Brugada syndrome (BrS) is a rare, inherited cardiac disorder characterized by distinctive electrocardiographic (ECG) findings, including right bundle branch block and ST-segment elevations in leads V1–V3. It poses significant risks such as ventricular arrhythmias, syncope, and sudden cardiac arrest, with many cases incidentally detected. Chest pain is present in approximately 17% of cases, presenting diagnostic challenges.
Case presentationThis report presents a case of BrS in a patient with ischemic heart disease and discusses the management challenges in resource-limited settings. A 58-year-old Somali man presented with sudden-onset chest pain and associated symptoms. His history included ischemic heart disease and an appendectomy. Examination revealed restlessness and diaphoresis, with normal vital signs. Investigations showed normal troponin levels and an ECG indicating ST elevation in lead V1. Managed with acute coronary syndrome (ACS), he was referred for angiography, revealing mild coronary artery disease and normal ventricular function. Follow-up indicated recurrent headaches and financial constraints limited implantable cardioverter–defibrillator (ICD) placement. BrS is associated with an increased risk of ventricular arrhythmias.
Discussion and conclusionDiagnostic challenges include distinguishing it from ACS due to overlapping ECG patterns. Management options are limited, with ICD insertion and quinidine being primary modalities. Resource limitations, such as the lack of ICD services, complicate management. Ongoing debate surrounds the efficacy and safety of beta-blocker therapy. BrS presents diagnostic and therapeutic challenges, emphasizing the need for comprehensive management approaches. Tailored strategies are essential, particularly in resource-limited settings, necessitating further research to optimize patient outcomes.
El síndrome de Brugada (BrS) es un trastorno cardíaco hereditario raro, caracterizado por hallazgos electrocardiográficos distintivos, que incluyen bloqueo de rama derecha y elevaciones del segmento ST en las derivaciones V1-V3. Plantea riesgos significativos como arritmias ventriculares, síncope y paro cardíaco súbito, con muchos casos detectados incidentalmente. El dolor torácico está presente en aproximadamente el 17% de los casos, lo que presenta desafíos diagnósticos.
Presentación del casoEste informe presenta un caso de BrS en un paciente con enfermedad cardíaca isquémica y discute los desafíos de manejo en entornos con recursos limitados. Un hombre somalí de 58 años se presentó con dolor torácico de inicio súbito y síntomas asociados. Su historial incluía enfermedad cardíaca isquémica y una apendicectomía. El examen reveló inquietud y diaforesis, con signos vitales normales. Las investigaciones mostraron niveles normales de troponina y un ECG que indicaba elevación del ST en la derivación V1. Manejado como síndrome coronario agudo (SCA), fue referido para angiografía, revelando una enfermedad coronaria leve y una función ventricular normal. El seguimiento indicó dolores de cabeza recurrentes y limitaciones financieras que impedían la colocación de un DAI. El BrS está asociado con un mayor riesgo de arritmias ventriculares.
Discusión y conclusiónLos desafíos diagnósticos incluyen distinguirlo del SCA debido a patrones de ECG superpuestos. Las opciones de manejo son limitadas, siendo la inserción de DAI y la quinidina las modalidades principales. Las limitaciones de recursos, como la falta de servicios de DAI, complican el manejo. Existe un debate en curso sobre la eficacia y seguridad de la terapia con betabloqueadores. El BrS presenta desafíos diagnósticos y terapéuticos, enfatizando la necesidad de enfoques de manejo integral. Las estrategias personalizadas son esenciales, particularmente en entornos con recursos limitados, lo que requiere más investigación para optimizar los resultados de los pacientes.
