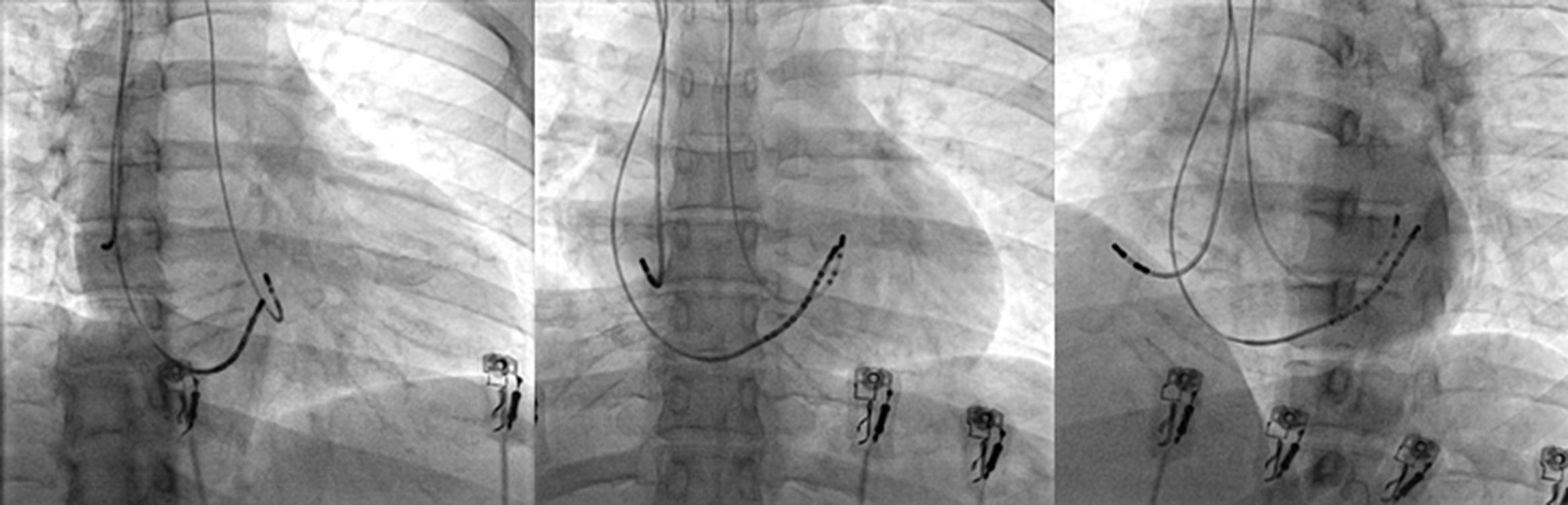
In cardiology, the current trend regarding invasive procedures is to maximize patients’ comfort without compromising their safety. This is the reason why, in some centers, radial artery puncture is the preferred approach for both coronary angiogram and angioplasty procedures as opposed to femoral access, due to fewer rates of complications.1 While performing electrophysiology (EP) procedures we often saw ourselves in the need to use several catheters in order to demonstrate the different pathways involved in the development of a tachycardia. However, nowadays this is not necessary for the vast majority of simple EP procedures. Others groups and we believed that with one or at most three catheters is enough to perform basic EP studies as well as ablations,2,3 allowing us to explore other vascular approaches instead of the traditional femoral access (Fig. 1). The latter could represent a practical alternative especially in patients in whom the femoral access is hard to find due to a variety of conditions such as obesity, tortuosity or vein occlusion, thereby allowing the patient to move soon after the surgery rather than lying in bed for a long period of time. The jugular and subclavian approaches had been suggested as alternative means to ablate anteroseptal accessory pathways, for both first intervention or recurrences.4–6 Also by using these alternative accesses we can achieve an ambulatory EP procedure discharging the patient just a few hours later, without the need to wait until the next day. Here we describe a case series by systematically using alternative vascular accesses instead of the traditional femoral approach with some novel technical improvements including AV nodal re-entry tachycardia (AVNRT) ablation, which to our knowledge has not been reported previously.
