Aorto-right ventricular fistula is a rare condition that communicates the ascending aorta to the right ventricle. This case describes a 31-year-old female attended at the outpatient clinic with a complain of dyspnea and edema in the lower limbs lasting about 2 months. Physical evaluation showed a holosystolic heart murmur on cardiac auscultation. Echocardiography and cardiac catheterization revealed a communication between the right coronary sinus to the right ventricular outflow tract. The patient underwent cardiac surgical treatment to correct the defect, in which fistula tissue was resected and the orifice was closed with bovine pericardium.
La fístula aortoventricular derecha es una entidad poco común que comunica la aorta ascendente con el ventrículo derecho. Se describe el caso de una mujer de 31 años que acudió a consulta externa con un cuadro de disnea y edema en miembros inferiores de aproximadamente 2 meses de duración. La evaluación física mostró un soplo cardíaco holosistólico en la auscultación cardíaca. La ecocardiografía y el cateterismo cardíaco revelaron una comunicación entre el seno coronario derecho y el tracto de salida del ventrículo derecho. La paciente fue intervenida para corregir el defecto; en la operación se resecó tejido de la fístula y se cerró el orificio con pericardio bovino.
Aorto-right ventricular fistula (ARVF) is a very rare condition which communicates the ascending aorta to the cavity of the right ventricle.1–4 The Sinus of Valsalva fistula was first described in 1839 and has a general incidence about 0.14–0.96% of all cardiac operations.3 The structure most frequently involved is the right coronary sinus, accounting for 64%, followed by the noncoronary sinus.1 It's known that the perforation often communicates the aorta to the right ventricle, but it can also do, rarely, to the right atrium, left chambers or even to pericardium.1,5
This condition is mostly like associated to ruptured aneurysm of Sinus of Valsalva, complication of endocarditis, chest trauma, aorta dissection or complication of another cardiac procedures as valve replacement, Ventricular Septal Defect (VSD) correction and Transcatheter Aortic Valve Replacement (TARV), among others.2,6,7 This case describes an adult with ARVF without any of these causes above and with no other abnormalities on the aortic valve and root, ascending aorta or ventricular septum.
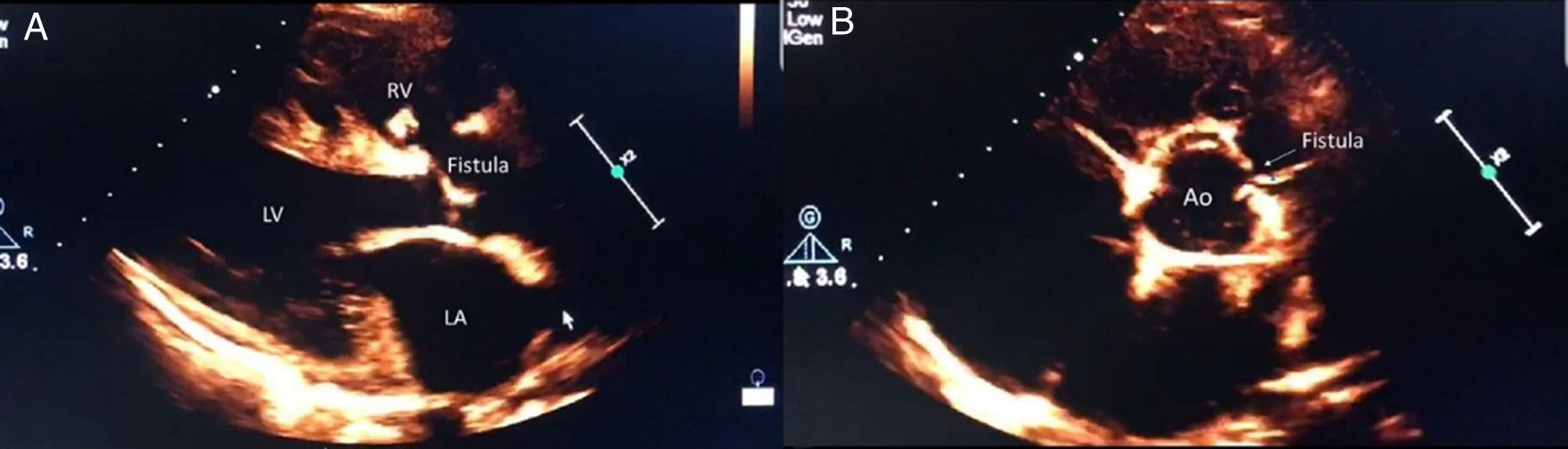
Case reportA 31-year-old women with unremarkable medical history was consulted at the ambulatory complaining of dyspnea and edema of the lower limbs lasting about 2 months. The patient had no history of endocarditis, trauma, previous surgery or other heart disease diagnosed so far. On physical evaluation, cardiac auscultation showed a rude, high-frequency holosystolic heart murmur, pancardiac, 4+/6+ according to Levine's scale, and bilateral lower limbs edema. Transthoracic echocardiography was performed, which showed (I) moderate atrial dilatation, (II) secondary increased pulmonary blood flow and (III) high-pressure blood flow directed from the right Valsalva sinus to the right ventricle, with intense retrograde flow over pulmonary valve, resulting in its functional insufficiency, see Fig. 1A and B.