Brugada syndrome (BrS) represents a rare yet potentially life-threatening inherited cardiac disorder characterized by a propensity for fatal cardiac arrhythmias. This syndrome manifests through distinctive electrocardiographic (ECG) findings, prominently including right bundle branch block and ST-segment elevations in the right precordial leads (V1–V3).1 The condition poses significant risks, as evidenced by numerous studies associating BrS with ventricular arrhythmias (VAs), syncope, and sudden cardiac arrest (SCA).2 Notably, a substantial proportion of individuals with BrS are incidentally detected, as most cases remain asymptomatic.2 Interestingly, chest pain episodes have been identified as a presenting symptom for approximately 17% of BrS diagnoses in the literature.3 However, achieving a definitive diagnosis of the underlying cause of chest pain in BrS patients remains elusive in many instances. It remains speculative whether such symptoms represent purely incidental non-cardiac manifestations or are indicative of concealed myocardial ischemia secondary to unrecognized vascular alterations in BrS.3 In this case report, we present a patient from Somalia with a history of ischemic heart disease who was incidentally diagnosed with BrS type A. Our objective is to delineate the challenges encountered in managing BrS and ischemia in resource-limited settings.
Presentation of the caseHistoryA 58-year-old man from Somalia presented with sudden-onset chest pain persisting for 6 h. He had no known chronic illnesses and described the pain as crushing in nature, with severity ranging from 9 to 8 on a scale of 10. He reported associated symptoms of nausea, sweating, restlessness, dizziness, and headache, along with epigastric pain. His past medical history included an appendectomy performed 20 years prior. There was a family history of ischemic heart disease stroke and sudden cardiac death in several relatives. Socially, he had a history of heavy smoking, totaling 35 pack-years, but had quit smoking 5 years ago.
Physical examinationOn examination, the patient appeared restless and diaphoretic but was oriented. Initial blood pressure was 150/80 mmHg, with other vital signs within normal limits. Cardiovascular examination revealed audible S1 and S2 without murmurs or added sounds. Respiratory examination showed clear chest with normal vesicular breathing. Abdominal examination revealed a soft abdomen with no tenderness or organomegaly.
InvestigationsTroponin levels were within normal limit and other laboratory findings included a white blood cell count of 14.8 × 103/μL, platelet count of 258 × 103/μL, creatinine level of 1.0 mg/dL, urea level of 29 mg/dL, sodium level of 134 mmol/L, and potassium level of 3.7 mmol/L. Serological tests for HBsAg, HCV, and HIV were negative.
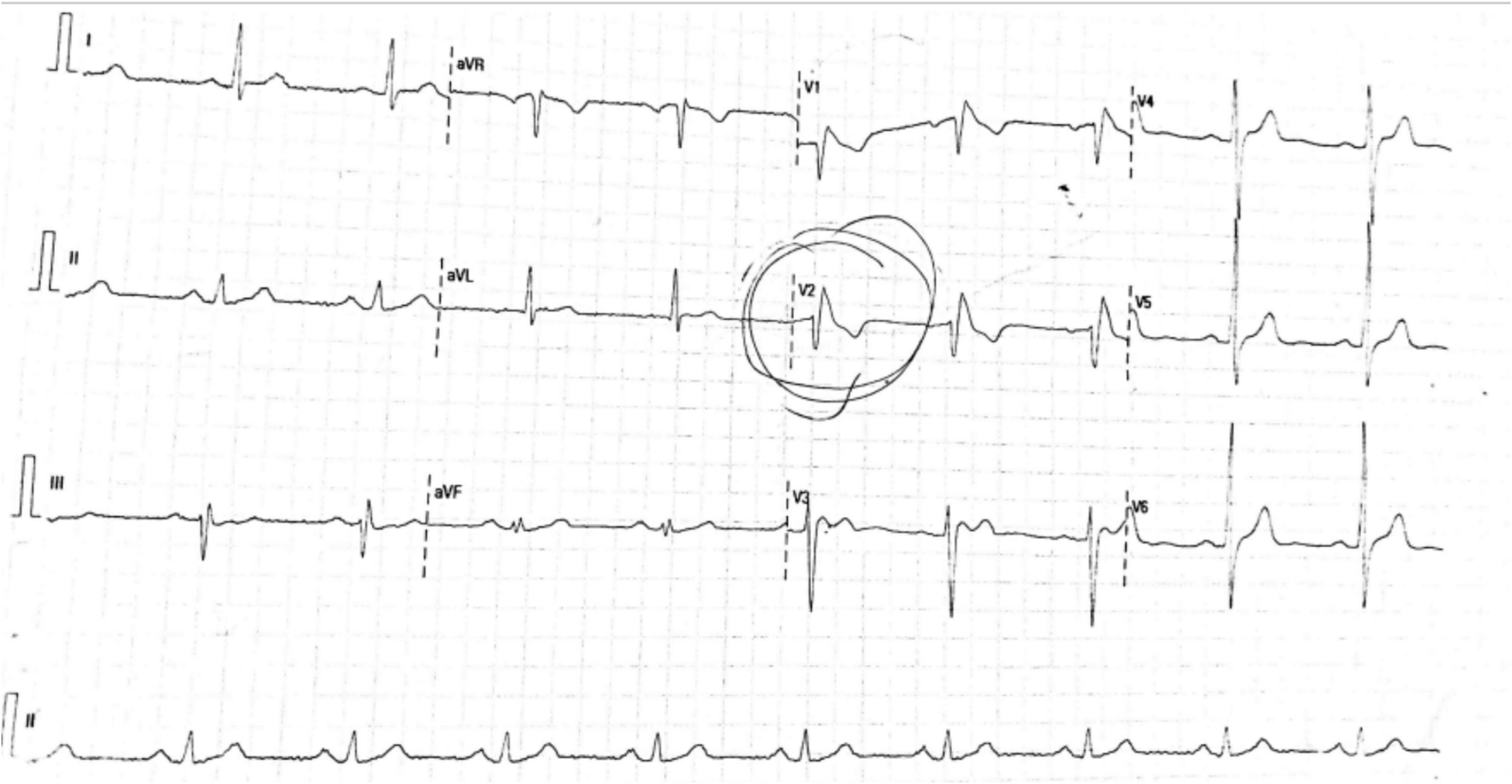
ECGThe electrocardiogram (ECG) revealed sinus rhythm with ST elevation in lead V1, transitioning to a saddle-back pattern (see Fig. 1).
