To analyze the perception of nursing professionals of the Madrid Primary Health Care environment in which they practice, as well as its relationship with socio-demographic, work-related and professional factors.
DesignCross-sectional, analytical, observational study.
Participants and contextQuestionnaire sent to a total of 475 nurses in Primary Health Care in Madrid (former Health Care Areas 6 and 9), in 2010.
Main measurementsPerception of the practice environment using the Practice Environment Scale of the Nursing Work Index (PES-NWI) questionnaire, as well as; age; sex; years of professional experience; professional category; Health Care Area; employment status and education level.
ResultsThere was a response rate of 69.7% (331). The raw score for the PES-NWI was: 81.04 [95%CI: 79.18–82.91]. The factor with the highest score was “Support from Managers” (2.9 [95%CI: 2.8–3]) and the lowest “Workforce adequacy” (2.3 [95%CI: 2.2–2.4]). In the regression model (dependent variable: raw score in PES-NWI), adjusted by age, sex, employment status, professional category (coefficient B=6.586), and years worked at the centre (coefficient B=2.139, for a time of 0–2 years; coefficient B=7.482, for 3–10 years; coefficient B=7.867, for over 20 years) remained at p≤0.05.
ConclusionsThe support provided by nurse managers is the most highly valued factor in this practice environment, while workforce adequacy is perceived as the lowest. Nurses in posts of responsibility and those possessing a higher degree of training perceive their practice environment more favourably. Knowledge of the factors in the practice environment is a key element for health care organizations to optimize provision of care and to improve health care results.
Analizar la percepción de los profesionales enfermeros de atención primaria de Madrid sobre el entorno en el que realizan su práctica, también relacionada con los factores sociodemográficos, laborales y profesionales.
DiseñoEstudio observacional analítico transversal.
Participantes y contexto475 enfermeros de Atención Primaria de Madrid (áreas 6 y 9, en 2010).
Mediciones principalesPercepción del entorno de la práctica, a través del cuestionario Practice Environment Scale of the Nursing Work Index (PES-NWI); edad; sexo; años de experiencia profesional; categoría; área de salud; contratación y nivel académico.
ResultadosSe estudiaron 331 sujetos (tasa de respuesta: 69,7%). La puntuación bruta para el PES-NWI fue: 81,04 [IC 95%: 79,18-82,91]. El factor mejor valorado fue «Apoyo de los gestores» (2,9 [IC 95%: 2,8-3]) y el peor, «Adecuación de la plantilla» (2,3 [IC 95%: 2,2-2,4]). En el modelo de regresión (variable dependiente: puntuación bruta del PES-NWI), ajustado por edad, sexo, situación laboral, permanecieron con una p ≤ 0,05, la categoría profesional (coeficiente B = 6,586) y los años de ejercicio profesional en el centro (coeficiente B = 2,139, para tiempo de 0 a 2 años; coeficiente B = 7,482, para tiempo de 3-10 años; coeficiente B = 7,867, para tiempo de más de 20 años).
ConclusionesLas enfermeras con cargo de responsabilidad y aquellas que tienen mayor formación tienen una mejor percepción de su entorno de práctica. Conocer los factores del entorno de la práctica es un elemento clave para la organización sanitaria con el fin de optimizar la provisión de cuidados, y mejorar los resultados en salud.
- •
It has been shown that an association exists between nursing practice environment factors and the stability of the nursing staff workforce, job satisfaction, quality of care and results in patients.
- •
Five key aspects have been identified regarding a healthy nursing practice environment: nurses’ participation; foundation of quality of nursing care; managers’ support; appropriate workforce and resources; and efficient relations between medical and nursing staff.
- •
The practice environment has been studied amply in the hospital environment but less in Primary Health Care.
- •
The perception of the environment practice nurses in primary care is better nursing managers, nurses with temporary contracts, which have a longer practice in the centre between 3 and 10 years, and those with graduate degrees in nursing.
- •
The environment factor with the poorest perception is Workforce Adequacy.
- •
We must develop leadership styles that optimize the performance of the workforce, and thus increase the efficiency of the health system.
Over the last decades it has been shown that an association exists between nursing practice environment factors and the stability of the nursing staff workforce, job satisfaction (absenteeism rates and perceived productivity), quality of care and results in patients (mortality, average length of stay, patient satisfaction).1 Kazanjian et al.2 reached the same conclusions after a systematic review which revealed that one or more unfavourable attributes in the nursing practice environment were associated with higher mortality rates. Moreover, the report of the USA Institute of Medicine, Keeping Patients Safe: Transforming the Work Environment of Nurses3 showed that 98,000 patients died each year due to errors, many of which were related to an unhealthy working environment characterized either by poor communication among health care staff, or resistance to changes and lack of leadership. On these same lines, the studies by Manojlovich et al.,4,5 also warned against the negative consequences (errors involving administering drugs) for patients of poor communication between medical and nursing professionals.
