The Williams–Beuren syndrome is a rare genetic disease characterized by: (a) typical facial features; (b) psychomotor retardation with a specific neurocognitive profile; (c) cardiovascular condition and (d) likely transient hypocalcemia in infancy.
The objective of this study was to describe the clinic evolution and diagnosis of patient with this syndrome that was associated with endocarditis caused by Streptococcus parasanguis in the ascending aorta and an aneurism located in the fronto-temporal area, which produced a parenchymal hematoma in the left lobe, and subarachnoid hemorrhage.
He was treated with ceftriaxone and dicloxacillin. Then we proceeded to correct the aneurysm and perform vegetation resection in aortic arteries with supravalvular aortic stenosis correction.
The evolution after one year has been favorable and is currently without neurologic sequelae.
A 5-year-old male patient presented a diagnosis of supravalvular aortic stenosis. After cardiac catheterization was performed, he presented a fever and right side paresis.
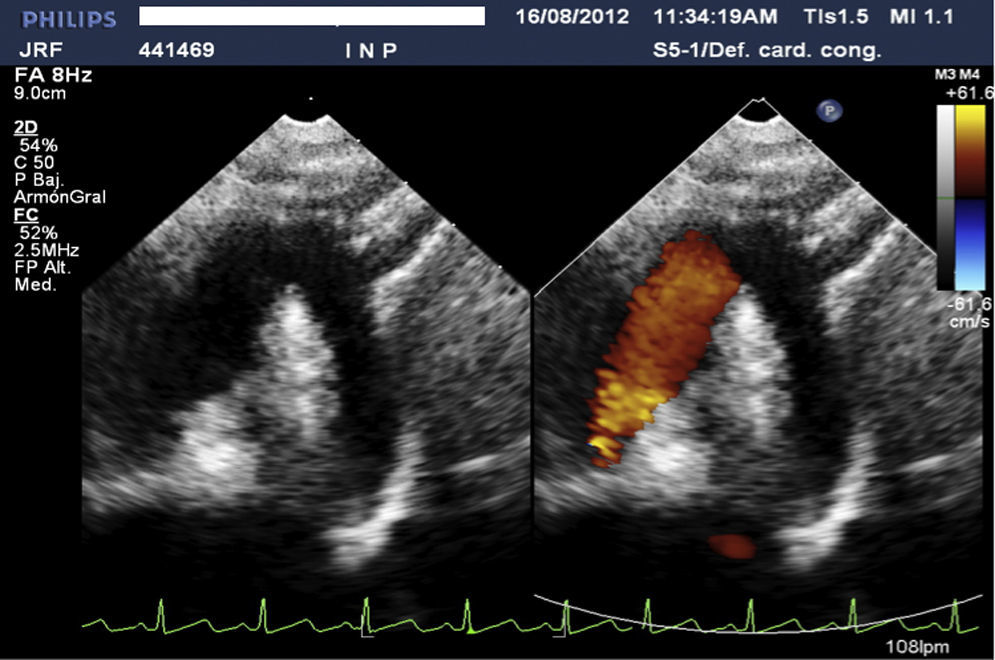
The echocardiogram showed multiple vegetations in the ascendant aortic arch and the supraortic arteries.
The blood cultures reported S. parasanguis.
The magnetic resonance showed a subarachnoid hemorrhage with an aneurysm and a hematoma.
El síndrome de Williams–Beuren es una enfermedad genética rara que se caracteriza por: a) rasgos faciales típicos; b) retraso del desarrollo psicomotor con un perfil neurocognitivo determinado; c) afección cardiovascular y d) probable hipocalcemia transitoria en la infancia.
El propósito de este estudio es dar a conocer un caso con este síndrome que se asoció a endocarditis infecciosa por Streptoccocus parasanguis de la aorta ascendente y aneurisma localizado en el área frontotemporal que produjo hematoma parenquimatoso del lóbulo izquierdo y hemorragia subaracnoidea.
El tratamiento que se ofreció fue antibioticoterapia con dicloxacilina y ceftriaxona, corrección de las lesiones cerebrales en dos 2 y reparación de la aorta ascendente con resección de las vegetaciones, en una tercera cirugía.
La evolución a un año ha sido favorable y actualmente se encuentra sin secuelas neurológicas.
Paciente masculino de 5 años de edad con diagnóstico de estenosis supravalvular aórtica. Tras un cateterismo cardiaco, presentó fiebre y hemiparesia derecha.
El ecocardiograma mostró múltiples vegetaciones en la aorta ascendente, arco aórtico y arterias supraaórticas.
Los cultivo sanguíneos reportaron Streptococcus parasanguis.
La resonancia magnética cerebral mostró hemorragia subaracnoidea con aneurismas y hematoma.
