Introduction
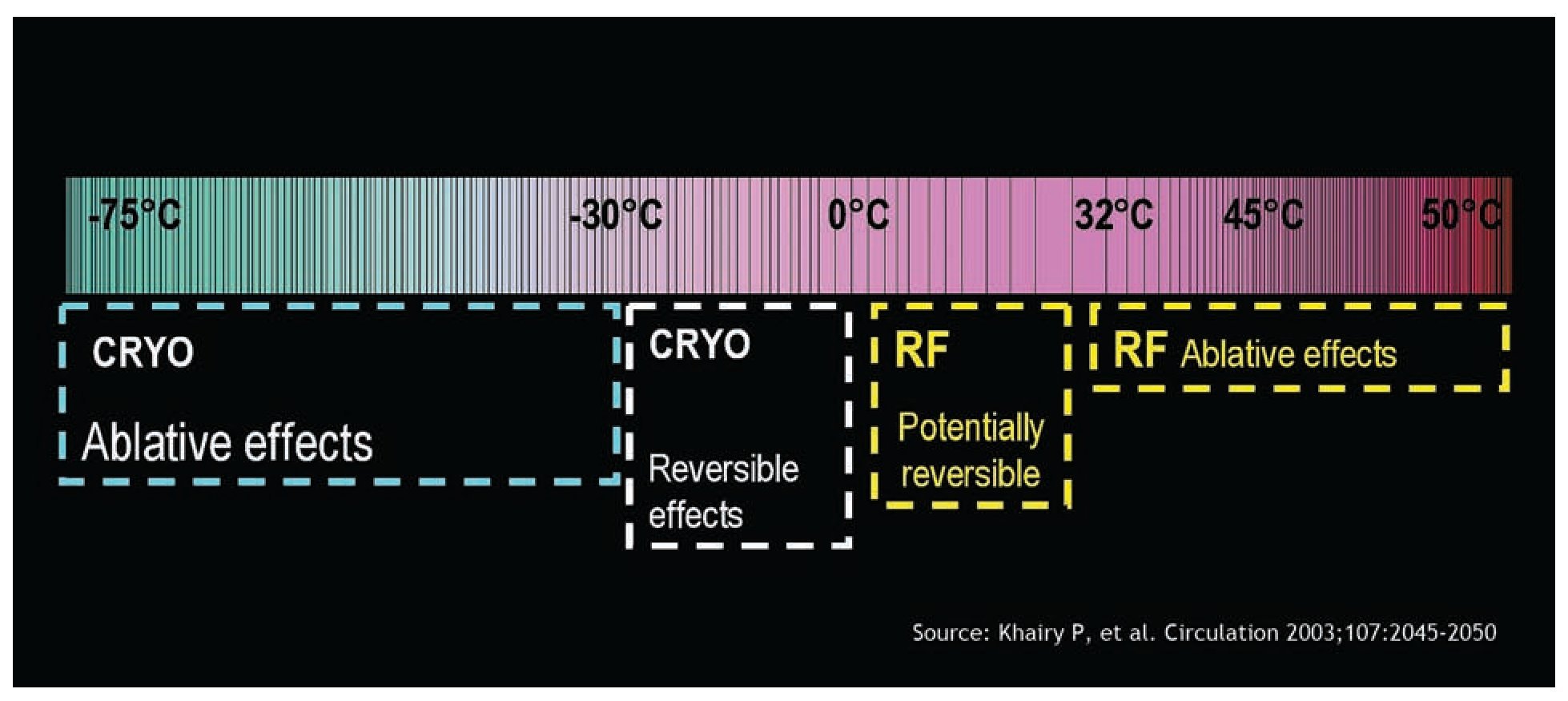
Atrioventricular nodal reentrant tachycardia AV-nodal reentry tachycardia (AVNRT) is one of the most frequent supraventricular tachycardia targeted for endocardial catheter ablation. Although radiofrequency (RF) ablation remains the standard for the treatment of AVNRT worldwide, according to published data a small risk of irreversible complete atrioventricular (AV) block remains.1-3 Particularly in young individuals, physicians and patients may be hesitant to perform RF catheter ablation because of the risk of inadvertent AV block, necessitating implantation of a permanent pacemaker (PM). Cryoablation is a new method in cardiac electrophysiology for percutaneous catheter ablation of cardiac arrhythmias. Cryoablation is an alternative to RF therapy for the treatment of AVNRT without any reported case of permanent AV block.4 The safety profile of cryoablation is also related to the reversibility of the cryothermal effect during cryomapping at -30° C, which allows for the functional assessment of a particular site before permanent cryoablation at - 80° C. In this way, the targeted tissue may be confirmed as safe for ablation. This can be useful in high-risk ablations, for example, next to the His bundle or the compact AV node. In the last decade, several studies have been addressed to AVNRT cryoablation. This article is a review of acute and long-term effects of cryoablation in patients suffering of AVNRT episodes.
