Situs inversus totalis (SIT), a rare congenital disorder, involves complete reversal of the heart's position and mirrored arrangement of visceral organs. Early diagnosis is crucial for managing complications like transposition of the great vessels and Kartagener syndrome, marked by bronchiectasis and sinusitis due to ciliary dysfunction.
Case presentationA 52-year-old male with diabetes mellitus presented with large amounts of watery diarrhea, vomiting, dizziness, and palpitations. He managed his diabetes with 70 units of insulin daily and had a history of chronic obstructive pulmonary disease. Physical examination revealed hypotension, tachycardia, and a right-sided apex beat. Investigations, including chest X-ray, ultrasound, and ECG, confirmed dextrocardia with situs inversus and hypovolemic shock secondary to acute gastroenteritis. The patient responded well to treatment and was discharged on the second day, continuing diabetic management.
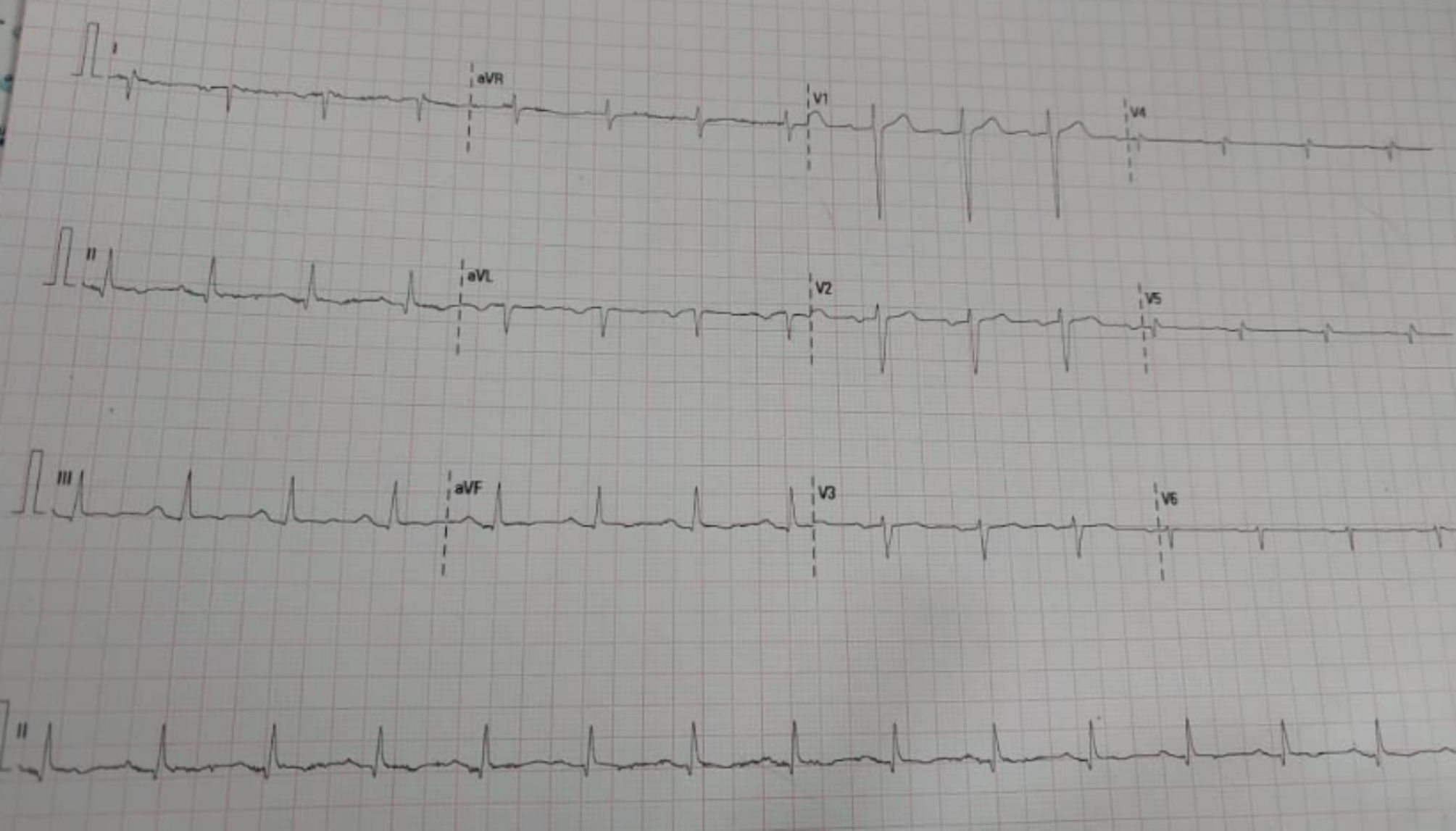
DiscussionSIT is a genetically determined anomaly with an incidence ranging from 1:35 000 to 1:1400, averaging 1:10 000, with a higher prevalence in males. Many patients are asymptomatic, with the condition often detected incidentally. Diagnostic imaging techniques, including chest radiography, CT scans, MRI, and ultrasonography, are crucial in confirming SIT. ECG findings, such as right-axis deviation and reversed QRS complexes, are valuable in diagnosing dextrocardia. Patient education is essential to empower individuals with SIT to navigate their healthcare, prevent complications, and reduce anxiety.
ConclusionSIT poses diagnostic challenges due to its incidental discovery. Accurate diagnosis relies on thorough imaging and clinical evaluation. Patient education is vital for informed care and anxiety reduction. Case reviews underscore the importance of healthcare providers' readiness to diagnose SIT effectively despite unrelated symptoms.
