Tricuspid regurgitation in patients with mitral valve disease is associated with poor outcome and predicts poor survival, heart failure, and reduced functional capacity. The objective was to access if modified De Vega Annuloplasty (mDA) using pericardial patch offered significant surgical, functional and economical benefits over RA done for Mitral valve replacement with severe functional tricuspid regurgitation in a predominant rheumatic population.
MethodsThis retrospective study analyzed data from 50 patient who were eligible for this study and underwent mitral valve replacement surgery for severe mitral valve stenosis with functional tricuspid valve disease (30 AR and 20 mDA) between the period of January 2015 and December 2019 at Kem Hospital, Mumbai. Post-operatively all patients has routine TTE (transthoracic echocardiography) before discharge and subsequently at 6 months and 1 year. Severity of TR (Tricuspid Regurgitation), LVEF (Left Ventricular Ejection Fraction), TAPSE (Tricuspid Annular Plane Systolic Excursion) and PASP (Pulmonary Artery Systolic Pressure) were used for determining functional status of the patient.
ResultsThere was no statistically significant difference in residual TR. There was significant improvement in NYHA (Newyork Heart Association) stage. Statistically significant difference was seen in the cost, with mDA demonstrating economic benefits for the patient.
ConclusionsSimilar functional outcomes were seen with both techniques. Only incremental economic benefit was seen with mDA in the form of lower cost for the patient. However, this is just the early outcome and long term study is ongoing to ascertain outcome.
La regurgitación tricuspídea en pacientes con valvulopatía mitral se asocia a un mal resultado y predice una mala supervivencia, insuficiencia cardíaca y una menor capacidad funcional. El objetivo fue acceder a si la anuloplastia de De Vega modificada (mDA) mediante parche pericárdico ofrecía beneficios quirúrgicos, funcionales y económicos significativos sobre la RA realizada para la sustitución de la válvula mitral con regurgitación tricúspide funcional grave en una población predominantemente reumática.
MétodosEste estudio retrospectivo analizó datos de 50 pacientes que fueron elegibles para este estudio y se sometieron a cirugía de reemplazo de válvula mitral por estenosis severa de válvula mitral con enfermedad de válvula tricúspide funcional (30 AR y 20 mDA) entre el período comprendido entre enero del 2015 y diciembre del 2019 en el Hospital Kem, Bombay. Después de la operación, todos los pacientes tienen ETT (ecocardiografía transtorácica) de rutina antes del alta y posteriormente a los 6 meses y a un año. La gravedad de la TR (regurgitación tricuspídea), FEVI (fracción de eyección del ventrículo izquierdo), TAPSE(excursión sistólica del plano anular tricúspide y PASP (presión sistólica de la arteria pulmonar) se utilizaron para determinar el estado funcional del paciente.
ResultadosNo hubo diferencia estadísticamente significativa en la TR residual. Hubo una mejora significativa en el estadio de la NYHA (New York Heart Association). Se observó una diferencia estadísticamente significativa en el costo, demostrando la mDA beneficios económicos para el paciente.
ConclusionesSe observaron resultados funcionales similares con ambas técnicas. Sólo se observó un beneficio económico incremental con la mDA en forma de menor coste para el paciente. Sin embargo, este es solo el resultado inicial y se está llevando a cabo un estudio a largo plazo para determinar los resultados.
Left sided heart disease, particularly rheumatic mitral valve (MV) disease, is frequently associated with functional tricuspid regurgitation (TR). Tricuspid valve (TV) leaflets are morphologically normal in majority of the cases but do not coapt properly because of either distortion of leaflets, chords and papillary muscles resulting from dilation of the right ventricle (RV) and TV annulus.
Even after successful surgical correction of left-sided valvular lesions significant TR often does not regress and can also progress.1 Poor outcome and functional status are associated with uncorrected TR.2 Without treatment, TR may worsen over time leading to worsening of symptoms, quality of life, heart failure and even death.