ManagementThe patient was managed according to acute coronary syndrome (ACS) protocol, including administration of morphine (2 doses were required), aspirin, clopidogrel (loading and maintenance doses), heparin, nitroglycerin, and beta-blockers. He was referred for angiography to Indodargaar Metrocardiac Center.
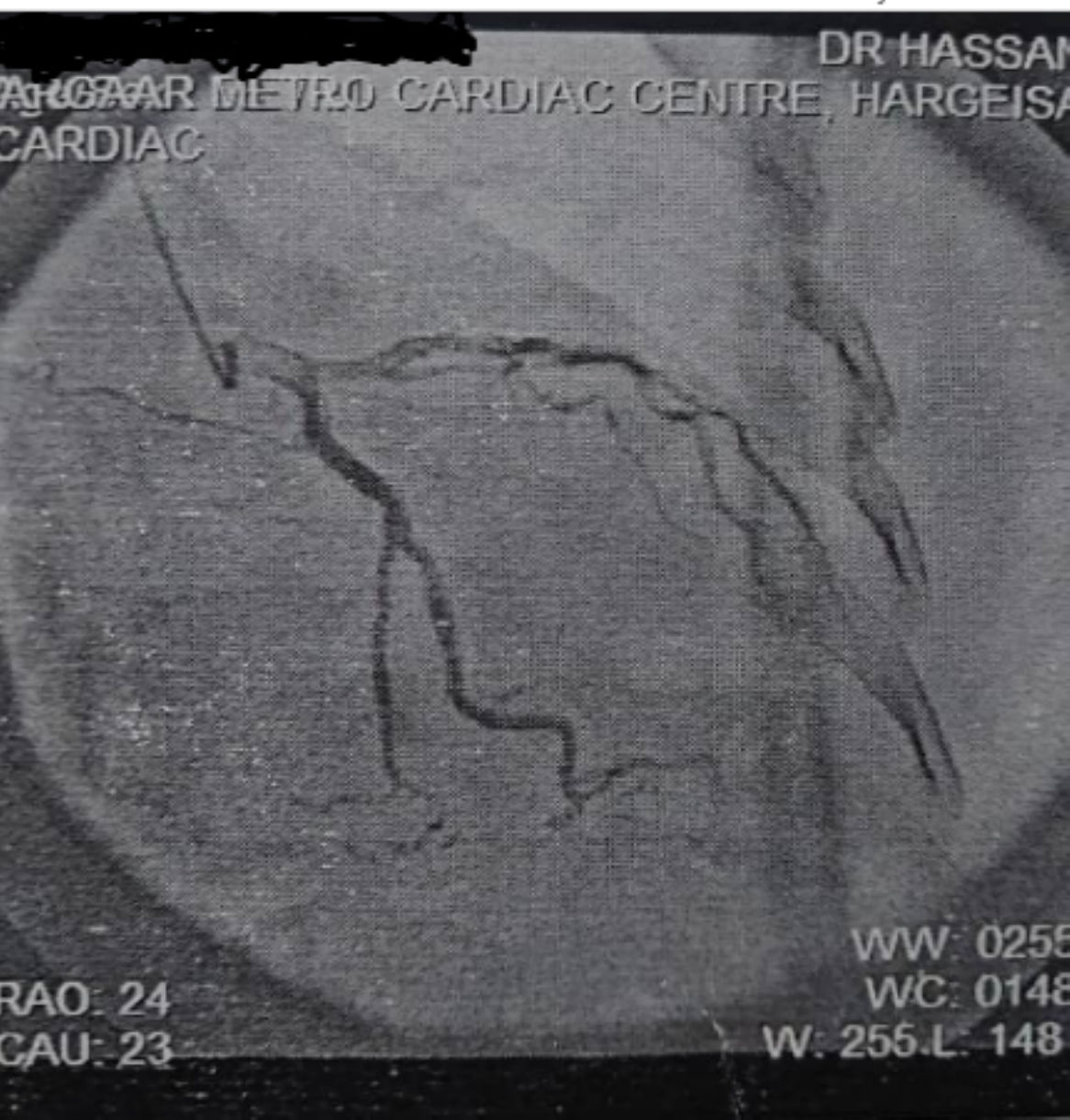
Cardiology assessmentEchocardiography revealed normal-sized chambers with no regional wall motion abnormality, normal right ventricular function, and intact interatrial and interventricular septa. Doppler findings showed trivial mitral regurgitation and tricuspid regurgitation with no pulmonary artery hypertension. Coronary angiography revealed mild coronary artery disease, with a normal left main coronary artery and a Type 3 vessel left anterior descending artery with a 50% stenosis in the mid-segment. The left circumflex artery was non-dominant with mild disease in the proximal segment. The posterior descending artery and left ventricular branch were normal (see Fig. 2).
ImpressionThe patient was advised to undergo optimal medical management for mild coronary artery disease and to travel abroad for ICD implementation, since it is not available in Somaliland.
TimelineFollow-upAfter a 3-month follow-up period, the patient exhibited recurrent episodes of headache, prompting clinicians to consider a potential adverse reaction to isosorbide mononitrate. Upon discontinuation of the medication, a significant improvement in symptoms was observed, including the absence of chest pain for the subsequent 3 months. However, due to financial constraints, the patient opted against pursuing implantable cardioverter-defibrillator (ICD) placement through travel.
