Ectopia cordis is an extremely rare congenital cardiac malformation in which heart is partially or completely out of the thoracic cavity. We report a case of thoracic ectopia cordis diagnosed in a prefectoral hospital birthroom, located at north Togo, 400km from Lome. It is the first case documented in a new born in our country.
La ectopia cordis es una anomalía cardíaca congénita extremadamente rara en la que el corazón se encuentra parcial o totalmente fuera de los límites de la caja torácica. Presentamos un caso de ectopia cordis torácica diagnosticado al nacer en un hospital de la prefectura del norte de Togo, a 400km de Lomé (TOGO). Este es el primer caso documentado en un recién nacido en nuestro país.
Ectopia cordis is an extremely rare congenital cardiac malformation in which heart is partially or completely out of the thoracic cavity. The estimated prevalence of ectopia cordis is 5–8 per million live births.1,2 Four types have been described: cervical (5%), thoracic (65%), abdominal (10%) and thoraco-abdominal (20%).3 The thoracoabdominal type is generally associated with Cantrell's pentalogy or one of its variants including a bifid sternum, a diaphragmatic and anterior abdominal wall defect as well as an intracardiac malformation.4 We report a case of thoracic ectopia cordis, diagnosed in Bassar delivery room, in the north of Togo. It is the first case documented in a new born in our country.
Case presentationA 10-hour-old, vaginally delivered full-term female neonate was referred from Bassar departmental hospital (400km from Lome) to Sylvanus Olympio University Hospital (Lome) after finding a beating heart outside the thoracic cavity.
She was the youngest of two children, the 07 years old brother having no visible malformation. The father was 28 years old and the mother 27 years old. There was no history of consanguinity. There was no family history of any such or related congenital heart diseases She had no known exposure to teratogens. The mother also had no history of chronic ill health. The pregnancy was regularly followed up in prenatal consultations from the 2nd month. The only obstetric ultrasound done at the 6th month did not detect any abnormality.