Prior studies indicate an incidence of 7–16% for development of late, moderate to severe TR after MV operations.3 Consequently surgical correction of severe TR at the time of MV repair or replacement is recommended for the management of patients with valvular heart disease by the American College of Cardiology/American Heart Association Guidelines.3
Multitudes of techniques are available for tricuspid valve repair with both Ring Annuloplasty and Suture Annuloplasty having their fair share of proponents and critics. In the absence of a consensus favoring a single method and continued research for an ideal technique, the current choice regarding which technique to use for addressal of functional TV regurgitation can be a difficult one and is institution based.
Here is our institutional retrospective, cohort based, comparative study based on the technique we use i.e. Ring Annuloplasty (RA) as well modified De Vega Annuloplasty (mDA) using pericardial patch. This study was undertaken to compare the outcome of two different surgical techniques and their early outcome in terms of functional outcome.
Patient and methodWe performed a retrospective cohort study of 50 consecutive rheumatic patients who underwent mitral valve replacement for severe mitral stenosis with severe functional TR who presented in the period between January 2015 to December 2019 in KEM Hospital, Mumbai for mitral valve surgery. Retrospective data analysis was done and review of the records of all 50 patients which included clinical histories and complain, preoperative transthoracic echocardiogram, operative techniques and follow up transthoracic echocardiography on discharge and consequently at 6month and 1 year were done as per institutional protocol. We divided patients into two cohorts: Cohort A (n=30) Ring Annuloplasty (RA) patient and Cohort B (n=20) modified De Vega Annuloplasty (MdA) using pericardial pledget with interrupted suture.
We excluded ischemic heart disease patient requiring concomitant surgery for same, severe mitral valve regurgitation, organic TV disease, infective endocarditis, left atrium clot, chronic kidney disease, large left atrium (>6cm), emergency surgery and patients with associated congenital anomalies from our study. We also excluded patient lost follow-up within 1 yr of surgery.
Ethical considerationInformed consent of the patients have been taken before publishing the data.
Preoperative dataIn Cohort A 15 patients had NYHA grade II dyspnea, 10 Patients had NYHA grade III dyspnea and 5 patients had NYHA grade IV dyspnea. In Cohort B 10 patient had NYHA grade II dyspnea and 8 patients had dyspnea NYHA grade III while 2 patients presented with NYHA grade IV. Other clinical parameter included in Table 1. There was no statistically significant difference between both groups in clinical data. There was no significant difference in both groups regarding left ventricular end-systolic diameter (LVESD), left ventricular end-diastolic diameter (LVEDD), ejection fraction (EF), pulmonary artery systolic pressure (PASP), and tricuspid annular plane systolic excursion (TAPSE) as seen in Table 2.
The preoperative clinical characteristics and echocardiographic data.
| Cohort A (n=30) | Cohort B (n=20) | p value | |
|---|---|---|---|
| Age | 38.00+8.14 | 38.15+6.68 | 0.9457 |
| Sex (female) | 15+2.83 | 10+2.83 | 0.2191 |
| LVESD | 3.89+0.407 | 3.945+0.456 | 0.6565 |
| LVEDD | 4.05+0.253 | 4.075+0.249 | 0.7673 |
| Ejection fraction | 59.17+2.65 | 58.50+3.28 | 0.4328 |
| PASP | 58.16±14.44 | 63.2+18.19 | 0.339 |
| TAPSE | 14.50+2.22 | 14.80+2.21 | 0.6419 |
All patients had the operation performed through a median sternotomy, cardiopulmonary bypass, and antegrade cold delNido cardioplegia with systemic cooling. Mitral valve replacement was performed in all patients. After completion of left-sided valve surgery, both vena cavae were snared, and the right atrium was opened to repair the tricuspid valve on the arrested heart. Severity of functional tricuspid regurgitation was checked using trans-esophegeal echocardiography, syringe saline test and by inserting finger.