Principles of cryoablation
Cryocatheter ablation is performed by using a cryoablation system (CryoCath, Inc.) that consists of a control console and a 7F steerable catheter with a 4- or 6-mm-tip electrode and uses N2O as the refrigerant fluid. The console delivers the refrigerant fluid to the tip of the cryo-catheter through a hollow injection tube. The refrigerant fluid undergoes a phase change (from liquid to gas) at the tip of the cryocatheter, resulting in cooling of the adjacent myocardial tissue. The gas is then removed through a second coaxial tube under vacuum.
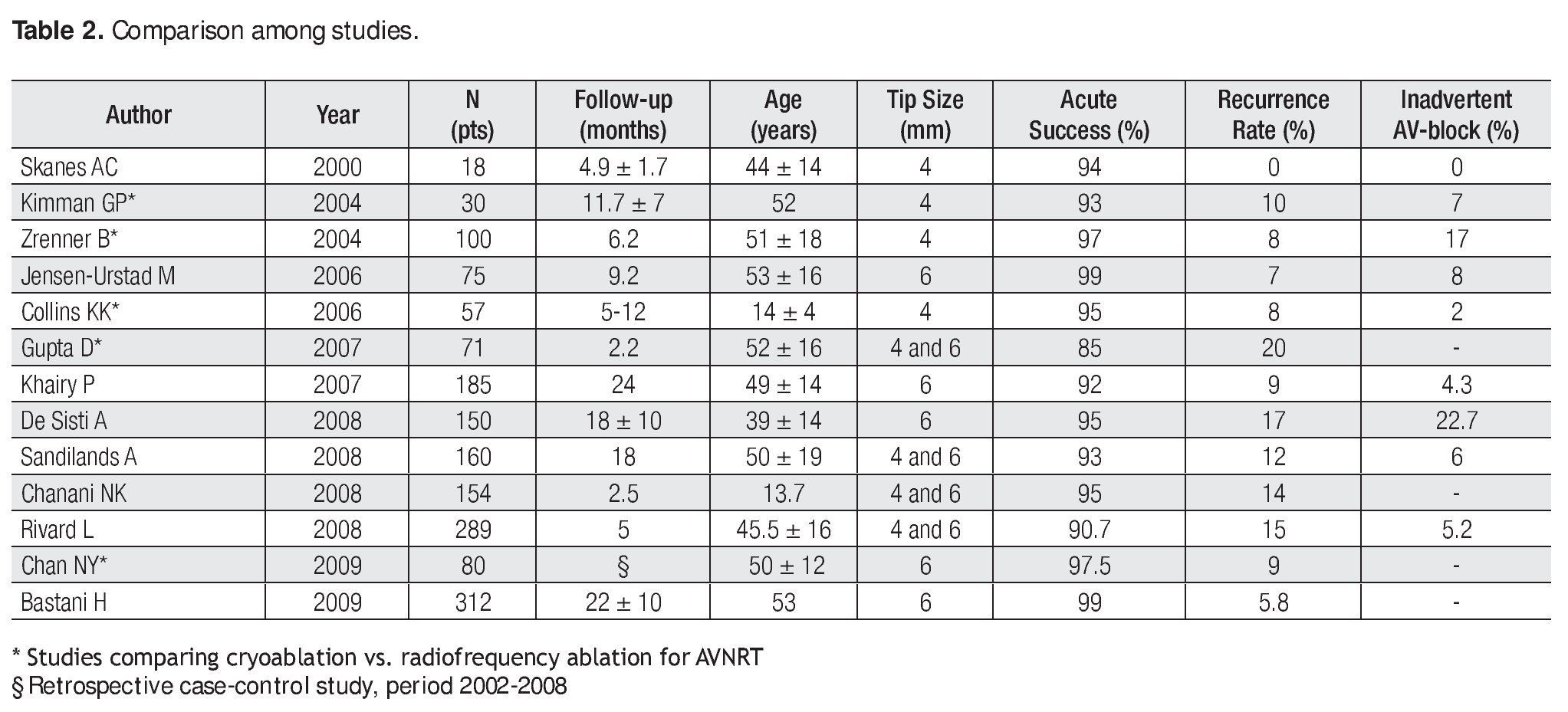
The protocol of cryoablation procedure includes a preliminary cryomapping and a subsequent cryo-applicaction after successful and uncomplicated cryomapping.5 Cryomapping is carried out first at a cryocatheter tip temperature of -30 to -40° C for a maximal duration of 60 s to test the electrophysiological effects on the target site by using programmed stimulation, which reproducibly demonstrated dual nodal physiology or induced AVNRT (Figure 1). In case of ineffective results or AV-block, cryomap-ping is stopped and then repeated at new target sites. Cryoablation, which creates a permanent lesion by cooling