During a 4 month period (from October 2012 to February 2013), 30 patients sent to our center for simple electrophysiological procedures such as: electrophysiological studies (EP), AV nodal ablation or supraventricular tachycardias (SVT) ablation with the exception of typical atrial flutter, were included prospectively and consecutively. Complex arrhythmias such as atrial fibrillation, atypical atrial flutter or ventricular tachycardia, were excluded. Informed consent was obtained from all patients. In order to get vein access, we performed one or two subclavian vein punctures, in the same site, using a 6 and 7Fr introducer sheath for diagnostic and also therapeutic catheters respectively. Artery access was achieved by puncturing the radial artery with a special 6Fr introducer sheath (Terumo Co.). Once the artery patency was assured and the sheath introduced, we administered 2.5mg of verapamil once or twice depending on the presence of vasospasm, and then switch for a 7Fr conventional sheath. After that, 5000U of non-fractioned I.V. heparin were administered. All ablations were performed with a red, blue or orange curve 4mm tip ablation catheter (Biosense Webster Co.).
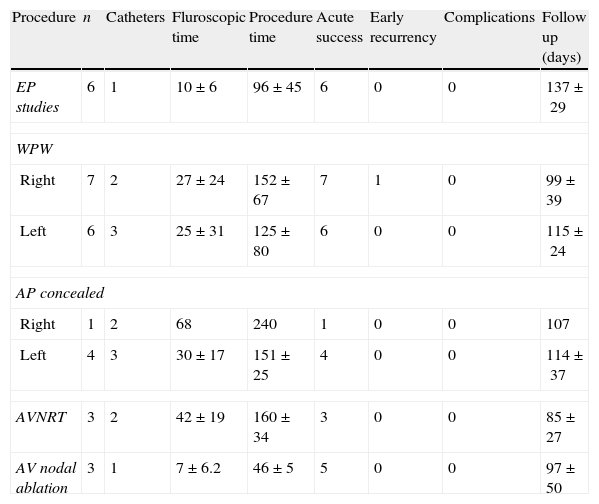
ResultsThirty procedures (6 EP studies and 24 ablations) were completed (Table 1). Patient's mean age was 39±15 years, 60% (18 patients) were males; 5 EP studies were for TV induction in patients with dilated cardiomyopathy after transradial angiography, using only one deflectable diagnostic catheter through the radial artery. The remaining EP study was for treatment of symptomatic non-documented palpitations; in this case, we used 2 catheters through the subclavian vein approach. The ablations were performed to 13 patients with Wolff–Parkinson–White (WPW) syndrome (7 from right and 6 from left origin); 5 patients with a concealed accessory (CA) pathway (1 from right and 4 from left origin); 3 patients with AVNRT and 3 patients with AV nodal ablation for rate control because permanent AF. In those patients with left accessory pathway (10 patients) we used 3 catheters, in 11 patients we used 2 catheters and in 9 patients we used 1 catheter; for the ablation of the left tachycardias we used 3 catheters, for the ablation of right tachycardias we used 2 vein punctures for 2 catheters; also for the EP study we used 2 catheters, and finally we used 1 catheter for ventricular stimulations taking advantage of the prior radial artery puncture for the coronary angiogram. All the ablations were successfully done during the first procedure. Only one patient with a WPW syndrome and Ebstein's anomaly presented an early recurrence within the first 24h after successful ablation. We performed the study again, this time through the femoral access using an irrigated tip catheter. After this second intervention the patient had again an early recurrence, which suggests that regardless of the approach used, this was a very difficult case. The mean follow up was 108±34 days and until now there has not been early or late complications in the subclavian or radial puncture sites. Because there was no previous experience in our center with the use of 7Fr transradial catheters for EP procedures, in the first 5 cases we followed up the radial punctures with arterial Doppler, but thereafter this was not necessary due to the good evolution and the difficulty that represented the follow-up of all patients with this procedure in our center (data not shown). The mean fluoroscopy time was 27±23min, and the procedure duration was 128±69min. There was no significant difference in the duration of our procedures in comparison with the traditional transfemoral ones.