Laschinger's6 conclusions, after developing Kanter's7Theory of Empowerment, maintain that many labour attitudes and responses are more closely related to the working environment within organizations and have less to do with individual traits of the professionals who work there. In an empowered working environment, employees have access to information, resources and opportunities to improve their knowledge and skills. This translates into greater productivity for the organization, greater implication from staff8 and, with regard to results in patients, it has been demonstrated the association between empowerment and patient safety.9
From research carried out by the American Academy of Nurses on magnet hospitals, based on original studies by Kramer et al.,10 stemmed the concept “practice environment” or “working environment”, which Lake defined as the organizational features that enable or hinder professional nursing practice.11 Lake identified five key aspects relative to the nursing practice environment, that must occur in a healthy working environment as appropriate at Magnet hospitals: nurses’ participation in the organization; foundation of quality of nursing care; managers’ support to nurses; adequate workforce and resources; efficient medical/nursing staff relations. Contextual factors are also key elements to carry out an evidence based practice (EBP).12–14
Several tools have been developed to measure the nursing practice environment; among the most widely used is the Practice Environment Scale of the Nursing Work Index (PES-NWI) designed by Lake (2002).11 The PES-NWI was developed from the Nursing Work Index (NWI) drawn up by Kramer and Hafner,15 which contained 65 items and was successively revised. Noteworthy among subsequent revisions is that performed by Aiken & Patrician (2002),16 which gave rise to the NWI-Revised with 46 items. Other recent publications, however, back up the PES-NWI as an instrument of greater methodological grounding.17,18 In Spain, de Pedro-Gómez et al. have carried out studies19,20 on transcultural adaptation and validation of the PES-NWI for use in Primary Health and Hospital Care with satisfactory results.
On the grounds expressed above, this study aimed to analyze the perception of Madrid Primary Health Care Nursing Professionals of their practice environment, and to characterize this perception as a function of socio-demographic, labour and professional factors.
MethodDesignA transversal, analytical, observational study was performed on the nurse population at Primary Health Care in the Community of Madrid during the period from June to October 2010.
Population and sampleThe estimated sample requirement was 475 nurses for a standard deviation of 15.24,21 with a precision rate of 1.2, reliability of 95% and an estimated population of 3600 nurses in the Community of Madrid. The sample was taken in the former Health Care Areas 9 and 6. All professional nursing staff at all centres pertaining to Primary Health Care Area number 9 and 6 were selected (currently known as South-West Health Care Authority, n=190 and North-West Health Care Authority, n=285). The exclusion criterion applied was the premise that seniority in the post should not be less than 6 months in the current position.
Study instruments and variablesThe data collection instrument used was the Practice Environment Scale of the Nursing Work Index (PES-NWI), adapted to the Spanish context, validated by de Pedro-Gómez (showing Cronbach's alpha coefficient for global reliability of 0.906)19 and re-validated in Primary Care (with Cronbach's alpha of 0.913).20
The questionnaire comprises 31 items (each item measures on a Likert type, four-point scale, the lowest score corresponds to the minimum agreement and the highest to maximum agreement). All 31 items are grouped under five factors: (I) “Participation of nurses in issues affecting the health centre” (Participation); (II) “Foundation of quality of nursing care” (Foundation Care); (III) “Nurse Managers’ Capacity, Leadership and Support to Nursing Staff” (Managers Support); (IV) “Workforce Dimensions and Adequacy of Human Resources” (Workforce Adequacy); (V) “Relations between medical and nursing staff” (Physician/Nurse relations). The following variables were also studied: age; sex; years of professional experience (in general and at the current centre); professional category (clinical nurse, nurse manager); Health Care Area (6 or 9); employment status (indefinite duration contract, definite duration contract); and education level (University Graduate Degree in Nursing, Bachelor's/Master's (BSc/MSc) degree in Nursing, other further or post-graduate studies in other disciplines).
All people in the sample received a personalized questionnaire with a cover letter containing a confidentiality clause to guarantee data protection measures, in compliance with Organic Law 15/1999 on the Protection of Personal Data. An envelope was provided for returning the completed questionnaire to the research team. The study was approved by the Clinical Research Ethics Board of the University Hospital Puerta de Hierro, Majadahonda (Madrid).
Data processing and analysisDescriptive statistical indices were calculated. Regarding the PES-NWI, the summary scores were calculated for each factor and global, and likewise for mean value, according to the number of items for each factor. For the bivariate analysis, where values on the PES-NWI were considered as dependent variables and the rest of variables as independent, Student's t-tests, ANOVA and Pearson Chi-squared test correlation coefficient were used as statistical hypothesis tests. Finally, multivariate analysis was performed through multiple linear regression, in which the raw scores on the PES-NWI were treated as dependent variables and those obtaining statistical significance ≤0.20 at bivariate level were considered as explicative/predictive variables. 95% Confidence intervals were calculated (95%CI). All analyses were conducted with a significance level of ≤0.05. Work was carried out using the software package SPSS v. 17.