the tip temperature to -80° C generally for 4 minutes duration, is initiated immediately following successful cryomapping, defined as block of the slow pathway conduction or the non-inducibility of AVNRT. Programmed stimulation is repeated all the time during cryoablation to confirm the effectiveness of the ablation. If AVNRT is still inducible or AV-block occurs, cryoablation is stopped and cryomapping is repeated at a new target site. It is important to mention that, in contrast with radiofrequency catheter ablation of AVNRT, cryotherapy did not incluce ectopic rhythms.5
Figure 1. RF: radiofrequency; CRYO: cryoenergy.
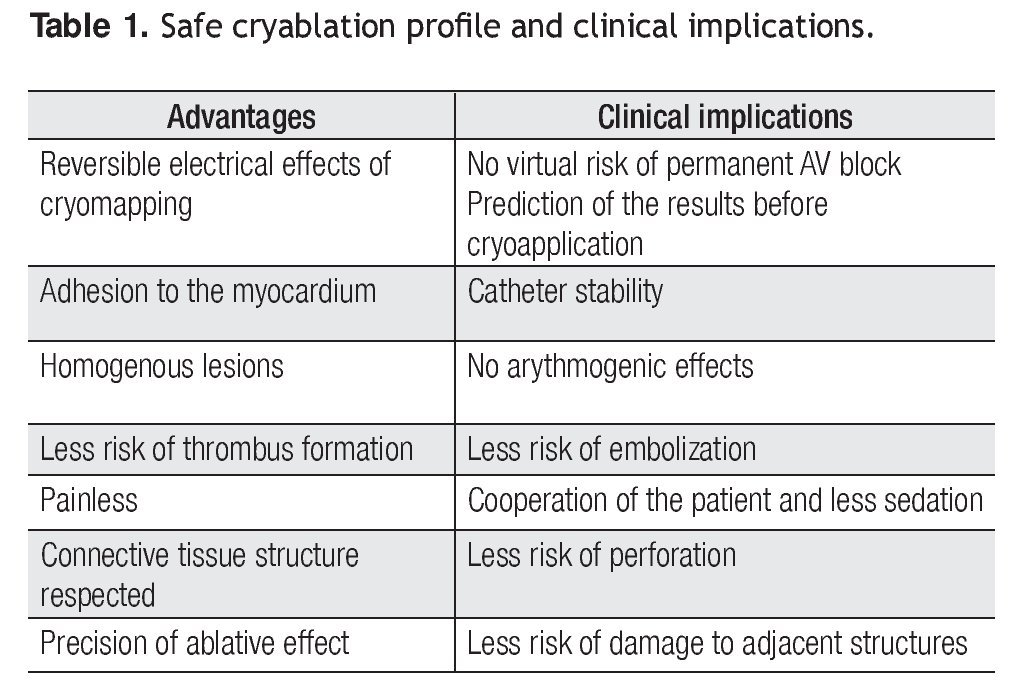
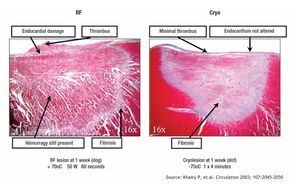
Advantages of cryoablation
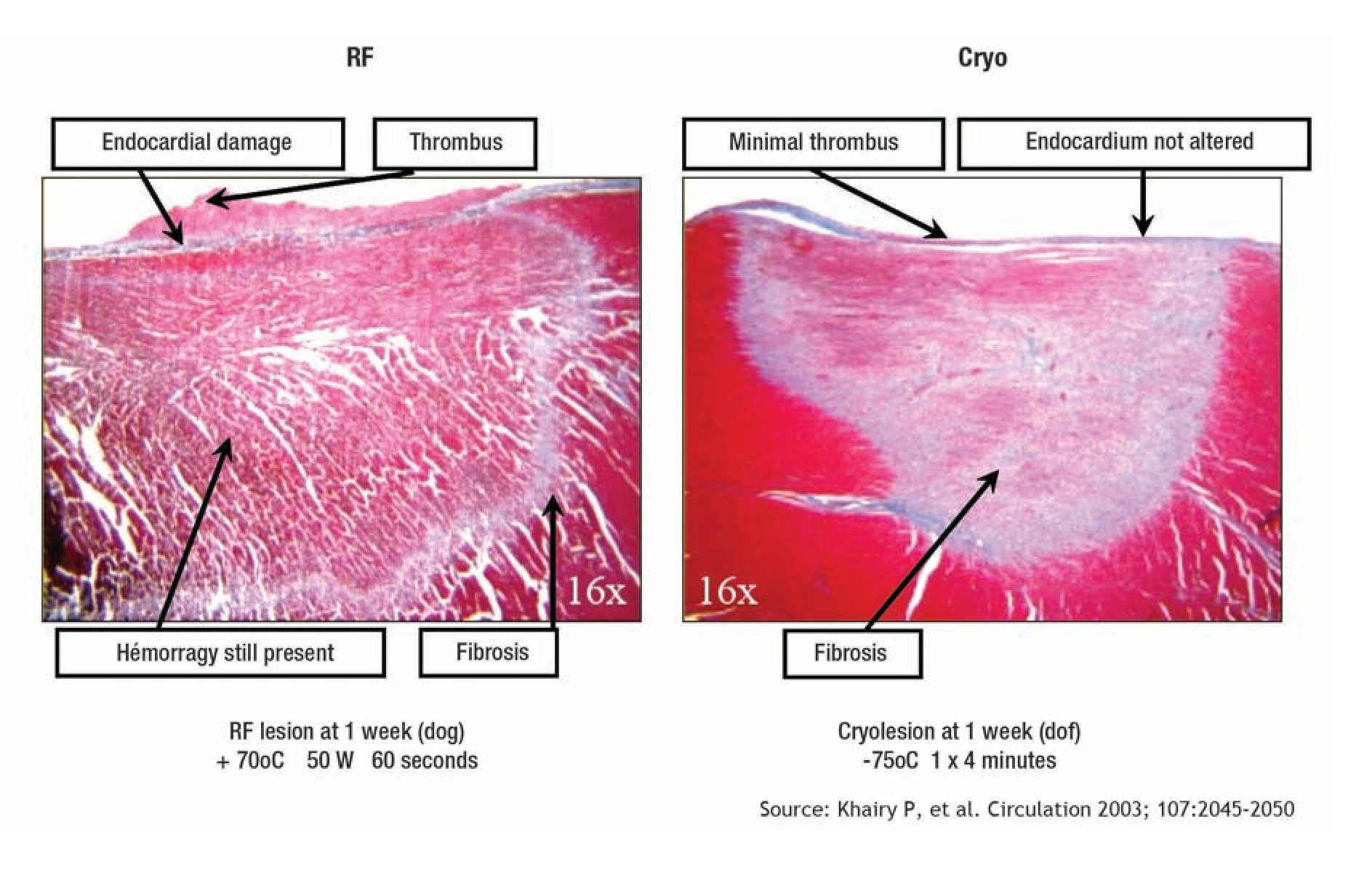
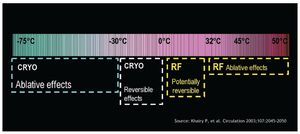
Contrarily to RF, during cryomapping and cryoablation the cryocatheter tip adheres to the myocardial tissue because of ice formation. In comparison to RF, cryoablation induces less endothelium and connective tissue damages, limiting thrombi generation, as well as the risk of cardiac perforation and tamponade.5,6 The adjacent structures like artery or vein vessels or the esophagus are preserved by the cryotechnique (Figure 2). Contrarily to RF, cryoablation is painless, which reduces the need of anesthesia and sedation (Table 1).
