Cardiac trauma after blunt chest trauma is a rare complication of patients arriving alive to an emergency department. We here present the case of patient who had a partial rupture of the interventricular septum after having had a blunt chest trauma in a traffic accident. As there was no ventricular septal defect, conservative management was deemed appropriate. At 3-year follow-up, the patient was free of right heart failure symptoms suggestive of the septal defect progression.
El traumatismo cardiaco después de un trauma contuso del tórax es raro en pacientes que sobreviven hasta llegar a un servicio de urgencias. Presentamos el caso de un paciente a quien se le diagnosticó una ruptura parcial del septo interventricular después de un trauma cerrado del tórax en un accidente de tránsito. Debido a que no tenía comunicación interventricular se optó por manejo médico y 3 años después el paciente continuaba sin síntomas de falla cardiaca derecha sugestivos de progresión del defecto anatómico.
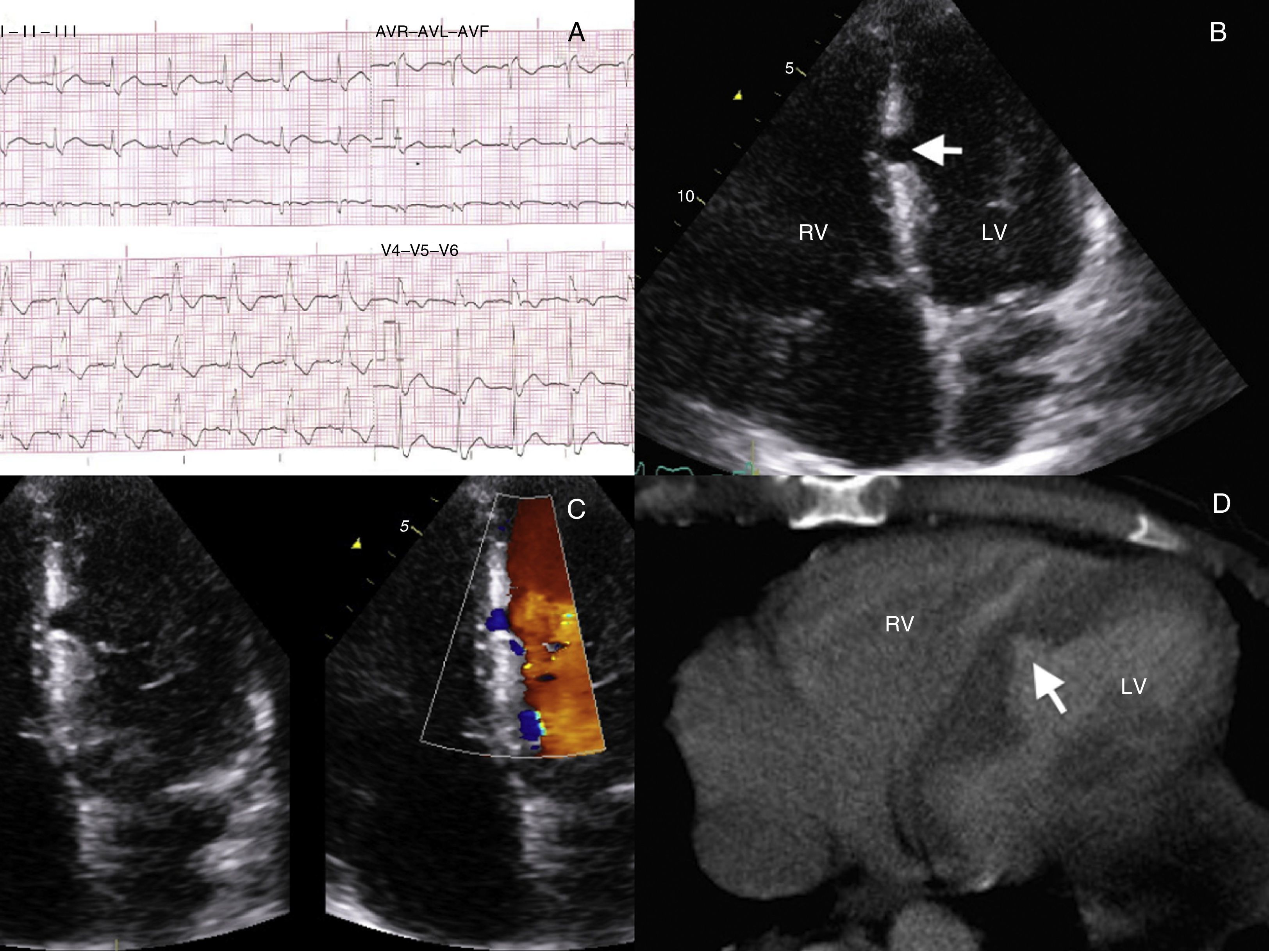
A 39-year-old male was transferred to the hospital after having had an accident in a collision with another motorcycle. On arrival, the patient was found tachypneic, tachycardic, hypotensive, and stuporous. There were signs of head trauma, thoracic contusion, and long bone and pelvic fractures. No serious injuries were seen on a computed tomography (CT) scan of the head but a chest CT scan revealed a bilateral pneumothorax and mediastinal hematoma. Therefore, he underwent further workup to rule-out blunt cardiac injury (BCI). An ECG showed a complete right bundle branch block (Fig. 1A) and troponin I levels were found raised up to 24ng/mL, which prompted to perform an echocardiogram that disclosed a partial rupture of the interventricular septum (PRVS) (Fig. 1B) without evidence of septal defect (VSD) on color Doppler (Fig. 1C). A second review of the chest CT scan also revealed such rupture (Fig. 1D). The patient became stable after tube thoracostomy, surgical fixation of bone fractures, and admission to the intensive care unit for mechanical ventilation. The cardiac surgeon declined any surgical intervention since there was no VSD. At 3-year follow-up, he remains free of symptoms of right ventricular failure. BCI is the cardiac damage resulting from thoracic trauma and should always be entertained as an impending condition in patients with blunt chest trauma. When both ECG and cardiac troponin I are normal at 8h after admission, BCI is certainly excluded.1 However, those patients with persistent hypotension, hypoxemia, heart block or arrythmias warrant an echocardiogram2 in order to rule out pericardial tamponade and valvular or myocardial injury. Although conservative management of PRVS has been previously reported,3 late rupture remains a concern.
(A) Surface ECG showing a complete right bundle branch block. (B) Echocardiography (apical 4 chambers view) displaying an incomplete rupture of the interventricular septum (arrow) at the left side. (C) Zoomed 2D and color Doppler imaging views disclosing no shunt between the left ventricle (LV) and the right ventricle (RV). (D) Close view of the heart on chest CT scan revealing an interventricular septum tearing (arrow) noticed in a second review of the scan.
No endorsement of any kind received to conduct this study/article.
Conflict of interestThe authors declare no conflict of interest.
Ethical disclosureProtection of people and animals. The authors declare that this research has not been conducted experiments on humans or animals. Confidentiality of data. The authors declare that they have followed the protocols of the workplace on the publication of patient data. Right to privacy and informed consent. The authors have obtained the informed consent of patients and/or subjects referred to in article consent. This document is in the possession of the corresponding author.