Situs inversus totalis, un trastorno congénito raro, implica la inversión completa de la posición del corazón y la disposición en espejo de los órganos viscerales. El diagnóstico temprano es crucial para manejar complicaciones como la transposición de los grandes vasos y el síndrome de Kartagener, caracterizado por bronquiectasias y sinusitis debido a la disfunción ciliar.
Presentación del CasoUn hombre de 52 años con diabetes mellitus presentó grandes cantidades de diarrea acuosa, vómitos, mareos y palpitaciones. Controlaba su diabetes con 70 unidades de insulina diarias y tenía antecedentes de EPOC. El examen físico reveló hipotensión, taquicardia y un latido apical en el lado derecho. Las investigaciones, incluyendo radiografía de tórax, ecografía y ECG, confirmaron dextrocardia con situs inversus y choque hipovolémico secundario a gastroenteritis aguda (AGE). El paciente respondió bien al tratamiento y fue dado de alta al segundo día, continuando con el manejo de la diabetes.
DiscusiónSIT es una anomalía determinada genéticamente con una incidencia que varía de 1:35,000 a 1:1400, promediando 1:10,000, con una mayor prevalencia en hombres. Muchos pacientes son asintomáticos, con la condición a menudo detectada incidentalmente. Las técnicas de diagnóstico por imagen, incluyendo radiografía de tórax, tomografías computarizadas, resonancia magnética y ultrasonografía, son cruciales para confirmar SIT. Los hallazgos del ECG, como la desviación del eje derecho y los complejos QRS invertidos, son valiosos para diagnosticar la dextrocardia. La educación del paciente es esencial para empoderar a las personas con SIT a navegar su atención médica, prevenir complicaciones y reducir la ansiedad.
ConclusiónSitus inversus totalis (SIT) presenta desafíos diagnósticos debido a su descubrimiento incidental. Un diagnóstico preciso depende de una evaluación clínica e imagenológica exhaustiva. La educación del paciente es vital para una atención informada y la reducción de la ansiedad. Las revisiones de casos subrayan la importancia de que los proveedores de atención médica estén preparados para diagnosticar SIT de manera efectiva a pesar de los síntomas no relacionados.
