Spontaneous bacterial peritonitis (n = 2,406) | 35,310 ± 60,896 | 29,034.7 ± 46,720.9 | 62,209.5 ± 104,787.0 | 55,747.9 ± 67,326.2 | < 0.001 |
| Hepatic encephalopathy (n = 5,292) | 58,134 ± 79,763 | 37,787.1 ± 55,215.3 | 68,692.7 ± 114,138.6 | 75,349.4 ± 94,665.9 | < 0.001 |
| Hepatorenal syndrome (n = 458) | 58,134 ± 79,763 | 36,429.4 ± 49,981.1 | 104,787.2 ± 102,096.5 | 129,973.2 ± 129,182.8 | < 0.001 |
| HCC related complications (n= 1,407) | 40,056 ± 65,453 | 31,508.8 ± 51,778.7 | 62,101.0 ± 94,105.0 | 49,806.3 ± 60,332.4 | < 0.001 |
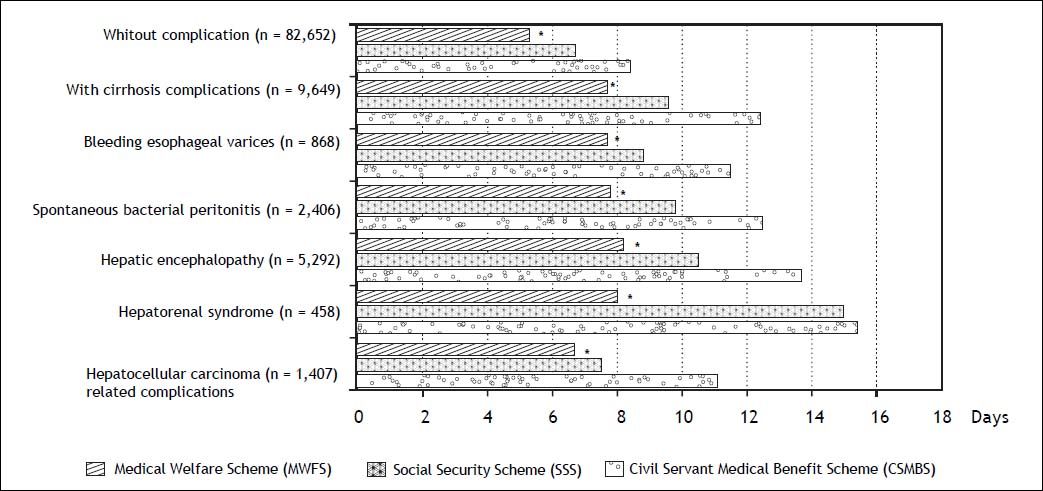
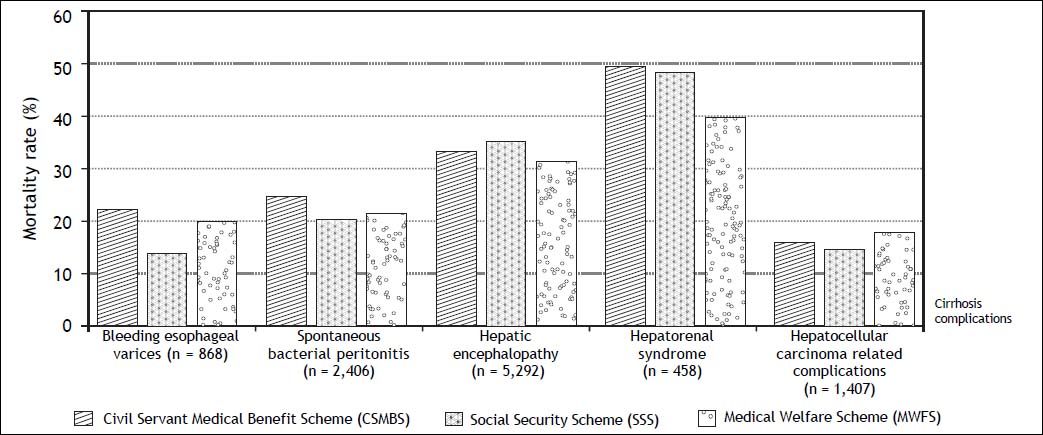
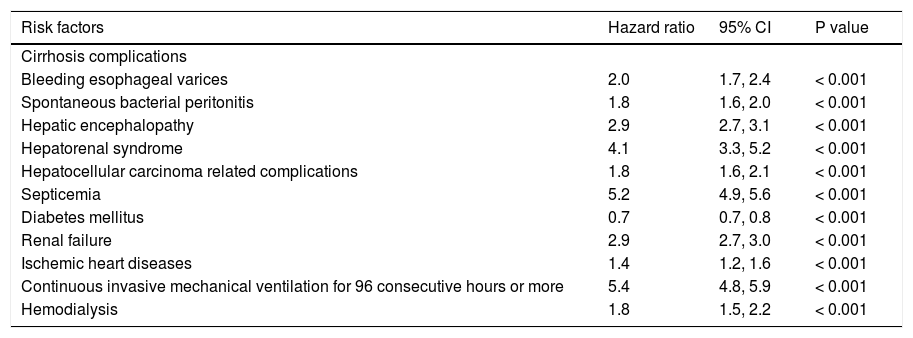
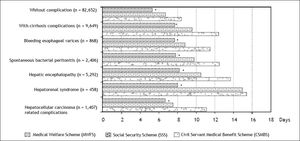
Cirrhosis patients in the MWFS group had significantly shorter admission durations compared to the SSS and CSMBS groups, despite cirrhosis complications (Figure 1). In-hospital mortality of patients with cirrhosis complications did not differ among the three groups (Figure 2). Comorbidities and cirrhosis complications were significantly correlated with patient survival. Respiratory failure requiring continuous invasive mechanical ventilation for 96 consecutive hours or more, and septicemia were associated with the highest risk of death (HR 5.4; 95% CI: 4.8-5.9 and HR 5.2; 95% CI: 4.9-5.6 respectively; P<0.001) (Table 4).