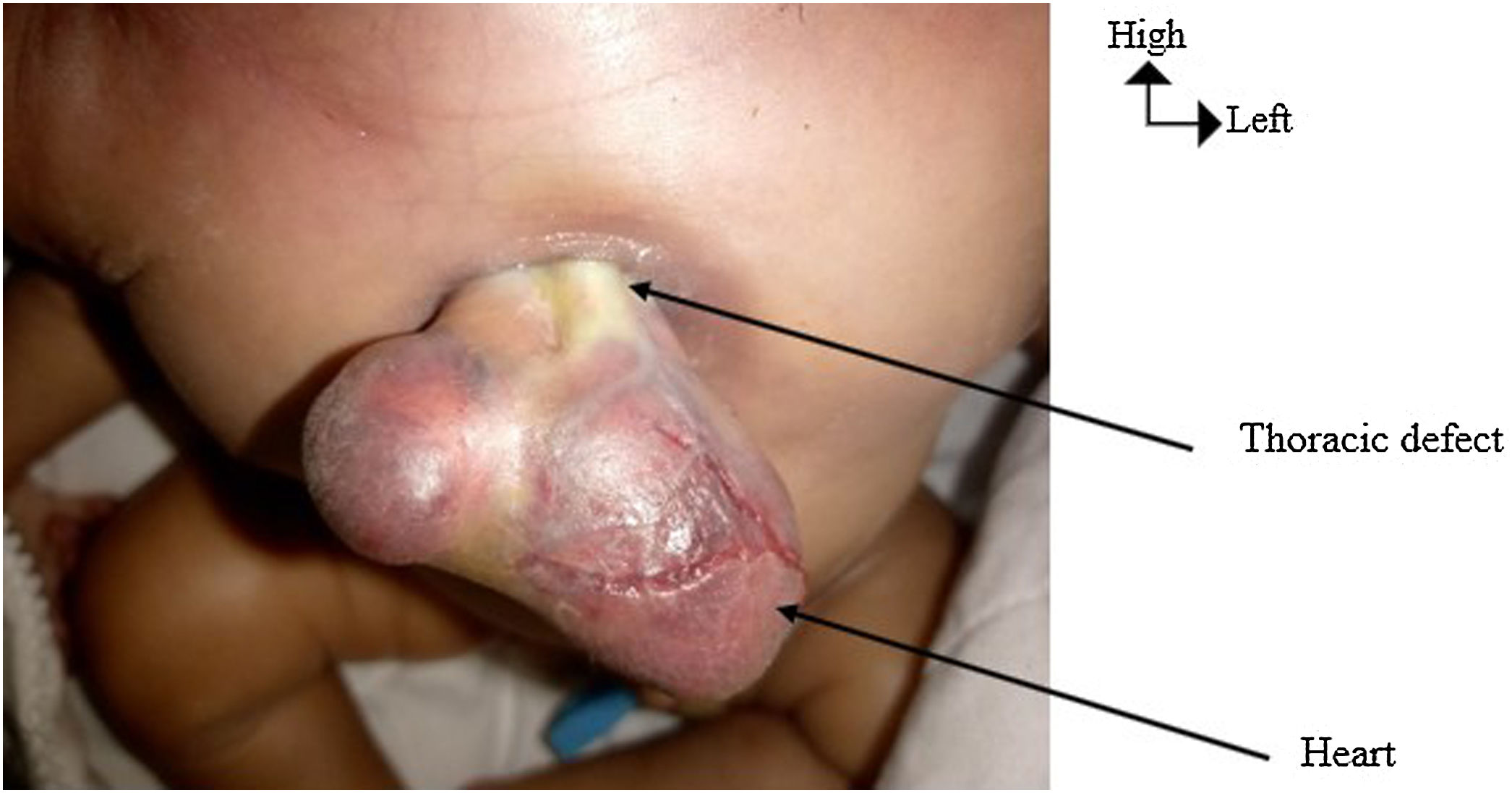
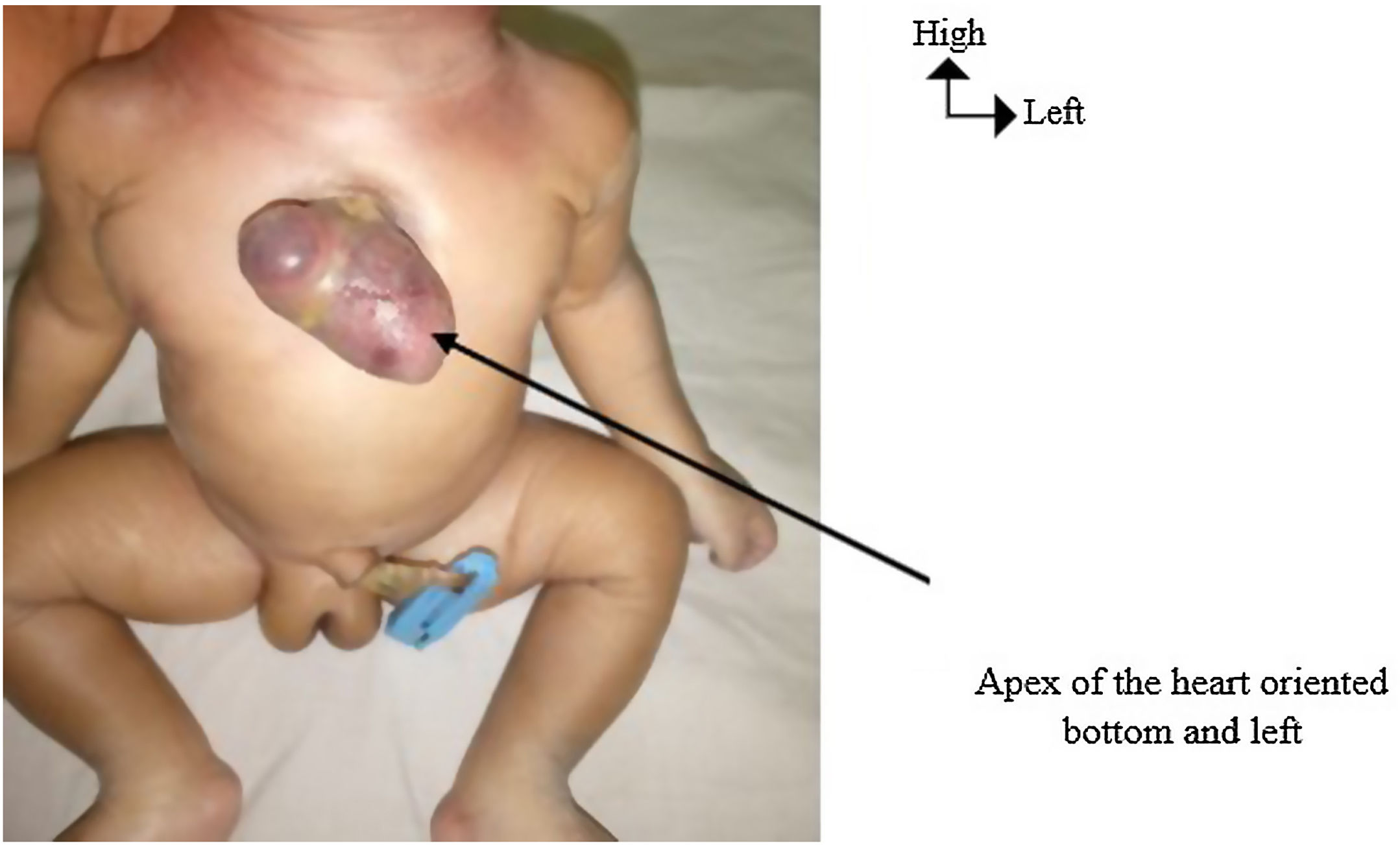
On clinical examination in birthroom, measurements were normal (Weight: 3000g; Height: 50cm; Cranial perimeter: 35cm); there was no difficulty in breathing or cyanosis. The patient was referred after the neonatal cleansing and wrapping with a clean cloth. They attempt the referral hospital by public transport vehicle. She died at her 22nd hour after birth, about 30min before their arrival at the reference center. At the post-mortem examination at the Sylvanus Olympio University Hospital, there was a defect in the middle of the sternum. The defect was 2cm in diameter. The heart burst through this defect and was normal in appearance (Fig. 1). There was no sternal bifidity. The apex of the heart was oriented bottom and left (Fig. 2). It was not covered with a serous membrane or a skin (Fig. 1). It had no abdominal defect. There were no other visible external malformations. No imaging assessment was performed. No autopsy was performed due to lack of parental consent.
Ectopia cordis is a rare congenital abnormality.1 Ectopia cordis was first observed 5000 years ago. However, authors notably Shad et al.2 and Byron et al.3 report that Haller was the first to use the term ectopia cordis to describe this malformation in 1706.
This malformation is described as a partial or complete malposition of the heart outside the chest. Byron3 classified ectopia cordis into four types: cervical, thoracic, thoracoabdominal and abdominal. In the case described, the heart burst through a defect located on the anterior thoracic wall. It was therefore a thoracic type. This thoracic type was explained embryonically by the rupture of the chorion at 3 weeks of gestation with resultant compression of the thoracic cavity and failure of descent of the heart at this stage.4 The possibility of amniotic bands is also ascribed.
Concerning our patient as in most of the cases described in literature, it was a sporadic case and no familial recurrence has been reported.5 Most of cases described in literature had associated cardiac malformations such as ventricular or atrial septal defect, pulmonary stenosis or atresia, tetralogy of Fallot, right ventricular diverticulum, left superior vena cava, and double right ventricular outflow tract.6 The non-performed autopsy did not allow us to assess any eventually internal cardiac malformations. Concerning extra cardiac malformations, the rest of the sternum was normal. There was no associated abdominal defect.