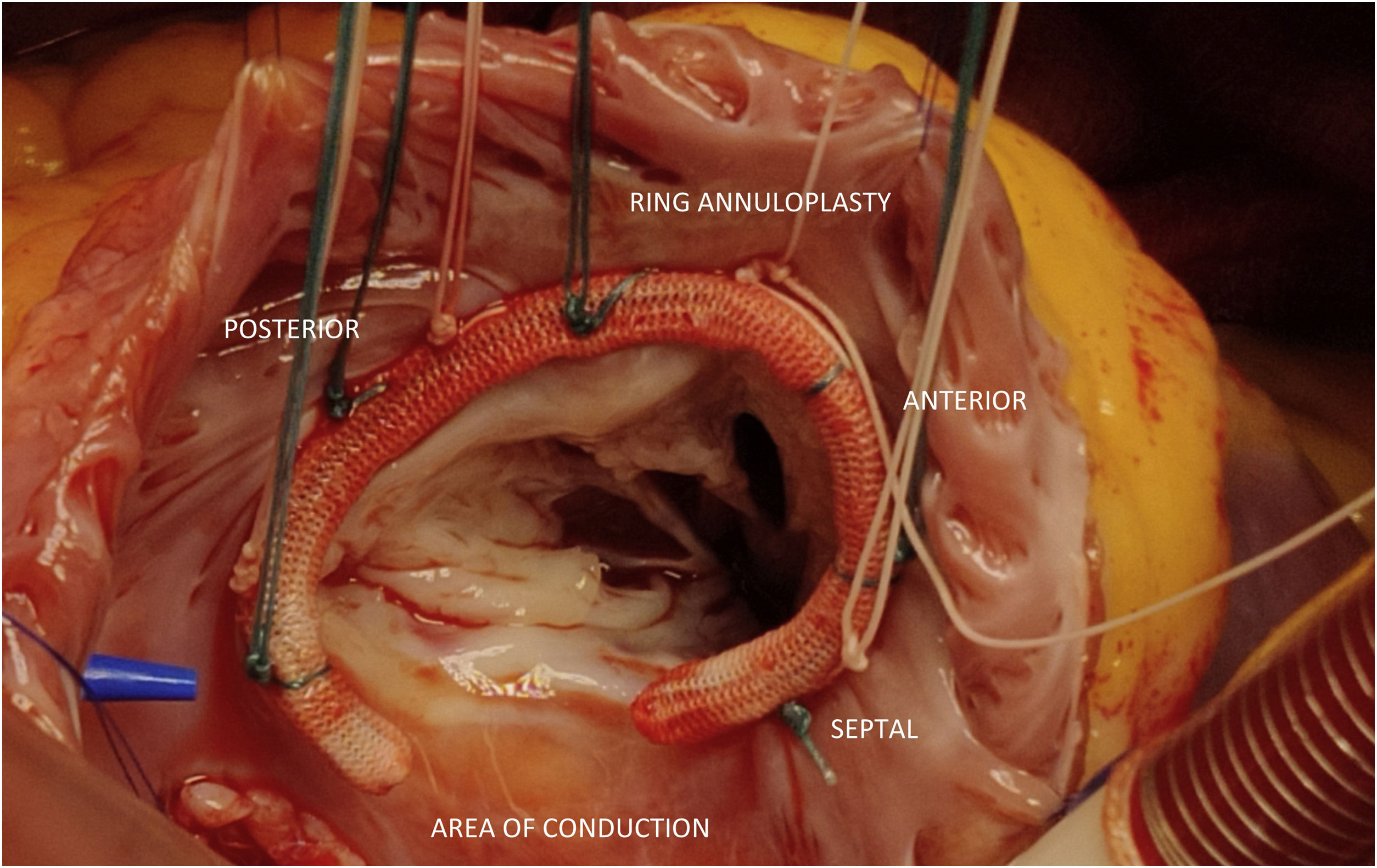
Ring annuloplasty: In the Ring Annuloplasty cohort, we used Contour 3D Annuloplasty rings (Medtronic, California, USA) (Fig. 1). U shaped 2–0 (26) braided polyester stitches were applied to the annulus from the anteroseptal commissure to the posteroseptal commissure with 3 sutures in anterior leaflet annulus, 2 in septal leaflet annulus and 5–6 in posterior leaflet annulus. The size of the ring was determined by the length of the septal leaflet. Stitches were applied to the ring and tied.
