Left or bilateral cardiac sympathetic denervation is employed as a final option for treating pharmacologically refractory ventricular arrhythmias of various etiologies. In this study, we share our experience with bilateral cardiac denervation. A total of 6 patients (mean age 73.8 years±6.5 years, mean LVEF 37±8.3%), between 2021 and 2022, with sarcoidosis or ischemic heart disease underwent bilateral cardiac denervation due to electrical storm despite prior treatments. It was achieved complete resolution of ventricular arrhythmias in 100% of cases, with no recurrence of cardiac device shocks and no mortalities, neither cases of pneumothorax, Horner's syndrome, or other complications. Therefore, it was concluded that in this study, bilateral cardiac denervation was effective for treatment of refractory ventricular arrhythmias. Further larger studies are required to confirm these findings.
La simpatectomía cardiaca izquierda o bilateral es usada como opción de última línea en el tratamiento de arritmias ventriculares refractarias de diferentes etiologías. En el siguiente texto, presentamos nuestra experiencia con la denervación cardiaca bilateral. En total, seis pacientes (edad promedio 73,8 ± 6,5, fracción de eyección del ventrículo izquierdo (FEVI) promedio 37 ± 8,3%) entre los años 2021 y 2022, con enfermedad cardiaca isquémica o sarcoidosis, fueron llevados a simpatectomía cardiaca bilateral por tormenta arrítmica que fue refractaria a otros tratamientos. Se consiguió una resolución completa de las arritmias ventriculares en 100% de los casos, sin recurrencias de descargas de los dispositivos cardiacos implantables y sin mortalidades reportadas. Tampoco se observaron situaciones de neumotórax, síndrome de Horner u otras complicaciones. Por lo anterior, pudimos concluir que, en este estudio, la simpatectomía cardiaca bilateral fue efectiva y segura para el tratamiento de las arritmias ventriculares refractarias. Se requieren estudios más grandes y comparativos para confirmar los hallazgos.
More than 100 years ago, Romanian oncologic surgeon Thomas Jonnesco performed the first left cardiac denervation in 1916, but he only published the case report in 1921.1 The first bilateral cardiac sympathetic denervation was performed in 1962, resulting in prolonged QRS normalization.2
The sympathetic postganglionic fibers of the superior thoracic ganglia innervate the heart and play an important role in maintaining arrhythmias.2 Other therapeutic options for blocking the heart's sympathetic signaling, such as stellate ganglion block and thoracic epidural anesthesia, have limited effects due to the short half-life of local anesthetics.2
Nowadays, left or bilateral cardiac sympathetic denervation is used for various types of ventricular arrhythmias of different etiologies, including channelopathies, long QT syndrome, polymorphic ventricular tachycardia, and many structural heart diseases like chagasic, sarcoidosis, hypertensive, and ischemic heart disease.1
In this paper, we present our case series of bilateral cardiac sympathetic denervation and discuss the important aspects to consider for the procedure's efficacy and complications.
Methods and resultsWe present a case series of bilateral cardiac sympathetic denervation procedures performed in our hospital between 2021 and 2022.
In each case, we used a two-port thoracoscopic approach (VATS) without selective intubation. We located a 5mm axillary port and another 5mm peri areolar port. We performed a bilateral T2–T4 sympathectomy by cutting the Kuntz nerves and preserving the stellate ganglion by making the proximal cut with scissors, thus avoiding diathermy injury. At the end of the procedure, we evacuated the pneumothorax with a Nelaton catheter, and none of the patients required a tube thoracostomy.