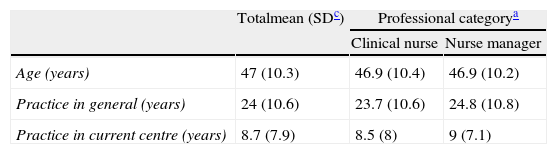
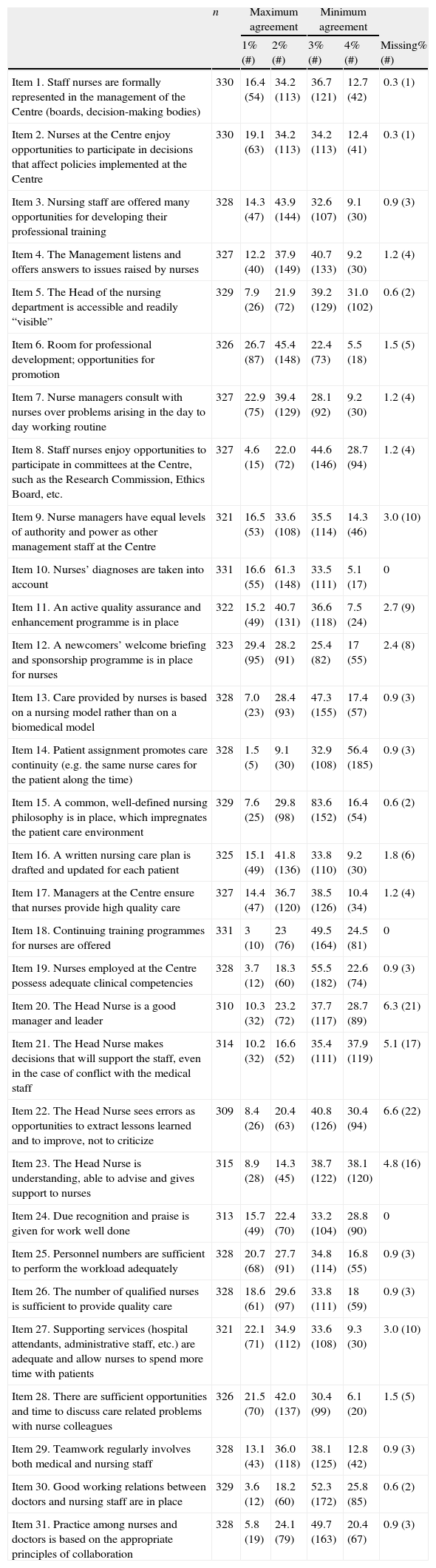
Results331 subjects were studied (response rate 69.7%). The characteristics of the participants are shown in Table 1. Regarding scores for the items in the PES-NWI, the highest percentage (56.4%) under “maximum agreement” went to item 14: “Patient assignment promotes care continuity (e.g. the same nurse cares for the patient along the time)”, pertaining to the factor Foundation Care. The item with the highest percentage (29.4%) under “minimum agreement” fell to item 12: “A newcomers’ welcome briefing and sponsorship programme is in place for nurses”, pertaining to the factor Foundation Care (Table 2).
Characteristics of the sample.
| Totalmean (SDc) | Professional categorya | ||
| Clinical nurse | Nurse manager | ||
| Age (years) | 47 (10.3) | 46.9 (10.4) | 46.9 (10.2) |
| Practice in general (years) | 24 (10.6) | 23.7 (10.6) | 24.8 (10.8) |
| Practice in current centre (years) | 8.7 (7.9) | 8.5 (8) | 9 (7.1) |
| Total% (#) | Professional categorya | ||
| Clinical nurse% (#) | Nurse manager% (#) | ||
| Sex | |||
| Women | 83.4 (262) | 84.1 (232) | 78.9 (30) |
| Men | 16.6 (52) | 15.9 (44) | 15.4 (8) |
| Total | 100 (314) | 100 (278) | 100 (38) |
| Professional category | |||
| Clinical nurse | 87.9 (277) | ||
| Nurse manager | 12.1 (38) | ||
| Total | 100 (315) | ||
| Employment status | |||
| Indefinite duration contract | 74.6 (226) | 74.8 (199) | 73 (27) |
| Definite duration contract | 25.4 (77) | 25.2 (67) | 27 (10) |
| Total | 100 (303) | 100 (266) | 100 (37) |
| Academic level | |||
| University graduate degree in nursing | 84.1 (260) | 83.4 (226) | 89.5 (34) |
| Bachelor's and/or master's degree in nursing | 4.9 (15) | 5.5 (15) | 0 |
| Other qualificationsb | 11 (34) | 11.1 (30) | 10.5 (4) |
| Total | 100 (309) | 100 (281) | 100 (38) |
| Health's Area | |||
| 6 | 53.8 (178) | 53.1 (147) | 50 (19) |
| 9 | 46.2 (153) | 46.9 (130) | 50 (19) |
| Total | 100 (331) | 100 (277) | 100 (38) |
| Years of experience | |||
| <3 years | 0 | 0 | 0 |
| 3–10 years | 14.3 (44) | 14.8 (40) | 10.8 (4) |
| 11–20 years | 23.7 (73) | 22.5 (61) | 32.4 (12) |
| >20 years | 62 (191) | 62.7 (170) | 56.8 (21) |
| Total | 100 (308) | 100 (271) | 100 (37) |
| Years of experience in current centre | |||
| <3 years | 11.7 (36) | 12.3 (33) | 7.9 (3) |
| 3–10 years | 55.4 (170) | 55.4 (149) | 55.3 (21) |
| 11–20 years | 24.4 (75) | 23.8 (64) | 28.9 (11) |
| >20 years | 8.5 (26) | 8.6 (23) | 7.9 (3) |
| Total | 100 (307) | 100 (269) | 100 (38) |
Assessment of the PES-NWI (Practice Environment Scale of the Nursing Work Index) items.