Cirrhosis complications and co-morbidities associated with in-hospital mortality in patients hospitalized with liver cirrhosis.
| Risk factors | Hazard ratio | 95% CI | P value |
|---|---|---|---|
| Cirrhosis complications | |||
| Bleeding esophageal varices | 2.0 | 1.7, 2.4 | < 0.001 |
| Spontaneous bacterial peritonitis | 1.8 | 1.6, 2.0 | < 0.001 |
| Hepatic encephalopathy | 2.9 | 2.7, 3.1 | < 0.001 |
| Hepatorenal syndrome | 4.1 | 3.3, 5.2 | < 0.001 |
| Hepatocellular carcinoma related complications | 1.8 | 1.6, 2.1 | < 0.001 |
| Septicemia | 5.2 | 4.9, 5.6 | < 0.001 |
| Diabetes mellitus | 0.7 | 0.7, 0.8 | < 0.001 |
| Renal failure | 2.9 | 2.7, 3.0 | < 0.001 |
| Ischemic heart diseases | 1.4 | 1.2, 1.6 | < 0.001 |
| Continuous invasive mechanical ventilation for 96 consecutive hours or more | 5.4 | 4.8, 5.9 | < 0.001 |
| Hemodialysis | 1.8 | 1.5, 2.2 | < 0.001 |
The etiology of liver cirrhosis was identified in 31,423/92,301 (34%) of cases. Out of these, the causes were identified as alcoholic liver disease in 73%, chronic hepatitis B in 14%, chronic hepatitis C in 12.6%, and non-alcoholic steatohepatitis (NASH) in < 1%.