El tratamiento fue a base de ceftriaxona y dicloxacilina. Se procedió a corregir el aneurisma cerebral y la resección de las vegetaciones en arterias aórticas con corrección de la estenosis supravalvular aórtica.
WBS is a congenital disorder that affects the vascular connective tissue. It presents in 1 in 8000–10,000 live births.1,2 It is a multisystem developmental disorder caused by a microdeletion of 7q11.23 at chromosome 7.
The diagnosis of WBS is first done by clinical characteristics. The diagnosis is confirmed by fluorescence in situ hybridization (FISH). Cardiovascular abnormalities in these patients (80%) are confirmed using echocardiography; however, to complement the study it requires an angiography, MRI and/or cardiac catheterization and, in patients with pulmonary artery stenosis, pulmonary gammagram to assess perfusion.
The supravalvular aortic stenosis (SAS) is the most frequent finding (56%). 1,3–6 WS patients with cardiac lesions are at risk for infective endocarditis, but uncommon in supravalvular aortic stenosis site.
Case presentationFive-year-old male patient with WBS. Fluorescence in situ hybridization (FISH) confirmed deletion of 7q11.23 in chromosome 7, and the patient was sent to us for a complete cardiac evaluation.
The patient had “elfin facies”, and murmur in the aortic focus grade III and in his neck arteries.
The initial echocardiogram reveled supravalvular aortic stenosis (with gradient of 71mmHg).
The cardiac catheterization demonstrated right branch pulmonary artery stenosis (with a gradient of 11mmHg), brachiocephalic artery stenosis, and right renal absence.
Fifteen days after the patient's cardiac catheterization, he presented a high fever and right side right hemiparesis.
We performed a trans-thoracic echocardiogram, which revealed numerous mobile vegetations localized at the ascendant aortic arch and the supra-aortic arteries (Fig. 1). Blood cultures were positive for Streptococcus parasanguis. Antibiotic treatment was initiated with ceftriaxone for 52 days and dicloxacillin for 21 days.
A cerebral angio-resonance was performed which demonstrated a peripheral aneurysm rupture in the middle cerebral artery, with a left parenchymal hematoma and a subarchnoid hemorrhage.
The neurosurgeons performed two surgeries one month after his antibiotic therapy. In the first procedure they repaired the left fusiform aneurysm in the front temporal area. The second procedure was to repair the second right side aneurysm.
A third surgical procedure was performed on the patient in order to excise the vegetations. Repair of the ascending and aortic arch achieved with a bifurcated patch plasty (Doty repair) was used with untreated autologous pericardium.
Following the three surgical procedures the postoperative evolution of the patient was good (Fig. 2), and with no neurological complications after one year of follow up.
DiscussionThe follow jet across the SAS seemed to cause a predisposition to severe endocarditis.7 The SAS is not a predisposing factor for endocarditis progression, but this lesion can influence infective endocarditis, after endothelium lesion like hemodynamic study in children with WS and vegetation growth.
Spontaneous progression and regression of SAS and PABS were detected.
Patients with WBS have a higher risk of having a ruptured aneurysm or of having a recurrence of stenosis given the characteristics of the overgrowth of smooth muscle. Our patient presented a cerebral aneurysm and infective cerebral hematoma.
Only two last reports had infective endocarditis in SAS, one of them after percutaneous balloon valvuloplasty for aortic stenosis 7 years after and other one after dental work-up.7,8
Prevention is priority; this is why, it is our opinion that antibiotic prophylaxis should be given to patients with WBS, with cardiac lesion, prior to any invasive procedures which may cause bacteremia. Congenital abnormalities in those associated with high velocity jets can result in endothelial damage in aortic sinutubular leading to platelet and fibrin deposition and the formation of nonbacterial thrombotic endocardial lesions. In the presence of bacteremia, organisms may adhere to these lesions, leading to an infective vegetation.9 In our patient's case, we believe that the etiology may have been the cardiac catheterization performed 15 days prior to the presentations of the infective endocarditis.
In a review of 101 cases of children with supravalvular aortic stenosis, none had endocarditis after catheterization, so in our experience, this case is unusual.10
The antibiotic management of this patient was successful because 10 days after starting treatment, the fever subsided. This allowed us to perform the two surgeries in the brain and one in the arteries. The evolution in both cardiac and neurological procedures has been uneventful.
It is the first case of a child with WBS presenting endocarditis at a supravalvular aortic stenosis level and with the presence of cerebral aneurysms.
Data privacyThe authors declare that patient data does not appear in this article.
FundingNo endorsement of any kind received to conduct this study/article.
Conflict of interestThe authors declare no conflict of interest.