| n | Maximum agreement | Minimum agreement | ||||
| 1% (#) | 2% (#) | 3% (#) | 4% (#) | Missing% (#) | ||
| Item 1. Staff nurses are formally represented in the management of the Centre (boards, decision-making bodies) | 330 | 16.4 (54) | 34.2 (113) | 36.7 (121) | 12.7 (42) | 0.3 (1) |
| Item 2. Nurses at the Centre enjoy opportunities to participate in decisions that affect policies implemented at the Centre | 330 | 19.1 (63) | 34.2 (113) | 34.2 (113) | 12.4 (41) | 0.3 (1) |
| Item 3. Nursing staff are offered many opportunities for developing their professional training | 328 | 14.3 (47) | 43.9 (144) | 32.6 (107) | 9.1 (30) | 0.9 (3) |
| Item 4. The Management listens and offers answers to issues raised by nurses | 327 | 12.2 (40) | 37.9 (149) | 40.7 (133) | 9.2 (30) | 1.2 (4) |
| Item 5. The Head of the nursing department is accessible and readily “visible” | 329 | 7.9 (26) | 21.9 (72) | 39.2 (129) | 31.0 (102) | 0.6 (2) |
| Item 6. Room for professional development; opportunities for promotion | 326 | 26.7 (87) | 45.4 (148) | 22.4 (73) | 5.5 (18) | 1.5 (5) |
| Item 7. Nurse managers consult with nurses over problems arising in the day to day working routine | 327 | 22.9 (75) | 39.4 (129) | 28.1 (92) | 9.2 (30) | 1.2 (4) |
| Item 8. Staff nurses enjoy opportunities to participate in committees at the Centre, such as the Research Commission, Ethics Board, etc. | 327 | 4.6 (15) | 22.0 (72) | 44.6 (146) | 28.7 (94) | 1.2 (4) |
| Item 9. Nurse managers have equal levels of authority and power as other management staff at the Centre | 321 | 16.5 (53) | 33.6 (108) | 35.5 (114) | 14.3 (46) | 3.0 (10) |
| Item 10. Nurses’ diagnoses are taken into account | 331 | 16.6 (55) | 61.3 (148) | 33.5 (111) | 5.1 (17) | 0 |
| Item 11. An active quality assurance and enhancement programme is in place | 322 | 15.2 (49) | 40.7 (131) | 36.6 (118) | 7.5 (24) | 2.7 (9) |
| Item 12. A newcomers’ welcome briefing and sponsorship programme is in place for nurses | 323 | 29.4 (95) | 28.2 (91) | 25.4 (82) | 17 (55) | 2.4 (8) |
| Item 13. Care provided by nurses is based on a nursing model rather than on a biomedical model | 328 | 7.0 (23) | 28.4 (93) | 47.3 (155) | 17.4 (57) | 0.9 (3) |
| Item 14. Patient assignment promotes care continuity (e.g. the same nurse cares for the patient along the time) | 328 | 1.5 (5) | 9.1 (30) | 32.9 (108) | 56.4 (185) | 0.9 (3) |
| Item 15. A common, well-defined nursing philosophy is in place, which impregnates the patient care environment | 329 | 7.6 (25) | 29.8 (98) | 83.6 (152) | 16.4 (54) | 0.6 (2) |
| Item 16. A written nursing care plan is drafted and updated for each patient | 325 | 15.1 (49) | 41.8 (136) | 33.8 (110) | 9.2 (30) | 1.8 (6) |
| Item 17. Managers at the Centre ensure that nurses provide high quality care | 327 | 14.4 (47) | 36.7 (120) | 38.5 (126) | 10.4 (34) | 1.2 (4) |
| Item 18. Continuing training programmes for nurses are offered | 331 | 3 (10) | 23 (76) | 49.5 (164) | 24.5 (81) | 0 |
| Item 19. Nurses employed at the Centre possess adequate clinical competencies | 328 | 3.7 (12) | 18.3 (60) | 55.5 (182) | 22.6 (74) | 0.9 (3) |
| Item 20. The Head Nurse is a good manager and leader | 310 | 10.3 (32) | 23.2 (72) | 37.7 (117) | 28.7 (89) | 6.3 (21) |
| Item 21. The Head Nurse makes decisions that will support the staff, even in the case of conflict with the medical staff | 314 | 10.2 (32) | 16.6 (52) | 35.4 (111) | 37.9 (119) | 5.1 (17) |
| Item 22. The Head Nurse sees errors as opportunities to extract lessons learned and to improve, not to criticize | 309 | 8.4 (26) | 20.4 (63) | 40.8 (126) | 30.4 (94) | 6.6 (22) |
| Item 23. The Head Nurse is understanding, able to advise and gives support to nurses | 315 | 8.9 (28) | 14.3 (45) | 38.7 (122) | 38.1 (120) | 4.8 (16) |
| Item 24. Due recognition and praise is given for work well done | 313 | 15.7 (49) | 22.4 (70) | 33.2 (104) | 28.8 (90) | 0 |
| Item 25. Personnel numbers are sufficient to perform the workload adequately | 328 | 20.7 (68) | 27.7 (91) | 34.8 (114) | 16.8 (55) | 0.9 (3) |
| Item 26. The number of qualified nurses is sufficient to provide quality care | 328 | 18.6 (61) | 29.6 (97) | 33.8 (111) | 18 (59) | 0.9 (3) |
| Item 27. Supporting services (hospital attendants, administrative staff, etc.) are adequate and allow nurses to spend more time with patients | 321 | 22.1 (71) | 34.9 (112) | 33.6 (108) | 9.3 (30) | 3.0 (10) |
| Item 28. There are sufficient opportunities and time to discuss care related problems with nurse colleagues | 326 | 21.5 (70) | 42.0 (137) | 30.4 (99) | 6.1 (20) | 1.5 (5) |
| Item 29. Teamwork regularly involves both medical and nursing staff | 328 | 13.1 (43) | 36.0 (118) | 38.1 (125) | 12.8 (42) | 0.9 (3) |
| Item 30. Good working relations between doctors and nursing staff are in place | 329 | 3.6 (12) | 18.2 (60) | 52.3 (172) | 25.8 (85) | 0.6 (2) |
| Item 31. Practice among nurses and doctors is based on the appropriate principles of collaboration | 328 | 5.8 (19) | 24.1 (79) | 49.7 (163) | 20.4 (67) | 0.9 (3) |
Mean values for each factor were as follows: 2.49 [95%IC: 2.42–2.56] for the factor Participation; 2.64 [95%IC: 2.58–2.7] for Foundation Care; 2.9 [95%IC: 2.8–3] for Managers Support; 2.3 [95%IC: 2.21–2.4] for Workforce Adequacy; and 2.7 [95%IC: 2.68–2.86] for Physician/Nurse Relations.