DiscussionIn 2010, cirrhosis accounted for 1.3 million deaths around the world, about 2% of global deaths.16 According to the National Center for Health Statistics (NCHS), chronic liver disease and cirrhosis is the 12th leading cause of death in the United States. The highest risk groups consist of persons aged 45 to 54 years and 55 to 64 years, where chronic liver disease and cirrhosis are the 4th and 7th leading cause of death.4,17
Our data supports that liver cirrhosis is a public health problem in all areas and at every hospital level in Thailand. Mortality rate of hospitalized liver cirrhosis patients in Thailand 2010 was 10.7%, compared to the overall mortality rate of inpatients of 4.4, 1.4 and 3.3% in CSMBS, SSS, and MWFS groups accordingly. In analysis of data from the National Health Security Office (NHSO), Thailand (2010), cirrhosis-related deaths was 20.5/100,000 persons which is comparable to estimated liver-related deaths in United State (25.7/100,000 persons in 2008).4 Mortality rates of hospitalized cirrhosis patients range from 3.3 to 40% depended on severity of cirrhosis, complications, and co-morbidities.5,18,19 Cirrhosis complications significantly increase risk of death. According to our data, hepatorenal syndrome was the most fatal complication of cirrhosis, which might be due to decompensated liver disease and insufficient liver transplantation. We found that only 19 liver transplants have been done in this registry data, compare with more than 2,500 endoscopic interventions for bleeding esophageal varices. Our data were consistent with previous data, and show that infectious and renal complications in persons with cirrhosis directly impact clinical outcomes.20,21 These data support that morbidity and mortality due to cirrhosis and its complications are significant public health problems in Thailand.
Length of hospital stay and hospital expenses incurred were higher in SSS and CSMBS groups, compared with MWFS, however no statistically significant differences were found in mortality rates from the various cirrhosis complications.
Acute-on chronic liver failure (ACLF) is distinct from acute decompensation and has been significantly related to death in patients with cirrhosis.22 This study has limitations, since it is related to a retrospective survey, and non-specialized doctors are more prone to describe all morbid events in cirrhosis as decompensation. The absence of data description on ACLF does not mean that these cases are rare. Etiology of cirrhosis could only be determined in 34% of cases, and a better method to define etiology of cirrhosis in Thailand should be developed, since its treatment and prevention is essential for better patient care.
Base on this limited data, alcoholic liver disease might be one of the significant causes of liver cirrhosis consistent with previous report,23 however out-patient data from the liver clinic in King Chulalongkorn Memorial hospital, Thailand, showed that chronic hepatitis B was the most common etiology (44.7%), followed by chronic hepatitis C (29.7%), alcoholic liver disease (14.8%), NASH (6.7%), and autoimmune hepatitis(4.1%) (unpublished data). These data suggest that most alcoholic patients did not access healthcare before admission from cirrhosis-related illness.
Alcohol consumption, viral hepatitis B and C, and metabolic syndromes related to overweight and obesity are the leading causes of cirrhosis and primary liver cancer.24–26 Prevention and treatment interventions in those conditions and risk factors are necessary to control further morbidities, mortality, and economic burden related to cirrhosis.
In conclusion, illness associated with cirrhosis is a significant public health problem in Thailand, with a mortality rate of up to 26% in hospitalized patients with decompensated forms of cirrhosis. Preventive measures are very important to reduce the burden of the disease in the future. Although differences among the three health care systems were found regarding medical expenses and admission periods, the outcomes of cirrhosis complications were similar for all of them.
Abbreviations- •
CI: confidence interval.
- •
CSMBS: civil servant medical benefit scheme.
- •
HCC: hepatocellular carcinoma.
- •
HR: hazard ratio.
- •
MWFS: medical welfare scheme.
- •
NASH: non-alcoholic steatohepatitis.
- •
NCHS: National Center for Health Statistics.
- •
NHSO: National Health Security Office.
- •
SSS: social security scheme.
No potential conflict of interest relevant to this article was reported.
Financial SupportThis work was supported by the Gastroenterological Association of Thailand, The ICTM Grant of the Faculty of Tropical Medicine, Mahidol University, Thailand.
AcknowledgementsWe would like to express our gratitude to the staff of the Office of Research Services and staffs at the Faculty of Tropical Medicine, Mahidol University, Faculty of Medicine, Chulalongkorn University, Clinical Epidemiology Unit, Faculty of Medicine, KhonKaen University, Vichaiyut Medical Center, and The National Health Security Office, Thailand.