Figure 2. RF: radiofrequency; CRYO: cryoenergy
Clinical results of cryoablation for AVNRT
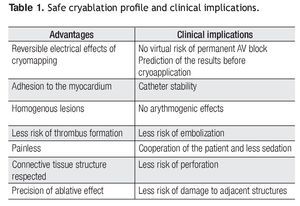
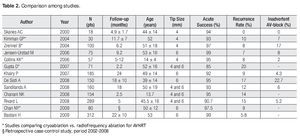
Cryoablation for AVNRT has been the object of numerous published studies in the last decade.4-21 Preliminary experiences have been conducted using a 4-mm tip catheter, nowadays employed especially in pediatric patients. In one of these first reports, Kimman et al,8 compared acute and long-term effects of RF and cryoablation in a prospective, randomized trial enrolling 102 patients with AVNRT. Procedural success using a 4-mm-tip catheter was identical between the two groups (91% and 93%, respectively) with similar fluoroscopy and procedural times. Long-term clinical success was also comparable showing 10% of recurrences in both groups. Similar results have been reported by Zrenner et al.9 in 200 patients randomly assigned to RF or cryoablation. Acute success rate was 97%, similar to that of RF. Nevertheless, recurrence rate was significantly higher in cryoablation patients than in the RF group (1% vs. 10%; p < 0.03). Subsequently, several studies have been published enrolling solely patients undergoing cryoablation, and mainly using a 6-mm-tip catheter.4.10-21 Globally, acute procedural success rate for AVNRT cryoablation reported in the literature ranges from 85% to 99% (Table 2), not so far from acute success described in RF series.1-3 In studies using RF the incidence of recurrence was low (3% to 5%), but permanent AV-block with a PM implantation has been reported to be from 1% to 2% in experimented centers.1-3 Overall, recurrence rate in studies involving cryoablation ranged from 7% to 20% (Table 2), higher than with RF catheter ablation. These inhomogeneous long-term results reported in cryoablation series could be explained by several reasons, like different cryocatheter size,4,16,17 patients age,22 inclusion of patients with complex anatomy,4 as well as different follow-up duration. Additionally, most of these studies have been planned without a control group of patients treated with RF. However, two recent non-randomized studies,13,18 in which a 6-mm cryocatheter was used, confirmed that acute success rate was similar between cryoablation and RF but recurrence rate was significantly higher with cryoablation.