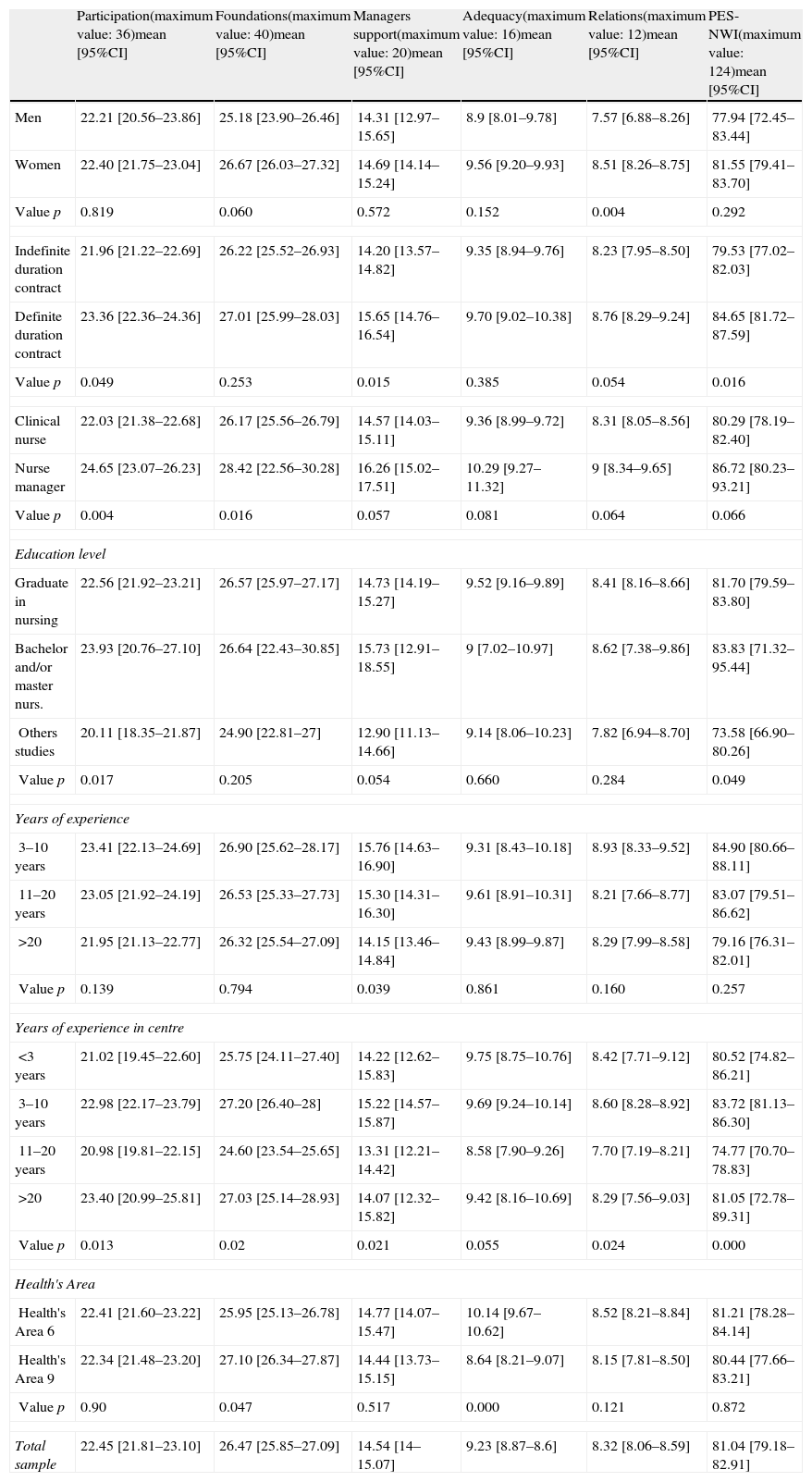
As for summary scores, women gave higher scores than men to the factor Physician/Nurse Relations (women: 8.5; men: 7.5; p=0.004). On employment status, nurses on definite duration contracts gave higher scores than those on indefinite duration contracts to the factor Participation (definite contracts: 23.3; indefinite contracts: 21.9; p=0.049); to the factor Managers Support (definite contracts: 15.6; indefinite contracts: 14.2; p=0.015); and to the factor Physician/Nurse Relations (definite contracts: 8.7; indefinite contracts: 8.2; p=0.054). Depending on their professional category, nurses in posts of responsibility gave higher scores than clinical nursing staff to the factor Participation (nurse manager: 24.6; clinical nurse: 22; p=0.004); to factor Foundation Care (nurse manager: 28.4; clinical nurse: 26.1; p=0.016); and to the factor Managers Support (nurse manager: 16.2; clinical nurse: 14.5; p=0.057).
