Introduction
Asthma is one of the main causes of morbidity in the paediatric patient, and its prevalence has been increasing considerably on a world scale over the last 20 years, particularly in paediatric populations.1 This illness requires constant care by the parents of the children affected. Due to its evolution it can involve many visits to the doctor and even continuous hospitalisation. However, this situation also causes serious changes in the daily life of the family, with significant repercussions on how a normal family functions.2 The influence of the family in the health-disease process is of vital importance, since it can function as a source of health or disease, or vice versa, and the patient may even compromise the health of the individuals who make up the family.3 The aim of our study was to compare how a family that includes a paediatric patient diagnosed with asthma functions, compared to families who do not have an asthmatic patient.
Methods
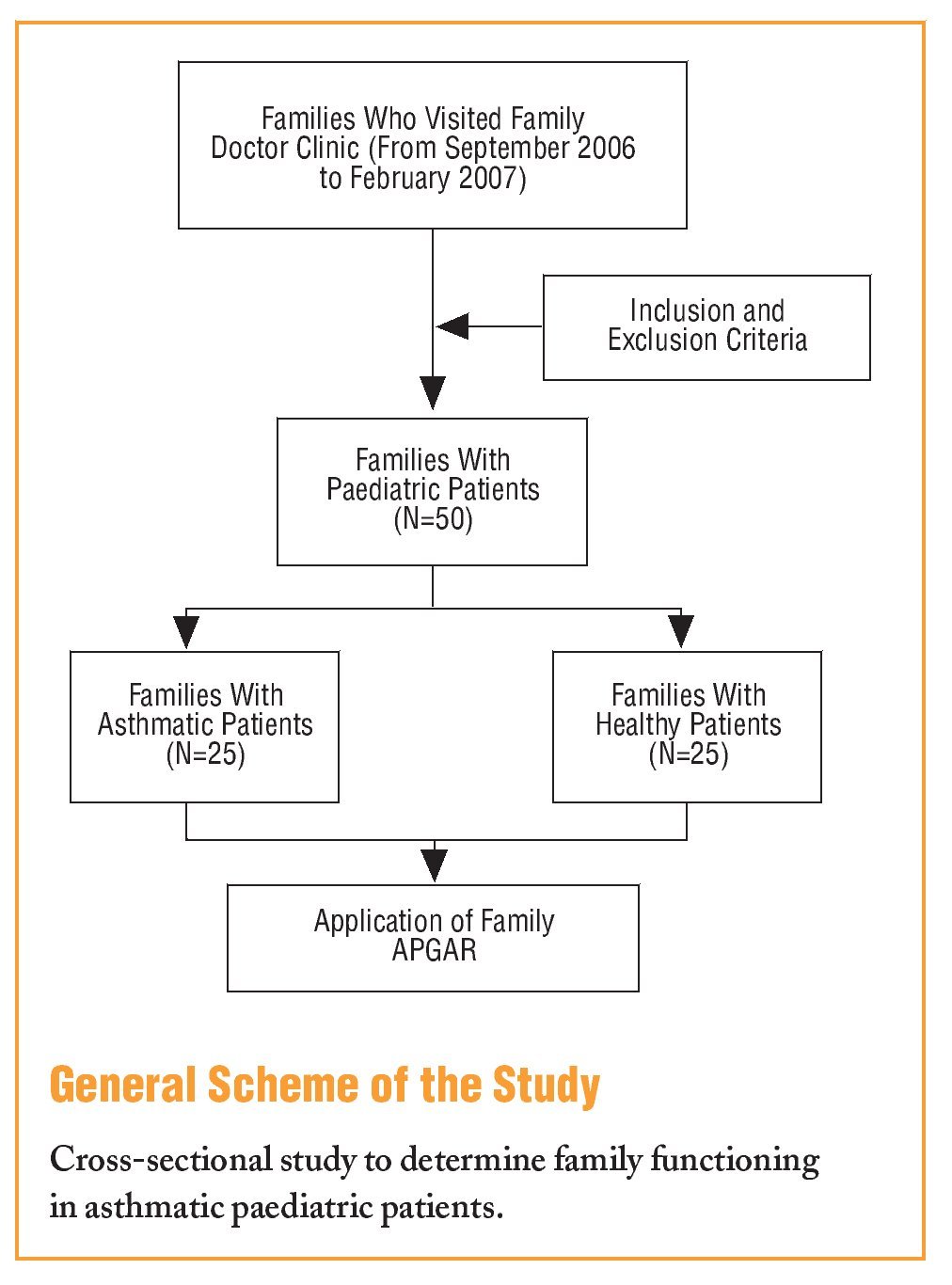
A cross-sectional study was carried out from September 2006 to February 2007. The inclusion criteria were: formally constituted family attached to a primary care unit; children of both sexes between 6 and 12 years old; healthy or asthmatic children who visited for monitoring.