Situs inversus totalis (SIT), also known as dextrocardia with situs inversus, is a rare congenital disorder characterized by the complete reversal of the heart's anatomical position to the right side, along with the inverse rotation of all visceral organs.1 This condition has a prevalence of approximately 0.01% within the general population. Early diagnosis is crucial due to its significant implications for patient management, including considerations for transplantation and various surgical procedures, as well as for identifying potential complications.2 Individuals diagnosed with SIT are at a notable risk of congenital cardiac diseases, predominantly characterized by conditions such as transposition of the great vessels. Moreover, a significant proportion of individuals with this congenital anomaly also exhibit Kartagener syndrome, which encompasses bronchiectasis and sinusitis due to inherent ciliary dysfunction.3,4 This report discusses a patient who was diagnosed with SIT incidentally.
Case presentationHPIA 52-year-old male with a known history of diabetes mellitus, previously diagnosed with insulin-resistant diabetes, presented with complaints of diarrhea. The patient reported experiencing large amounts of watery diarrhea, without the presence of blood, and described the consistency as normal. Additionally, he experienced several episodes of vomiting, dizziness, and palpitations.
Past medical historyThe patient has a history of diabetes mellitus, previously managed with 210 units of insulin daily. Recently, he has lost weight and currently manages his diabetes with 70 units of insulin daily. The patient is also diagnosed with chronic obstructive pulmonary disease (COPD).
Past surgical historyThe patient has no history of surgeries and has not received any blood transfusions.
Family and social historyThe patient was a heavy smoker in the past, but he has quit it 5 years ago. He is a father of 3 children.
Physical examinationThe patient's blood pressure was 90/70 mmHg, pulse rate was 109 beats per minute, temperature was 35.6 °C, and SpO2 was 98%. The patient appeared ill. Cardiovascular examination revealed an apex beat in the 5th intercostal space at the mid-clavicular line on the right side, with audible S1 and S2 heart sounds, no murmurs, but noted tachycardia. The respiratory system examination showed a clear chest with no crepitations or wheezes. The abdomen was soft and non-tender. A neurological examination indicated normal cranial nerves and motor and sensory functions.
InvestigationsThe patient underwent several investigations:
- 1.
Complete blood count (CBC): Normal
- 2.
Stool analysis: Normal
- 3.
HbA1c: 8.5%
- 4.
Chest X-ray: The heart was located on the right side (dextrocardia), with pulmonary infiltration in the bilateral lower lobes (Fig. 1).
- 5.
Ultrasound findings: The imaging confirmed the liver's abnormal positioning on the left side of the abdominal cavity (Fig. 2).
- 6.
ECG: Showed R waves in aVR and S waves in V6 and V5 with right axis deviation. (see Fig. 3).
The patient was diagnosed with dextrocardia with situs inversus and hypovolemic shock secondary to acute gastroenteritis (AGE).
ManagementThe patient was initially treated for hypovolemic shock secondary to AGE and managed for diabetes mellitus. Acute treatments were administered, and the patient responded well. He was subsequently discharged on the second day and is now under diabetic clinical management.