Regarding the academic level, nurses possessing advanced studies in nursing scored higher in the factor Participation than nurses with other qualifications (BSc/MSc in Nursing: 23.9; University Graduate degree in Nursing: 22.5; other qualifications: 20.1; p=0.017); in the factor Managers Support (BSc/MSc in Nursing: 15.7; University Graduate degree in Nursing: 14.7; other qualifications: 12.9; p=0.054).
Regarding the number of years dedicated to professional activity, professionals with 3–10 years’ experience scored higher than other groups in the factor Management Support (experience of 3–10 years: 15.7; 11–20 years: 15.3; more than 20 years: 14.1; p=0.039). Taking into account time employed at current workplace, professionals with 3–10 years’ experience scored higher than other groups in factors Foundation Care (experience of 3–10 years: 27.2; 0–2 years: 25.7; 11–20 years: 24.6; more than 20 years: 27; p=0.02); Managers Support (experience of 3–10 years: 15.2; 0–2 years: 14.2; 11–20 years: 13.3; more than 20 years: 14; p=0.021); and Physician/Nurse Relations (experience of 3–10 years: 8.6; 0–2 years: 8.4; 11–20 years: 7.7; more than 20 years: 8.2; p=0.024). However, for the factor Participation professionals with more than 20 years scored the highest: (professionals with more than 20 years: 23.4; 0–2 years: 21; 3–10 years: 22.9; 11–20 years: 20.9; p=0.013). With regard to the Health Care Area, nurses in Area number 6 scored higher than those in Area number 9 for factor Workforce Adequacy (Area 6: 10.1; Area 9: 8.6; p=0.000) (Table 3).
Summary scores of the factors and the global PES-NWI by sex, employment status, professional category, educational level, years of experience and area health.
| Participation(maximum value: 36)mean [95%CI] | Foundations(maximum value: 40)mean [95%CI] | Managers support(maximum value: 20)mean [95%CI] | Adequacy(maximum value: 16)mean [95%CI] | Relations(maximum value: 12)mean [95%CI] | PES-NWI(maximum value: 124)mean [95%CI] | |
| Men | 22.21 [20.56–23.86] | 25.18 [23.90–26.46] | 14.31 [12.97–15.65] | 8.9 [8.01–9.78] | 7.57 [6.88–8.26] | 77.94 [72.45–83.44] |
| Women | 22.40 [21.75–23.04] | 26.67 [26.03–27.32] | 14.69 [14.14–15.24] | 9.56 [9.20–9.93] | 8.51 [8.26–8.75] | 81.55 [79.41–83.70] |
| Value p | 0.819 | 0.060 | 0.572 | 0.152 | 0.004 | 0.292 |
| Indefinite duration contract | 21.96 [21.22–22.69] | 26.22 [25.52–26.93] | 14.20 [13.57–14.82] | 9.35 [8.94–9.76] | 8.23 [7.95–8.50] | 79.53 [77.02–82.03] |
| Definite duration contract | 23.36 [22.36–24.36] | 27.01 [25.99–28.03] | 15.65 [14.76–16.54] | 9.70 [9.02–10.38] | 8.76 [8.29–9.24] | 84.65 [81.72–87.59] |
| Value p | 0.049 | 0.253 | 0.015 | 0.385 | 0.054 | 0.016 |
| Clinical nurse | 22.03 [21.38–22.68] | 26.17 [25.56–26.79] | 14.57 [14.03–15.11] | 9.36 [8.99–9.72] | 8.31 [8.05–8.56] | 80.29 [78.19–82.40] |
| Nurse manager | 24.65 [23.07–26.23] | 28.42 [22.56–30.28] | 16.26 [15.02–17.51] | 10.29 [9.27–11.32] | 9 [8.34–9.65] | 86.72 [80.23–93.21] |
| Value p | 0.004 | 0.016 | 0.057 | 0.081 | 0.064 | 0.066 |
| Education level | ||||||