The relationship of the 30 procedures, including diagnosis, time of fluoroscopy, procedure, outcome and follow up.
| Procedure | n | Catheters | Fluroscopic time | Procedure time | Acute success | Early recurrency | Complications | Follow up (days) |
| EP studies | 6 | 1 | 10±6 | 96±45 | 6 | 0 | 0 | 137±29 |
| WPW | ||||||||
| Right | 7 | 2 | 27±24 | 152±67 | 7 | 1 | 0 | 99±39 |
| Left | 6 | 3 | 25±31 | 125±80 | 6 | 0 | 0 | 115±24 |
| AP concealed | ||||||||
| Right | 1 | 2 | 68 | 240 | 1 | 0 | 0 | 107 |
| Left | 4 | 3 | 30±17 | 151±25 | 4 | 0 | 0 | 114±37 |
| AVNRT | 3 | 2 | 42±19 | 160±34 | 3 | 0 | 0 | 85±27 |
| AV nodal ablation | 3 | 1 | 7±6.2 | 46±5 | 5 | 0 | 0 | 97±50 |
The alternative vascular accesses without using the traditional femoral approach are not a novel procedure. There are few communications that have reported yugular or subclavian accesses to perform anteroseptal right accessory pathway ablations6,7 and there are some case reports and systematical ablations of left accessory pathways through transradial artery puncture.8–10 The novelty in our study is that we performed all consecutive EP procedures employing these alternative vascular approaches at all times, including the first AVNR tachycardias and right posteroseptal accessory pathways reported with acute success and without complications. Also we used a 7Fr ablation catheter in all radial procedures, which has been described before but it is not the usual size used due to a possible risk of vasospasm (we did not encounter this complication in our series). The main reason why we decided to find an alternative vascular approach instead of the traditional femoral one is because we wanted to keep the patient's comfort, allowing an early movement; only a few hours after the procedure instead of lying in bed feeling such discomfort this is also the reason why the radial artery via is increasingly used for coronary procedures with excellent outcome. The subclavian vein via is widely used for pacemaker implantation and also it has been reported as an alternative way in those cases with WPW syndrome with an anteroseptal or midseptal right ventricular pathways;5 we choose to use this approach and not the yugular one because we are more accustomed to this via, due to our experience with pacemaker implantations.
In our study no complications in the artery or vein punctures occurred. In the first 5 cases of radial artery puncture patients were followed up with Doppler, but this was not necessary in subsequent procedures due to the good outcome; up to 3% of complications in femoral puncture has been reported, that includes thrombosis, fistula and hemathomas1; we are not excluding the possibility of vascular complications in this alternative approach but, such complications would be the same regardless of the approach used, and probably less for not using the femoral access.9,10
We are aware that with every new technique there is a need for a learning curve, but once it has been reached, the procedures are as easy as the standard technique employed without significantly increasing fluoroscopic or procedure times. In the near future we may use this alternative approach in order to avoid unnecessary and uncomfortable bed rest in those patients with mild or high risk of venous thrombosis; and perhaps we could perform simple EP procedures on an outpatient basis. Nowadays a cardiac electrophysiologist must be trained with the newest techniques available, including transeptal and epicardial puncture or all other available alternatives, in order to perform and securely resolve complex problems for the best interest and outcome of our patients.
Our results demonstrate an alternative approach that is as safe as the customary one for performing simple EP studies and ablations with good acute success rates and without complications.
FundingThere was no funding for this job.
Conflicts of interestThe authors do not have any conflicts of interest.
To the fellows and the people who work in the Department of Electrophysiology and Hemodynamic in the CMN 20 de Noviembre for their support.