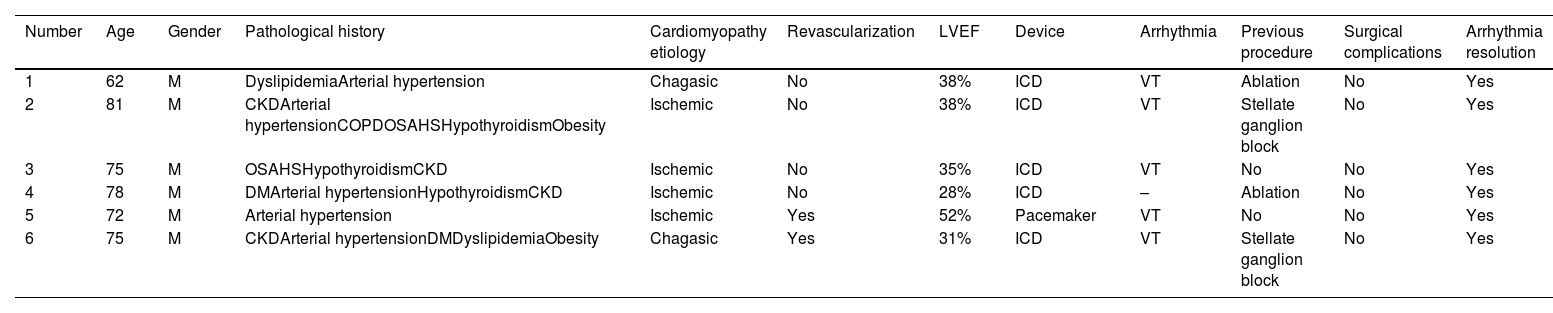
In Table 1, we show the epidemiological patient characteristics, previous failure procedures, and outcomes. We enrolled six patients aged 73.8 years (±6.5 years), all of them men, with sarcoidosis or ischemic heart disease. They presented ventricular arrhythmias with an electrical storm. Their left ventricular ejection fraction was 37% (±8.3%). Two of them had previously failed catheter ablation, and the other two patients had a previous Stellate ganglion block. All of the patients resolved the electrical storm during hospitalization in the postoperative period, and they did not present electrical shocks from their devices during follow-up.
Patient's preoperative characteristics and postoperative outcomes.
| Number | Age | Gender | Pathological history | Cardiomyopathy etiology | Revascularization | LVEF | Device | Arrhythmia | Previous procedure | Surgical complications | Arrhythmia resolution |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 62 | M | DyslipidemiaArterial hypertension | Chagasic | No | 38% | ICD | VT | Ablation | No | Yes |
| 2 | 81 | M | CKDArterial hypertensionCOPDOSAHSHypothyroidismObesity | Ischemic | No | 38% | ICD | VT | Stellate ganglion block | No | Yes |
| 3 | 75 | M | OSAHSHypothyroidismCKD | Ischemic | No | 35% | ICD | VT | No | No | Yes |
| 4 | 78 | M | DMArterial hypertensionHypothyroidismCKD | Ischemic | No | 28% | ICD | – | Ablation | No | Yes |
| 5 | 72 | M | Arterial hypertension | Ischemic | Yes | 52% | Pacemaker | VT | No | No | Yes |
| 6 | 75 | M | CKDArterial hypertensionDMDyslipidemiaObesity | Chagasic | Yes | 31% | ICD | VT | Stellate ganglion block | No | Yes |
CKD: chronic kidney disease; DM: diabetes mellitus; OSAHS: obstructive sleep apnea–hypopnea syndrome; ICD: implantable cardiac device; VT: ventricular tachycardia.
We did not observe any acute complications such as pneumothorax, hemothorax, or vascular lesions. Additionally, none of the patients presented chronic complications such as sweating pattern changes, Horner syndrome, or hyperalgesia.
DiscussionTraditionally, cardiac denervation has been used as a last resort for the treatment of pharmacologically refractory ventricular arrhythmias and after failing other procedures such as catheter cardiac ablation, stellate ganglion block, and thoracic epidural anesthesia. However, in our experience, cardiac sympathetic denervation was a safe and effective procedure with no complications, little morbidity, no mortalities, and a 100% efficacy rate for complete arrhythmia resolution, without cardiac device shocks recurrence or arrhythmic episodes detected and without reported complications. This could be explained by the surgical technique used, performing the procedure bilaterally, preserving the stellate ganglion, evacuating the residual pneumothorax at the end of the procedure without the use of thoracostomies. Nevertheless, contradictory results can be found in the literature.