| Graduate in nursing | 22.56 [21.92–23.21] | 26.57 [25.97–27.17] | 14.73 [14.19–15.27] | 9.52 [9.16–9.89] | 8.41 [8.16–8.66] | 81.70 [79.59–83.80] |
| Bachelor and/or master nurs. | 23.93 [20.76–27.10] | 26.64 [22.43–30.85] | 15.73 [12.91–18.55] | 9 [7.02–10.97] | 8.62 [7.38–9.86] | 83.83 [71.32–95.44] |
| Others studies | 20.11 [18.35–21.87] | 24.90 [22.81–27] | 12.90 [11.13–14.66] | 9.14 [8.06–10.23] | 7.82 [6.94–8.70] | 73.58 [66.90–80.26] |
| Value p | 0.017 | 0.205 | 0.054 | 0.660 | 0.284 | 0.049 |
| Years of experience | ||||||
| 3–10 years | 23.41 [22.13–24.69] | 26.90 [25.62–28.17] | 15.76 [14.63–16.90] | 9.31 [8.43–10.18] | 8.93 [8.33–9.52] | 84.90 [80.66–88.11] |
| 11–20 years | 23.05 [21.92–24.19] | 26.53 [25.33–27.73] | 15.30 [14.31–16.30] | 9.61 [8.91–10.31] | 8.21 [7.66–8.77] | 83.07 [79.51–86.62] |
| >20 | 21.95 [21.13–22.77] | 26.32 [25.54–27.09] | 14.15 [13.46–14.84] | 9.43 [8.99–9.87] | 8.29 [7.99–8.58] | 79.16 [76.31–82.01] |
| Value p | 0.139 | 0.794 | 0.039 | 0.861 | 0.160 | 0.257 |
| Years of experience in centre | ||||||
| <3 years | 21.02 [19.45–22.60] | 25.75 [24.11–27.40] | 14.22 [12.62–15.83] | 9.75 [8.75–10.76] | 8.42 [7.71–9.12] | 80.52 [74.82–86.21] |
| 3–10 years | 22.98 [22.17–23.79] | 27.20 [26.40–28] | 15.22 [14.57–15.87] | 9.69 [9.24–10.14] | 8.60 [8.28–8.92] | 83.72 [81.13–86.30] |
| 11–20 years | 20.98 [19.81–22.15] | 24.60 [23.54–25.65] | 13.31 [12.21–14.42] | 8.58 [7.90–9.26] | 7.70 [7.19–8.21] | 74.77 [70.70–78.83] |
| >20 | 23.40 [20.99–25.81] | 27.03 [25.14–28.93] | 14.07 [12.32–15.82] | 9.42 [8.16–10.69] | 8.29 [7.56–9.03] | 81.05 [72.78–89.31] |
| Value p | 0.013 | 0.02 | 0.021 | 0.055 | 0.024 | 0.000 |
| Health's Area | ||||||
| Health's Area 6 | 22.41 [21.60–23.22] | 25.95 [25.13–26.78] | 14.77 [14.07–15.47] | 10.14 [9.67–10.62] | 8.52 [8.21–8.84] | 81.21 [78.28–84.14] |
| Health's Area 9 | 22.34 [21.48–23.20] | 27.10 [26.34–27.87] | 14.44 [13.73–15.15] | 8.64 [8.21–9.07] | 8.15 [7.81–8.50] | 80.44 [77.66–83.21] |
| Value p | 0.90 | 0.047 | 0.517 | 0.000 | 0.121 | 0.872 |
| Total sample | 22.45 [21.81–23.10] | 26.47 [25.85–27.09] | 14.54 [14–15.07] | 9.23 [8.87–8.6] | 8.32 [8.06–8.59] | 81.04 [79.18–82.91] |
Nursing staff age was found to correlate negatively with the factor Participation (r=−0.117; p=0.045), Managers Support (r=−0.161; p=0.06) and PES-NWI (r=0.132; p=0.038).
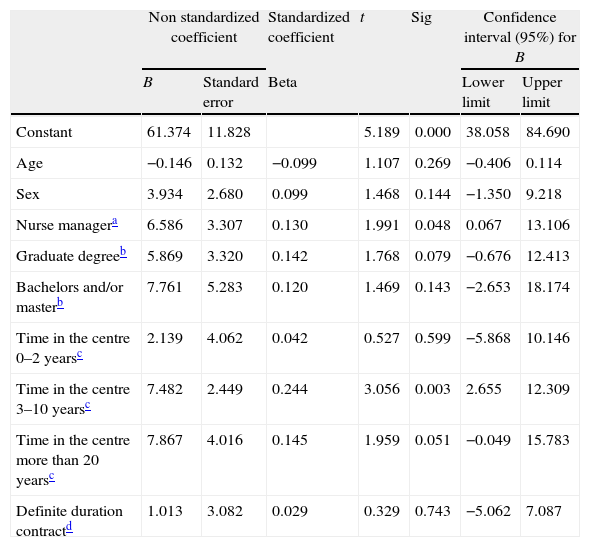
The categories that remained in the multiple linear regression model (dependent variable: crude score in PES-NWI), adjusted by age, gender and employment status, with p≤0.05, were professional category (coefficient B=6.586, for “nurse manager; category of reference: clinical nurse), the number of years worked at the centre (coefficient B=2.139, for time ranging from 0 to 2 years; coefficient B=7.482, for time ranging from 3 to 10 years; coefficient B=7.867, for more than 20 years; category of reference: 11–20 years); educational level obtained a p value of 0.079 (coefficient B=5.869, for Bachelor's degree and coefficient B=7.761, for Master's degree; category of reference: other university studies) (Table 4).