Majority of patients are stillborn or die within hours or days after birth.5,7,8 This was the case of our patient who died 22h after birth. Survey depends on the type of ectopia cordis, the capacity of thoracic cavity, compression or not of large cardiac blood vessels, presence or not of skin covering and presence or not of associated extra cardiac malformations.9 There are also some factors specific to developing countries that affect more the prognosis of this affection such as difficulty of patient's conditioning, difficulty of accessing to medical transport, delivery at home.10 Survival cases have been reported, like Tchoumi and al reported case's in cameroun where the patient survived until the 7th month of life without any surgery.10 We notice that in this case, the skin covering was intact and that there were no other associated malformations. In our case, the heart was neither covered with a serous membrane nor with a skin and the patient attempted the referral center by public transport vehicle.
Data from the literature reveal that the heart is completely uncovered in 41% of patients; covered with a serous membrane in 31% of patients and with a skin covering in 27% of cases.3,10
Definitive surgical management is possible.3,10 It requires technical platform not available in developping countries. In the literature, the survey of patients without extra cardiac malformations who attempts surgical correction is on average 5 years.
ConclusionEctopia cordis is a rare malformation. In developing countries, it is most often diagnosed at birth. The survival of affected patients depends on several factors. The necessary means to manage this affection remain limited in developing countries, making the prognosis almost always fatal.
Informed consentAuthors declare that the informed consent for publication was obtained from the patient's parents.
Conflict of interestNone.