The exclusion criteria were: if there were members of the nuclear family with chronic diseases (diabetes mellitus, arterial hypertension) or with neoplastic diseases.
A total of 50 families were included. All gave written informed consent. There were 15 families with an asthmatic child and 25 other families with a healthy child.
The assessment of family functioning was performed by applying a specific and validated tool called Family APGAR,4-6 which is described on the basis of the following scores: 0 to 3, severe dysfunction; 4 to 6, moderate dysfunction; and 7 to 10, a functioning family. The assessment was also made dichotomously, by only considering the functioning and dysfunction of the family. In the latter case, the severe and moderate dysfunctions were grouped, it was applied to members of the family, among which was the mother and a brother/sister over 10 years.The final rating of the tool was determined from the average score of the 2 applications. The sociodemographic variables included were the age of the patient and the mother, marital state and the composition of the family. To evaluate the latter, it was determined whether a family was nuclear or not.
The sample size was calculated by the EpiInfo statistics package, using the stat calc application, taking into account the following values: an alpha of 95%, power of 80%, and a prevalence of the factor studied (family dysfunction) in the healthy group of 4%, and 40% in the asthmatics group, giving a sample size of 25 families per group. The differences between the variables were determined using the c2 test. The mean differences in age were calculated using the Student t test for independent samples, and to calculate associations, the odds ratio (OR) was used with a 95% confidence interval (CI).
Statistical significance was considered as a value of P<.05, and the data were processed using the SPSS statistics package, version 10.
Results
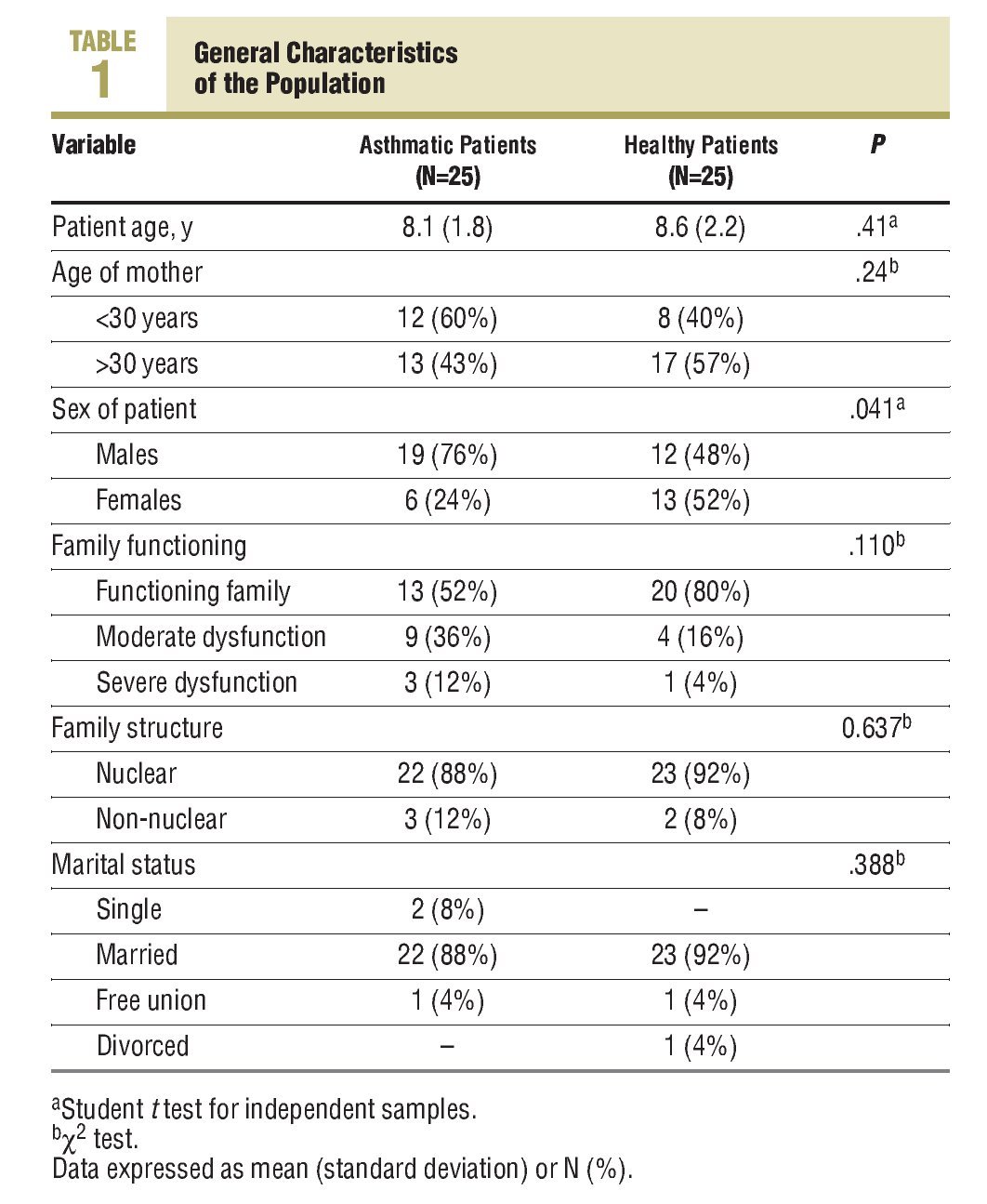
As regards the sex of the patients, the majority were males, with 62% in both family groups. The majority of patients (90%) belonged to nuclear families, with no differences between both groups. The marital state of the mother was also similar (Table 1).
The assessment of family functioning identified family dysfunction in a total 34% of the families.
On assessing the degree of functioning, moderate dysfunction was observed in 36% of families with asthmatic children compared to 16% for those did not, with a similar distribution in the case of severe dysfunction (12% compared to 4%; P=.11) (Table 1).
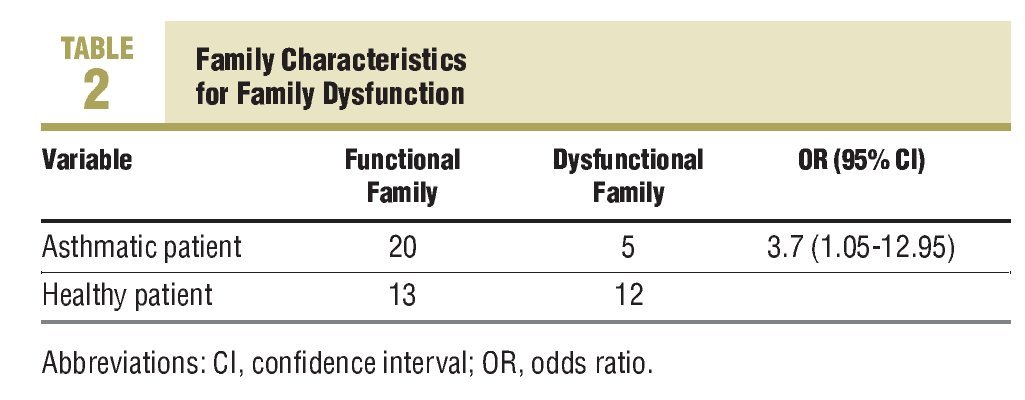
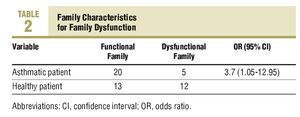
On determining the relationship with asthma, family dysfunction was more often observed in families with asthmatic children (48%) compared to families who did not (20%) (OR, 3.69; 95% CI, 1.05-12.95) (Table 2).