Long-term predictive criteria
Some authors focused on long-term predictive criteria in AVNRT cryoablation patients. There are some evidences that a 6-mm-tip cryocatheter is superior to a 4-mm-tip in long-term results.4,16,17 Rivard et al,17 found that cryoablation with a 4-mm-tip catheter, when compared with 6-mm-tip, is associated with a 2.5-fold increased risk of arrhythmia recurrence during the follow-up. Sandilands et al,15 found that complete anterograde slow pathway conduction suppression is associated with long-term clinical success. However, residual persistence of slow pathway conduction has not been found as a predictor of AVNRT recurrence by other authors.4,14,16 Experimentally, a freezing-thawing-freezing cycle has been described to be associated with more extensive lesions.23 Whereas some authors21 described in pediatric patients a long-term better effect of a "bonus" cryo-application at the effective site, others4,14 did not observe any significant effect in adults.
Inadvertent AV-block during cryoablation
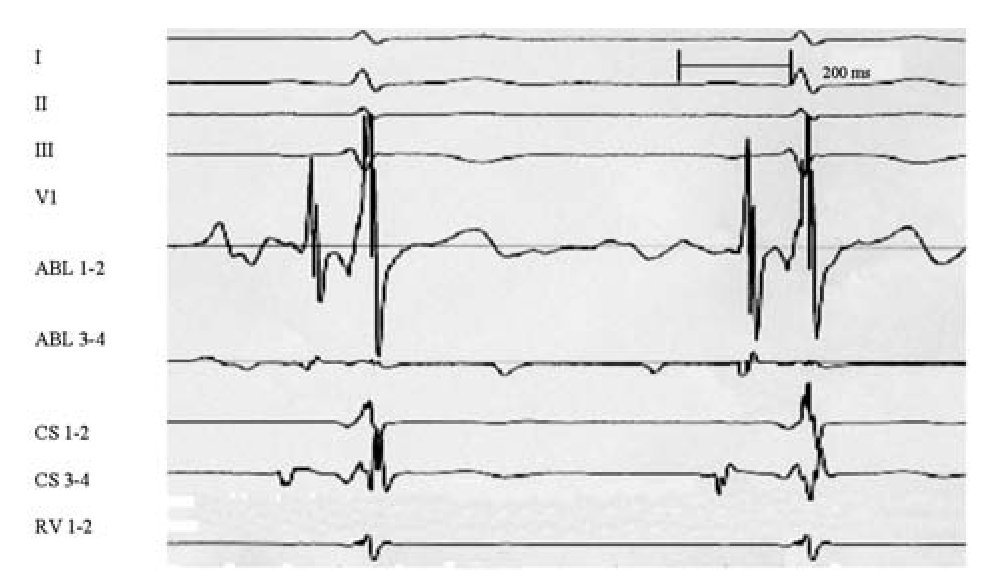
Up to now, to our knowledge, no case of complete AV-block necessitating PM implant after cryoablation has been reported in the literature although this complication can be possible. Nevertheless, inadvertent AV-block, preceded by preliminary successful and uncomplicated cryomapping, ranges between 7% and 23%, when including also unwanted fast pathway lesion with PR prolongation (Table 2). Despite that AV-block occurrence was not uncommon, AV conduction rapidly recovered with tissue warming in all series describing this complication (Figure 3). In a study of De Sisti et al,4 all AV blocks occurring during cryoablation were transient, confirming the safety profile of cryoablation. After cryoablation interruption, 2nd - 3rd AV-block lasted generally few seconds, while 1st degree AV-block sometimes persisted, but AV conduction recovered after hours or some days (up to 4 days) in these patients. However, inadvertent fast pathway lesion with residual permanent 1st degree AV-block has been recently described, but these patients underwent multiple ablation procedures and presented a small Kock's triangle.24 Thus, adverse but still reversible effects on AV conduction may be observed during cryoablation in spite of the lack of previous deleterious effects of cryomapping. As underlined by Fischbach,25 this experience demonstrates that the cryolesion created during cryoablation may expand relative to that suggested by cryomapping.