Echocardiography images showing communication between the right coronary sinus and the right ventricle. (A) Highlights the fistula from the sinus of valsava to the right ventricle by a longitudinal paraesternal axis. (B) Shows the communication by a transverse paraesternal axis. RV, right ventricle; LV, left ventricle; LA, left atrium; Ao, aorta.
Decided for her admission to clinical compensation and diagnostic complementation. After clinical improvement, cardiac catheterization of the left and right chambers was performed, which revealed (I) coronary arteries free of atherosclerotic disease, (II) increased blood flow from the aorta to right ventricular cavity, (III) right ventricular diastolic overload, (IV) moderate functional tricuspid valve incompetence and (V) appearance of increased pulmonary blood flow. Hence, it was decided for surgical approach to correct the defect.
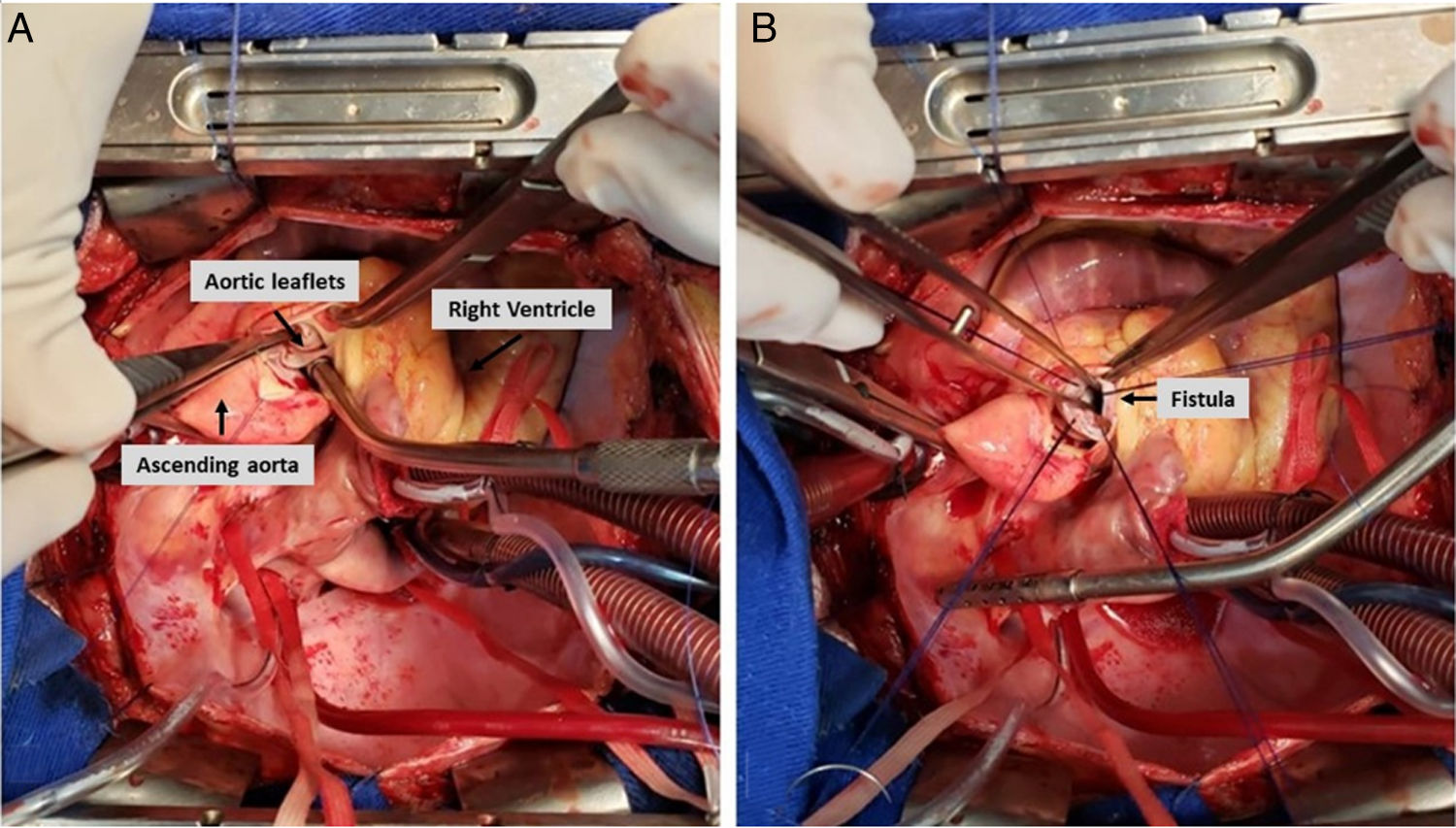
Surgical access was performed by median longitudinal sternotomy, installation of extracorporeal circulation circuit with aortic cannula positioned in ascending aorta and bicaval venous drainage. Hypotermia up to 32°C, transverse aortotomy, identification of the orifice in the right Valsalva sinus of the right coronary leaflet, with communication to the right ventricle outflow tract. The fistula tissue was resected and the orifice was closed with bovine pericardium and prolene 5/0 suture, see Fig. 2A and B.