Multiple linear regression model for the PES-NWI.
| Non standardized coefficient | Standardized coefficient | t | Sig | Confidence interval (95%) for B | |||
| B | Standard error | Beta | Lower limit | Upper limit | |||
| Constant | 61.374 | 11.828 | 5.189 | 0.000 | 38.058 | 84.690 | |
| Age | −0.146 | 0.132 | −0.099 | 1.107 | 0.269 | −0.406 | 0.114 |
| Sex | 3.934 | 2.680 | 0.099 | 1.468 | 0.144 | −1.350 | 9.218 |
| Nurse managera | 6.586 | 3.307 | 0.130 | 1.991 | 0.048 | 0.067 | 13.106 |
| Graduate degreeb | 5.869 | 3.320 | 0.142 | 1.768 | 0.079 | −0.676 | 12.413 |
| Bachelors and/or masterb | 7.761 | 5.283 | 0.120 | 1.469 | 0.143 | −2.653 | 18.174 |
| Time in the centre 0–2 yearsc | 2.139 | 4.062 | 0.042 | 0.527 | 0.599 | −5.868 | 10.146 |
| Time in the centre 3–10 yearsc | 7.482 | 2.449 | 0.244 | 3.056 | 0.003 | 2.655 | 12.309 |
| Time in the centre more than 20 yearsc | 7.867 | 4.016 | 0.145 | 1.959 | 0.051 | −0.049 | 15.783 |
| Definite duration contractd | 1.013 | 3.082 | 0.029 | 0.329 | 0.743 | −5.062 | 7.087 |
Model's parameters: R: 0.346; R2: 0.12; F: 3.197; p=0.001; Durbin–Watson statistics: 2.08.
This study allows knowing how the nursing professionals of Spanish Primary Health Care perceive their practice environment, as well as the factors that contribute to a more positive perception.
Practice environment perception was better in nurse managers, nurses under definite duration contracts, nurses with professional experience at the centre of 3–10 years, and staff with advanced studies in nursing. Global score in the PES-NWI was 81.04, only slightly higher than the score registered for nursing professionals in Primary Health Care in the Balearics (80.4).14
The environmental factor valued most highly was Managers Support while the lowest valuation was for Workforce Adequacy. The poor perception is easily explained by the fact that the ratio of nurses in General Care per 1000 inhabitants in Spain is considerably lower than the average in OECD countries (in 2009, the most recent data available, 4.9 in Spain against 8.4 throughout the OECD22); to which we must add the high rate of ageing in our society,23 which leads not only to an increasing nursing demand but to a greater complexity in the provision of care. It must also be stressed that Madrid is one of the three Spanish autonomous communities with the lowest ratio of general care nurses in Primary Health Care (63.8 per 100,000 inhabitants) in Spain (83.9 per 100,000 inhabitants).24
Nurse managers expressed a positive perception for the factors Participation, Foundation Care and Managers Support, coinciding with the findings of the study conducted by de Pedro-Gómez.14 It seems likely that holding a post that requires leadership encourages deeper institutional commitment, which in turn helps generate a better working environment. Both Manojlovich25 and Verhaeghe26 have shown that managers play a vital role in creating favourable working environments, by strengthening the doctor/nurse relationship and reducing stress and other threatening influences.
Professional nursing staff with seniority at the centre of less than 10 years showed a more positive perception of all factors except Participation, and a more positive overall perception of the practice environment. In the work by de Pedro-Gómez et al.,14 on the contrary, nursing staff with between 2 and 10 years’ experience expressed the poorest perception. We must point out here that although in this study experience was captured differentiating between professional life and the current centre of employment, having found a link between the latter and perception of the practice environment, in de Pedro-Gómez's study this differentiation was not drawn, which may explain the disparity. In any case, this is matter for further research, as the controversy can be seen clearly on reviewing the literature. Wieck et al.27 in their study of the generational differences regarding stress in the working environment, the intent to leave the profession and job satisfaction, reached the conclusion that it is the younger nurses (born after the 80s) who suffer greater levels of stress (a circumstance directly related to job satisfaction), and likewise surpass their older colleagues in the intention to abandon the profession (it must be remembered that a nurse's age does not necessarily correspond to his or her experience). Schmalenberg and Kramer28 found no significant differences with regard to the number of years of experience of nurses at Magnet hospitals (better environment) and other hospitals without the recognition. Sexton et al.29 made an interesting analysis combining experience and academic level, reaching the conclusion that the higher the academic qualifications, the higher the perception of the practice environment, and further, that this difference increased with experience.
The findings of Sexton et al.29 are in line with the results of this study which, despite its limitations from the point of view of statistical significance (reduced number of subjects in the category Advanced Studies in Nursing), suggest that nurses with Master's or Bachelor's studies in Nursing have a better perception of the factors Participation and Managers Support, as well as a better overall perception of the working environment. Likewise, Schmalenberg and Kramer28 have shown that Magnet hospitals have a significantly higher percentage of nurses with Master's or Doctor's degrees.
This study provides knowledge about nursing practice environments in Primary Health Care, that is fundamental in encouraging a positive working climate defined as that which encourages continuity,26 promotes low stress levels27 and good physician/nurse relations,30 greater autonomy in nurses’ jobs30 and higher quality care.31
The fact that the highest scoring factor was Managers Support should serve to reinforce the impact of nurses’ leadership on results in patients. The role of nurse manager is key to establishing standards in the provision of care, through their comprehensive knowledge of the care requirements, through their experience in applying evidence in practice,32 through their implication with the institution, and through their integrating and motivating role towards the other nurses in the team.
In these economically difficult times that require severe cuts, health institutions, in order to obtain better health results and increase the efficiency of the health system, should invest in developing leadership styles that enable human resources optimization while guaranteeing an adequate workforce, both from a quantitative and a qualitative point of view.
FundingThe results presented here form part of a study that has been funded partially with the First Prize for National Research in Nursing (12th edition) from Hospital Universitario Marqués de Valdecilla (Santander) in 2010.
Conflict of interestThe authors have no conflict of interest to declare.