Modified De Vega's technique using pericardial patch: After assessing the severity of functional tricuspid annulus, we start suturing from anteroseptal to posteroseptal commisure using U shaped 2–0 (26) braided polyester stitches in interrupted manner using pericardium strip in whole as a pledget which were applied at annulus about 2 at anterior leaflet annulus and 3–5 on posterior leaflet annulus depending upon the severity (Fig. 2). The degree of narrowing of the annulus was controlled by inserting the back of LA retractor, prosthetic valve gauge and by inserting two finger (index and ring) as free passage through the annulus as rough measurement for size of annulus after the repair to avoid over correction. Sutures were then tied.
The intraoperative test was done by syringe saline test and by transesophageal echocardiography after coming off by-pass. The repair was desirable.
Statistical analysisSPSS version 20 (Statistical Package for Social Science, IBM Corp, Chicago, IL, USA) was used for data entry and analysis. Data were presented as mean and standard deviation. Fisher Exact test were used to compare qualitative variables. Independent samples t-test test was used to compare two quantitative variables in both groups. Unpaired samples t-test was done to compare preoperative and postoperative quantitative variables in the same group. p-value was considered statistically significant when <0.05.
ResultsAs seen from Table 3 there is no statistical difference between CPB time and cross clamp time. Also, the immediate postoperative were identical in both cohorts with no statistically significant difference of ICU and hospital stay.
Perioperative outcomes.
| Cohort A (n=30) | Cohort B (n=20) | p value | |
|---|---|---|---|
| CPB time | 185.59+30.70 | 176.85+38.56 | 0.328 |
| Cross clamp time | 152.13+32.60 | 145.20+30.28 | 0.251 |
| Postoperative CVP | 8.73+2.02 | 8.20+2.04 | 0.3664 |
| Days of Support: Milrinone | 2.17+0.75 | 2.20+0.62 | 0.8692 |
| Adrenaline – | 1.60+0.89 | 1.75+1.33 | 0.6355 |
| reexploration | 0.17+0.38 | 0.15+0.37 | 0.8780 |
| ICU stay | 2.18+0.60 | 2.16+0.60 | 0.765 |
| Hospital stay | 7.70+1.21 | 7.40+0.90 | 0.3616 |
| Mortality | 0.17+0.38 | 0.15+0.37 | 0.8780 |
The patient in both cohort required Inj. Milrinone for almost 2–3 days.
There were total of 5 mortality in Cohort A and 3 in Cohort B out of which 2 patient in Cohort A died after reexploration and 11 patients in Cohort B died after reexploaration.
Improvement in NYHA classificationIn Cohort A, all 5 patients improved from NYHA class IV to class II/III in immediate postoperative period and at 6 month 3 patient had improved to NYHA class I/II. Out of 10 patient 7 patient improved from NYHA class III to class I/II in immediate postoperative period and 2 patient at 6month. Out of 15 patients in NYHA class II 8 patient showed immediate postoperative improvement while around 4 showed improved over period of 6month and 2 over a period of 1 year. There was significant improvement in NYHA status (p=0.000067) after ring annuloplasty.
In Cohort B, 2 patient improved from NYHA class IV to class III in immediate postoperative period and 1 patient to class I/II by 1year. Out of 8 patients from NYHA class III, 4 patients returned to class I/II in immediate postoperative period and 2 patient in span of 6 month while one in span of 1 year. Out of 10 patients in class II, 6 patients showed sudden improvement in immediate postoperative period, 3 in span of 6 month and 1 patient showed significant improvement over a period of 1 year. There was also significant improvement in NYHA status (p=0.000074) after De Vega repair. There was no prosthesis/valve related mortality in the follow-up period.
Predischarge echocardiographic dataWell-functioning prosthetic mitral valve was seen in all patients in the pre discharge Echocardiography. Both TAPSE (p=0.902) and PASP (p=0.473) show no statistical difference, as shown in Table 4.
Echocardiographic data after six months and 1 yearWell functioning prosthetic valves were seen in all patients of both Cohorts after six months. No statistical significant difference was seen in residual tricuspid regurgitation between both Cohorts as shown in Table 5. Both Cohorts demonstrated significant improvement in the Right ventricular function as seen by improved TAPSE in the early postoperative period and after six months (p<0.005) as well as 1 year as shown in Table 6. There was a statistically significant difference in pre-operative, early postoperative and follow up 6 month TAPSE (Fig. 3). PASP improved after six months in both Cohorts (Fig. 4). No patient had severe TR 1 year after the surgery.