DiscussionSIT is a rare congenital condition characterized by the complete reversal of all thoraco-abdominal organs. While functional malformations associated with this condition are primarily cardiovascular, significant visceral or structural deformities can also occur. SIT is a genetically determined anomaly, with an incidence ranging from 1:35 000 to 1:1400, and an average of 1:10 000, with a higher prevalence in males.5 A patient presented with complaints of diarrhea and vomiting and SIT was diagnosed incidentally, unrelated to the primary concerns of the patient. This unique finding in the case underscores that many patients with SIT often have the condition detected incidentally. Most patients with SIT lead normal, healthy lives, and the detection of the condition is often incidental. As an example, a case describes a lady diagnosed with SIT at the age of 84 years, incidentally, when she was imaged as part of the evaluation for carcinoma of the urinary tract (case 6). This case illustrates that SIT can remain undiagnosed until late in life, especially when it does not present any symptoms directly related to the reversal of organ placement. In another instance, a case report from Cape Coast Teaching Hospital describes a diabetic patient with chest pain and cough who was incidentally diagnosed with SIT. The detection was made during routine examinations, highlighting the importance of physician vigilance in diagnosing SIT, especially in patients presenting with unrelated symptoms.6 While most patients with SIT lead normal, healthy lives, these cases emphasize the necessity for healthcare providers to consider the possibility of SIT in patients, even when their presenting symptoms are not directly related to the anatomical anomaly. The reviewed cases indicate that SIT can go undetected for many years and often comes to light during investigations for other medical condition. The ability of a physician to diagnose SIT can be greatly enhanced with various imaging techniques. Chest radiography, for example, is a crucial tool that typically reveals dextrocardia, with the heart's apex pointing to the right and both the aortic arch and stomach bubble also located on the right. CT scans provide a detailed view of the mirror-image anatomy of the internal organs, making it easier to confirm SIT. MRI is another valuable technique, complementing echocardiography and angiography.1 It is particularly useful for showing abnormalities related to congenital heart disease and for aiding in surgical planning. Additionally, ultrasonography highlights the mirror-image arrangement of the abdominal organs. Fetal ultrasonography can even detect SIT before birth, alerting physicians to the potential for primary ciliary dyskinesia or congenital heart disease, prompting further evaluation.1 ECG is valuable in diagnosing SIT as the findings can indicate the presence of dextrocardia. In patients with dextrocardia, the standard 12-lead ECG will show marked right-axis deviation of the P wave and QRS complex, with lead I frequently demonstrating a largely negative QRS complex and inverted P and T waves. The QRS complexes in leads aVR and aVL are reversed, resulting in a positive R wave in lead aVR. The typical QRS complex progression in the precordial leads is reversed, most noticeably in V4–V6. There is a loss of amplitude toward V6, and V1 and V2 are also reversed.7 Patient education in situs inversus is crucial to empower individuals to navigate their healthcare effectively, thereby preventing potential challenges and confusion in medical care.8 Educating patients about their condition also plays a pivotal role in alleviating anxiety associated with their diagnosis. In our case, we provided comprehensive information to the patient who had not previously been aware of his condition, ensuring he understood its implications.
ConclusionIn summary, SIT is a rare congenital condition that, while typically asymptomatic, presents unique diagnostic challenges due to its often incidental detection. Comprehensive imaging techniques and vigilant clinical evaluation are essential for accurate diagnosis. Furthermore, patient education is crucial in ensuring informed healthcare decisions, reducing anxiety, and preventing potential complications associated with this condition. The reviewed cases highlight the importance of awareness and preparedness among healthcare providers to manage SIT effectively, even when presenting symptoms appear unrelated.
Manuscript SubmissionWe confirm that this manuscript has not been submitted to any other journal for publication.
Authors' contributionsDr. Abdirahman Ibrahim Said provided medical care to the patient, conducted history taking, and supervised the patient's hospital stay and follow-up. Dr. Abdirahman Omer Ali, Dr. Abdirahman Ibrahim Said, Dr. Amtarahman Ibrahim Said, and Dr. Hassan Sh. Abdirahman contributed to the development of the manuscript. All authors critically reviewed and approved the final version of the manuscript.
Ethical approvalEthical approval for this study was obtained from the Borama Regional Hospital (BRH) Ethical Committee, authorized by the Ministry of Health in the Awdal Region, Somaliland (Registration number BRH 100/2024).
Consent for PublicationInformed consent was obtained from the patient after a thorough explanation of the study's purpose and implications. The patient was assured that their information would remain confidential and used solely for scientific purposes.
FundingThis study did not receive any external funding.
We extend our special appreciation to Dayib Barkhad, Mahmed Bashiir and Fadxiye Nuur for their expertise and assistance in the consultation and management of the patient. Their contributions were instrumental in the comprehensive care provided and the success of this case report.