DiscussionBrS is an autosomal dominant genetic disorder characterized by abnormal findings on the surface ECG. It is associated with an augmented risk of ventricular tachyarrhythmias and sudden cardiac death, placing it in a pivotal position within contemporary cardiology.4 Notably, the intricate diagnostic landscape, marked by 2 discernible patterns of ST elevation known as the “coved type” and “saddle back” configurations, underscores the complexity inherent in discerning BrS from ACS.4 While ACS and BrS present with distinct ECG patterns, the manifestation of right ventricular ST-segment alterations in acute myocardial ischemia further complicates diagnostic clarity.5,6 Moreover, the potential coalescence of BrS with vasospastic angina exacerbates diagnostic intricacies, necessitating a nuanced diagnostic approach.6 Research findings, such as those by Kimie Ohkubo et al., elucidate the intricate interplay between significant coronary artery stenosis and BrS, emphasizing the imperative for meticulous diagnostic delineation amidst overlapping clinical features.6
The management of BrS poses formidable challenges due to the limited therapeutic modalities available, primarily encompassing ICD insertion and quinidine administration.7 While ICD implantation is considered indispensable in symptomatic BrS cases, the judicious utilization of ICDs in asymptomatic patients necessitates scrupulous consideration, often guided by electrophysiological studies.8 The pivotal role of ICDs in mitigating the risk of sudden cardiac death is extensively documented in the literature.9 However, the conspicuous absence of ICD implantation services in certain regions, such as Somaliland, accentuates the pressing need for enhanced cardiac care infrastructure to cater to BrS patients and individuals with other arrhythmic conditions.8 Concomitantly, guidelines advocated by the European Society of Cardiology underscore the necessity of a comprehensive approach to patient care, encompassing robust educational initiatives aimed at fostering awareness of modifiable or precipitating factors associated with BrS.8
In the management of BrS in resource-limited settings in sub-Saharan Africa, strategies vary depending on the available resources. A series of cases from countries like Ivory Coast and Congo demonstrated effective management approaches. In these settings, patients, particularly those who are symptomatic or at high risk despite being asymptomatic, received ICDs when possible.10 For instance, an ICD was successfully used in a patient from Ivory Coast, where it provided appropriate discharges in response to ventricular fibrillation. In situations where ICD implantation was not feasible, alternative management strategies were employed, with patient being treated with quinidine, which proved effective. Diagnostic methods commonly used included the ajmaline intravenous test and electrophysiological studies, essential for confirming the diagnosis and assessing arrhythmia risk. Moreover, patients were managed in well-organized outpatient care units, ensuring continuous monitoring and follow-up. This comprehensive approach highlights the adaptability and resourcefulness required to manage BrS effectively in resource-limited settings, ensuring patients receive appropriate care despite the constraints.10
The discourse extends to therapeutic considerations, notably pertaining to beta-blocker therapy. While long-term beta-blocker therapy post-myocardial infarction has been shown to reduce mortality in ACS patients,11 its applicability in BrS management remains a subject of debate.12 Beta-blockade in BrS patients may exacerbate ST-segment elevation and inadequately control arrhythmias, prompting cautious utilization until ICD implantation.12,13 This multifaceted discussion underscores the ongoing deliberations within the cardiology community regarding optimal therapeutic strategies for BrS patients.
ConclusionBrS poses diagnostic and therapeutic challenges in cardiology. Electrocardiographic patterns like the “coved type” and “saddle back” complicate differentiation from ACS. Co-occurrence with conditions such as vasospastic angina adds to diagnostic complexity. Management typically involves ICD insertion and quinidine administration, but ICD implantation decisions for asymptomatic patients require careful consideration. Limited access to ICD services underscores the need for improved cardiac care infrastructure. Therapeutic debates, especially regarding beta-blocker therapy, persist due to efficacy and safety uncertainties. Tailored approaches are essential for optimizing outcomes in BrS management.
Authors' contributionsDr. Abdirahman Ibrahim Said provided medical care to the patient, conducted history taking, and supervised the patient's hospital stay and follow-up. Dr. Abdirahman Omer Ali, Abdiwahaab Osman, Dr. Muna Abdilahi, and Dr. Hassan Sh. Abdirahman contributed to the development of the manuscript. All authors critically reviewed and approved the final version of the manuscript.
Ethical approvalEthical approval for this study was obtained from the BRH Ethical Committee, authorized by the Ministry of Health in the Awdal Region, Somaliland (Registration number BRH 50/2024).
Consent for Publication StatementThe patient provided informed consent after a thorough explanation of the purpose and implications of the consent. The patient was assured that their information would remain confidential and solely utilized for scientific purposes.
DeclarationsWe hereby affirm that this manuscript has not been submitted to any other journal for publication.
FundingNo external funding was received for this study.
We express our sincere gratitude to Dr. Said Ahmed Walhad, Principal of the College of Health Sciences, for his valuable support and guidance throughout this endeavor. Additionally, we extend our special appreciation to Dr. Abdirahman Warfaa and Dr. Hassan Awil Yusuf, along with the entire cardiology team, for their expertise and assistance in the consultation and management of the patient. Their contributions have been instrumental in the comprehensive care provided to the patient and the success of this case report.