Indications and choice of optimal surgical technique pose challenges for tricuspid valve repair for functional TR. Patients with severe TR, moderate TR with either tricuspid annular dilatation (greater than 4cm) or Tricuspid index greater than 21mm/m2 are indicated to be intervened in as per AHA/ACC guidelines 2020 update.4 Conservative treatment, repair or replacements are included in the plethora of management options. The ideal repair technique is elusive and continues to evolve with the ongoing research with the ultimate fact being that optimal anatomic and physiologic correction influences long term results of the repair.
The effect of each repair on right ventricular function and remodeling, which may have an impact on long-term survival has been also studied previously. However in our study, we examined the effect of each repair technique on TAPSE and PASP. Also, our study is related to early outcome of repair.
Our study shows no statistical difference in using ring Annuloplasty or modified De Vega's technique on degree of TR (p=0.253).
Preoperative tethering of tricuspid valve leaflets and postoperative left ventricular dysfunction predict mid-term outcome of tricuspid repair as they are associated with recurrence of TR early after the procedure regardless of the type of Annuloplasty. Increased right ventricular pressure is an additional adverse prognostic factor as it also results in worse TR during mid- term follow-up. However, the authors did not report on the difference between the types of Annuloplasty as regards to better or worse outcome.5 In our study we repaired functional TR in patients with moderate-to- severe or severe TR. This is consistent with most of the authors elsewhere.
Our study shows that in immediate postoperative period PASP did not change much but after 6 month there is significant statistical difference seen (p=0.009).
Similar to our study Wang and colleagues6 found no significant difference in NYHA class between the two techniques in patients who underwent surgery for secondary TR. But Matsuyama and colleagues7 demonstrated a significant difference in TR recurrence between the two Cohort in long term as per (p=0.027).
Critiques of De Vega annuloplasty label it as being unpredictable and unreliable, most likely due to “Guitar String Syndrome” which is consequent to the long suture line, which breaks or slides through the tissue as the annulus dilates. To overcome this shortcoming and decrease the perioperative complication we have used pericardial strip as a pledget to reinforce the suture and the long term result were similar to that of ring annuloplasty, also the pericardial strip does not develop any retraction or degeneration in long term.8
We found no statistically significant difference between modified DeVega and ring repair in the early postoperative period which is supported by prior studies done by Khallaf et al.9 and Dokhan et al.10 thus reinforcing our findings.
There were no differences in survival and freedom from major cardiac/cerebrovascular adverse event between the two Cohorts. Also the results mentioned can be attributed to meticulous surgical technique in both Cohorts and optimal post operative ICU management and follow-up.
There was incremental economic benefit seen in patient with modified De Vega's technique using pericardial pledget even though not statistically significant i.e. because with ring annuloplasty patient has to pay cost for ring i.e. around 30–35 thousand Indian rupee (for a patient without any government scheme or health insurance) whereas for modified De Vega using pericardial patch they do not need to pay anything extra.
The limitation of our study include its retrospective nature, small sample size in single center study and no long term follow up. Moreover we did not record and analyze RV diameter because this data was not routinely recorded in our hospital. Also the method of repair was chosen by operating surgeon.
The study evaluated the two repair techniques in patients with rheumatic heart disease with severe functional tricuspid regurgitation in which no ideal technique has been found yet.
ConclusionIn the absence of a consensus favoring a single method and continued research for an ideal technique, the current choice regarding which technique to use for addressal of functional TV regurgitation can be a difficult one and can be institution based. Our study shows that with modified De Vega repair using pericardial patch has remarkable clinical utility in cases of functional tricuspid regurgitation. Our study shows comparable prognosis with both the techniques of TV repair, that is, prosthetic ring annuloplasty and modified DeVega repair, when done for functionally significant TR in a pre-dominantly rheumatic population. But a larger sample size and long term follow up is still needed for better confirmation of early promising results.
Ethical considerationInformed and written consent of all the patient and relevant department have been taken before publishing the data.
FundingNo funding used.
Conflict of interestNone/