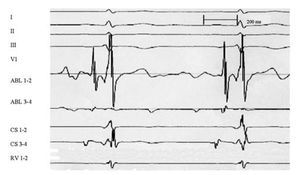
Figure 3. Example of inadvertent AV-block during cryoablation. Despite a successful and uncomplicated preliminary cryomapping (-30° C), 10 sec from the beginning of the cryoablation at -80° C, a 2/1 AV-block appeared. AV-block was transient, followed by complete AV recovery few seconds later. I, II, V1: surface ECG leads; ABL: ablation catheter; HIS: His catheter; CS: coronary sinus catheter.
Clinical implications
It has been assumed that the cornerstone of cryotechnology is the capability to test its effect by creating a reversible lesion at a less critical temperature (-30 to -40° C) and, thereby, assessing a risk of AV-block. Cryoadherence prevents dislodgement of the catheter tip and therefore avoids unwanted energy delivery at the compact AV node or His bundle. Junctional ectopy, a sensitive marker of successful RF ablation,26 does not occur during cryoablation, which can facilitate monitoring during ablation. If this is the case, there will be a significant proportion of patients, especially young ones and those with particular AV node anatomy, in whom a less efficacious action may be preferred over the risk of needing a PM implantation, a disastrous event in the young population. However, inadvertent AV-block can occur despite an uncomplicated cryomapping. It has been observed in an animal model that the minimal application of cryoenergy to achieve complete nodal AV-block is of 10 sec in duration.27 These data stress the need for a careful attention when ablating with cryoenergy instead of RF. Nevertheless, cryoablation's safe profile is counterbalanced by a slightly higher recurrence rate of arrhythmias during the follow-up.
Procedural target, anatomic sites, and markers of successful ablation are not the same between cryoablation and RF. Atrio/ventricular amplitude ratio at successful target when using cryoablation tends to be higher (Figure 4) than that usually recommended when employing RF. Absence of junctional rhythm during cryoablation facilitates fast pathway monitoring, whereas during RF it constitutes a common accepted marker of success.
Figure 4. Note on ABL 1-2 the slow pathway potential and an atrio/ventricular amplitude ratio of about 1 recorded at the successful site before cryoapplication, slightly above the coronary sinus ostium. Procedural target, anatomic sites and markers of successful ablation are not the same between cryoablation and RF. Atrio/ventricular amplitude ratio at successful target when using cryoablation tends to be higher than that usually recommended when employing RF. I, II, III, V1: surface ECG leads; ABL: ablation catheter; CS: coronary sinus catheter; RV: right ventricle.
Recurrence rate seems to be lower along the learning curve effect, and the use of 6-mm-tip catheters. Finally, a limitation for a widespread use of cryocatheters is their cost, which is higher in France than catheters commonly used in RF.
Conclusions
Current experiences indicate that cryoablation for AVNRT is effective and safe. However, its use seems to be counteracted by a slightly lower long-term efficacy when compared to radiofrequency. Further studies evaluating long-term success of cryoablation versus radiofrequency are warranted. However, for high-risk ablations, cryoenergy is very helpful and should be systematically used.
Correspondence author: Joelci Tonet,
Hôpital de La Pitié-Salpêtrière, Institut de Cardiologie, Unité de Rythmologie, 47-83. Boulevard de l'Hôpital, 75651 Paris, France.
Fax: 33142163057.
E-mail:joelci.tonet@psl.aphp.fr
Received on March 19, 2010;
accepted on September 19, 2010.