The surgery had no complications during operation, and the patient was discharged at the fifth day after the procedure. In the postsurgical outpatient evaluation, the patient was asymptomatic, and the echocardiography three months later showed: (I) left atrium: 36mm; (II) diameter of right ventricle: 18mm; (III) final diastolic diameter of left ventricle: 42mm; (IV) final systolic diameter of left ventricle: 28mm; (V) ejection fraction of left ventricle: 62%; (VI) soft aortic valve regurgitation; (VII) absence of flow between the sinus of valsalva to the right ventricle.
DiscussionThe Congenital Aorto-Right Ventricle Fistula is a defect on the wall of the aorta and, although there is no definitive etiology for this anomaly, it is probably caused by its weakness throughout the development and is present at birth but may manifest clinically at any age. The abnormalities of the Sinus of Valsalva are characterized into three different groups: (1) unruptured aneurysm of the Sinus of Valsalva, (2) aneurysm of the Sinus of Valsalva with intracardiac or extracardiac rupture, and (3) intracardiac or extracardiac fistula of the Sinus of Valsalva.1,5
Meyer and colleagues1 made a survey about the procedures realized at the Texas Heart institute from April 1956, to September 1973. They found 45 patients with aneurysm and/or fistula of the Sinus of Valsalva, representing 0.43% of all procedures which were required cardiopulmonary bypass. Of the 45 patients in the group, 22 had an unruptured aneurysm, whereas 10 and 13 had a ruptured aneurysm and a simple fistulous communication, respectively. On the other hand, according to Walpot and contributors6 and Nishi et al.,5 the major cause of an aorto-cardiac fistula is a rupture of an aortic sinus aneurysm, accounting for 76% of the cases.
Many patients can be asymptomatic, but the typical symptoms are like Congestive Heart Failure (CHF). A pain in the chest and a sudden onset of the symptoms point to a ruptured aneurysm. It is possible to hear a “to-and-fro” murmur on cardiac auscultation with a systolic and diastolic thrill. The diagnosis is usually taken by transthoracic or transesophageal echocardiography, cardiac catheterization with aortography, computed tomography or magnetic resonance imaging (MRI), revealing a left-to-right shunt.
It is important to differentiate the ARVF from the Aorto-Right Ventricular Tunnel (ARVT). This condition, as the first, communicates the aorta to the right ventricle, however the second one's perforation arises above the sinutubular junction instead and runs into extra-cardiac tissues addressed to ventricular chambers, forming a conduit that by-passes the sinutubular junction. According to McKay et al.,8 the origin of the tunnel from the ascending aorta serves to differentiate it from rupture of an aneurysmal Sinus of Valsalva. Most part of the aorto-ventricle tunnel communicates the aorta to the left ventricle (90%), and just a small part of the cases do to the right ventricle.9 In the other hand, some surgeons consider that apart from fistulae secondary to infection, trauma or post surgical, most cases are a manifestation of a ruptured Sinus of Valsalva. While some authors use the term aorto-ventricular tunnel, others say that these terms are sinonimous and do not correspond to a different pathology. In their opinion the right term is ruptured Sinus of Valsalva. In the ARVF, the communication is localized below the sinutubular structure, where the abnormal pathway remains completely within the heart.8
The surgical correction is the treatment of choice. If promptly diagnosed and treated, it is possible to avoid major morbidity resulting from CHF caused by left-to-right shunt.2 Even in asymptomatic patients, closure of the fistula is recommended in low surgical risk person due to the low rate of procedure complications and the risk of heart failure, bacterial endocarditis, pulmonary vascular disease, aneurysm formation and spontaneous rupture.3 Currently, an alternative of treatment is transcatheter closure, but it is required more studies to analyze the optimal management.2,5
Consent statementThe patient gave her consent for clinical information relating to this case to be reported in a medical publication.
Financial supportNo financial support.
Conflict of interestsNo conflict of interest.