Discussion
Family dysfunction is a condition associated with families with paediatric asthmatic patients. Similarly, severe family dysfunction is present in a higher proportion of these families.
In our study a specific and validated tool was used to evaluate family functioning,4-6 which helped to identify differences between families of healthy children and families with asthmatic children.
Two studies, performed in paediatric populations with asthma, demonstrated that caring for paediatric patients with asthma can lead to an emotional burn-out in the parents and families.7,8
In a study carried out on a paediatric population on the quality of life of parents with asthmatic children, it was shown that many parents are unaware of the scope of the disease and can feel frustrated and even have depressive symptoms. Likewise, some parents indicate that daily family life is dependent on the level of control of the asthma in the child.9
According to our data, there are no previous studies that have evaluated family functioning in families with asthmatic paediatric patients using a specific tool. There are studies performed on adult populations with chronic lung diseases where there is evidence of a 20% prevalence of family dysfunction.10 However, when the patient is of paediatric age there is a higher level of concern for the parents, which modifies their parental roles and functions, a situation that can radically alter family interrelationships,11 since it not only has an impact on the patients.
Another factor related to family dysfunction is the inexperience of the family in the process of adapting to their new roles. The combination of this factor together with the recent diagnosis of asthma could have even more influence on changes in the family dynamics. Although we did not evaluate the level of knowledge the mothers had on asthma, or the time it took for the disease to progress, we consider that the age of the mother could indeed have an influence on the family dysfunction, since 40% of the mothers were less than 30 years old.
In a systematic review12 carried out on patients with different chronic diseases, including asthma in a paediatric population, it was shown that were no differences between both groups. However, we believe that this similarity could be due to not using a specific tool.
We can conclude that family dysfunction is present more often in families with asthmatic children. Another study showed that the symptoms of the asthmatic child can be reduced and his/her quality life improved by introducing changes in the family dynamics.13 Along this same line, it showed that the negative collateral effects of asthma on the parents can increase the asthma symptoms of the ill child.9 For this reason, we believe that the evaluation of the family dynamics should be considered a fundamental part of the integral approach to the paediatric patient with asthma. Although family dysfunction was an event associated with families with asthmatic children, with this type of study it is not possible to establish the causality between the variables, therefore we believe that studies have to be performed which will enable us to objectively establish the causality between these two events.
What Is Known About the Subject
•The influence of the family on the health-disease process is of vital importance, since the family can function as a source of health or disease.
•There is a relationship between different chronic diseases and family dysfunction; however, the differences are higher in relationship with asthma in children.
What This Study Contributes
•Asthma in a paediatric patient is associated with family dysfunction, therefore this parameter needs to be investigated in families as part of the integral approach.
Spanish version available www.elsevier.es/233.600
A commentary follow this article (page 546)
This study was wholly financed by the principal authors, with no conflicts of interest.
The present work was presented as a poster in the presentation of Biomedical Research Works in the XII National Congress of Family Medicine, held in Jalisco, México.
Correspondence:
J.E. Guzmán-Pantoja,
Batalla de Trinidad N.o 3068, Fraccionamiento Residencial Revolución,
45580 Tlaquepaque,
Jalisco, México
E-mail: familymedicinedoctors@gmail.com; dreduardoguzman@yahoo.com
Manuscript received November 30, 2007.
Manuscript accepted for publication May 22, 2008.