Murtaza et al. published a meta-analysis in which they reported a pooled non-recurrence rate of ventricular tachycardias after Cardiac Sympathetic Denervation of all causes of arrhythmias to be 60%, although with high heterogeneity (I2=43%).3 Additionally, Shah et al.4 and Chihara et al.,5 in their systematic reviews, reported complete arrhythmia resolution rates of 53–100%4 and 52.4%,5 respectively.
This significant variability in the success outcomes of the procedure may be attributed to the inclusion of patients who underwent only left sympathectomy, as in the case series of König et al.,6 Cai et al.,7 and Prabhu et al.,8 which reported a complete resolution of arrhythmias of 38%, 42%, and 22%, respectively. In comparison, series such as Okada et al.,9 Téllez et al.,10 or even our own experience, demonstrated success rates of 80%, 92%, and 100%, respectively, by including only bilateral cardiac denervation.
However, it is important to highlight that in other series where only bilateral denervation were included, such as in the study by Lee et al.,11 recurrence rates as low as 46% were reported, which raises questions. Additionally, in the systematic review by Chihara et al.,5 they report complete resolution of arrhythmias defined as the absence of cardiac device discharges after denervation, with rates of 66.5% and 65% with or without stellate ganglion preservation, compared to 63.8% with left denervation alone.
According to Vaseghi et al.,12 patients with bilateral Cardiac Sympathetic Denervation experienced longer sustained VT (ventricular tachycardia) or implantable cardioverter-defibrillator (ICD) shock-free and orthotopic heart transplantation (OHT)-free survival in comparison to those with left CSD alone. However, left CSD was not identified as an independent factor associated with the recurrence of ICD shocks.
When analysis was restricted to only arrhythmias caused by conditions other than Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT) and Long QT Syndrome (LQTS), the pooled VT non-recurrence rate was 50% (range 41–58%, I2=5%).12
Additionally, Vaseghi et al.12 described poor prognostic factors for complete arrhythmia resolution after cardiac denervation, including a worse NYHA classification, use of more than one antiarrhythmic drug, and a ventricular tachycardia cycle lasting more than 400ms. On the other hand, patients with a history of bilateral cardiac sympathetic denervation had more free-shock time and transplant-free survival compared to only left cardiac sympathetic denervation (p=0.014), highlighting the importance of bilateral denervation.12
In view of all the previously mentioned aspects, the importance of comparative studies is highlighted in order to determine the superiority of bilateral denervation over left denervation alone.
Regarding surgical complications, the most commonly reported one was pneumothorax in 5%4 and 5.5%5 of cases, even without reporting any events as in our series, omitting the use of thoracostomies. The majority of cases did not necessitate further treatment.
Horner's syndrome was reported in 3%4 and 4.3%5 of cases, which resolved spontaneously in most instances. The latter complication could be avoided by preserving the stellate ganglion, without compromising the surgery's effectiveness. Other more severe complications, such as hemothorax, vascular injuries, and brachial plexus injuries, occurred in less than 1% of cases each, establishing it as a safe procedure.
ConclusionsCardiac sympathectomy is a safe procedure, with mostly self-resolving minor complications and variable effectiveness for complete arrhythmia resolution. Comparative studies are needed to assess the necessity of bilateral procedures or to identify poor prognostic factors. Additionally, comparative studies with other procedures, such as catheter ablation, need to be conducted before considering sympathectomy as a first-line treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Ethical considerationsAs a descriptive and retrospective study in which only medical records were reviewed and the identity and patients’ data will be protected, it is considered a non-risk research, therefore informed consents are not required.
Data availability statementThe articles that support the findings of this literature systematic review are available in the databases (PubMed, Embase, and Scopus) and can be accessed through a license. Regarding the patients’ clinical histories in the case series, to acquire additional information or their respective verification, please contact the correspondence author.
FundingNone.
Conflict of interestNone.