Papillary fibroelastoma is a benign cardiac tumor generally found on valve surfaces, although involvement of a cardiac chamber endocardium has been rarely reported. They are usually asymptomatic, but embolic events are highly associated presenting with neurological clinic. We present a case of a patient with recurrent stroke presenting with aphasia, right hemiparesis and left oculocephalic deviation, in which a mobile mass was observed in the transesophageal echocardiography at the ligament of Marshall, being a very unusual location for the tumor. Surgical resection was performed uneventfully and histopathological examination confirmed the diagnosis.
El fibroelastoma papilar es un tumor cardiaco benigno que se encuentra generalmente en la superficie valvular, siendo muy infrecuente la afectación del endocardio de las cámaras cardiacas. Suelen ser asintomáticos, aunque eventos embólicos están muy asociados manifestándose con clínica neurológica importante. Presentamos el caso de una paciente con ictus embólico recurrente que presenta afasia, hemiparesia derecha y desviación oculocefálica izquierda, en la que se observó en el ecocardiograma transesofágico una masa móvil a nivel del ligamento de Marshall, una localización muy infrecuente del tumor. Se realizó resección quirúrgica completa y sin incidencias, obteniendo posteriormente el diagnóstico histopatológico de fibroelastoma papilar.
Cardiac papillary fibroelastoma (PFE) is a benign primary cardiac tumor with significant propensity for embolization. Current reports indicate its increasing incidence, being considered the most frequent benign cardiac tumor in adults, probably due to the advent of transesophageal echocardiography (TEE).1,2 Approximately 84% of PFEs arise from valve surface, especially in the aortic valve. Non-valvular PFEs are very unusual, and the location in the left atrium is exceedingly rare (1.6–2%).2,3 To our knowledge, there are only two cases reported to arise at the level of the ligament of Marshall.4
Although most cases are asymptomatic and diagnosed incidentally, symptomatic patients can present complications related to thromboembolic events, more frequently transient ischemic attack and ischemic stroke, which can be recurrent.1,4 Diagnosis is suspected during echocardiography, but needs to be confirmed by histopathological examination. A transesophageal echocardiogram is usually required, due to its small size. The only available curative treatment, is complete surgical excision of the tumor.1,4
We present a case of a patient with recurrent ischemic stroke that presents with aphasia, right hemiparesis and left oculocephalic deviation, in which a mobile mass was observed at the level of the ligament of Marshall, being an extremely rare location for this tumor. Surgical resection was performed uneventfully and histopathologic examination confirmed the diagnosis of PFE.
Case reportA 59-year-old woman arrived at the emergency department with acute onset of aphasia, right hemiparesis and left oculocephalic. Her medical history included smoking, dyslipidemia and an ischemic stroke 4 month prior to admission with complete functional recovery, in which an electrocardiogram (EKG), transthoracic echocardiography (TTE) and a twenty-four-hour EKG Holter monitoring were performed, without encountering the embolic source of the stroke. No usual risk factors for stroke were present, such as hypertension, diabetes or thrombophilia.
She had no symptoms of cardiac illness, and the clinical cardiovascular examination was unremarkable. An EKG showed normal sinus rhythm and a right-bundle branch block not reported previously. Chest radiography and laboratory results were within normal limits. A cerebral computed tomography angiogram demonstrated ischemic lesions on the left middle cerebral artery territory and an emergent endovascular reperfusion was performed by thrombectomy without complications. Neurologic evolution was favorable, persisting mixed aphasia. A TTE was performed showing only thickening of the free edge of the aortic valve veils generating mild aortic insufficiency, but no cardiac mass was observed.
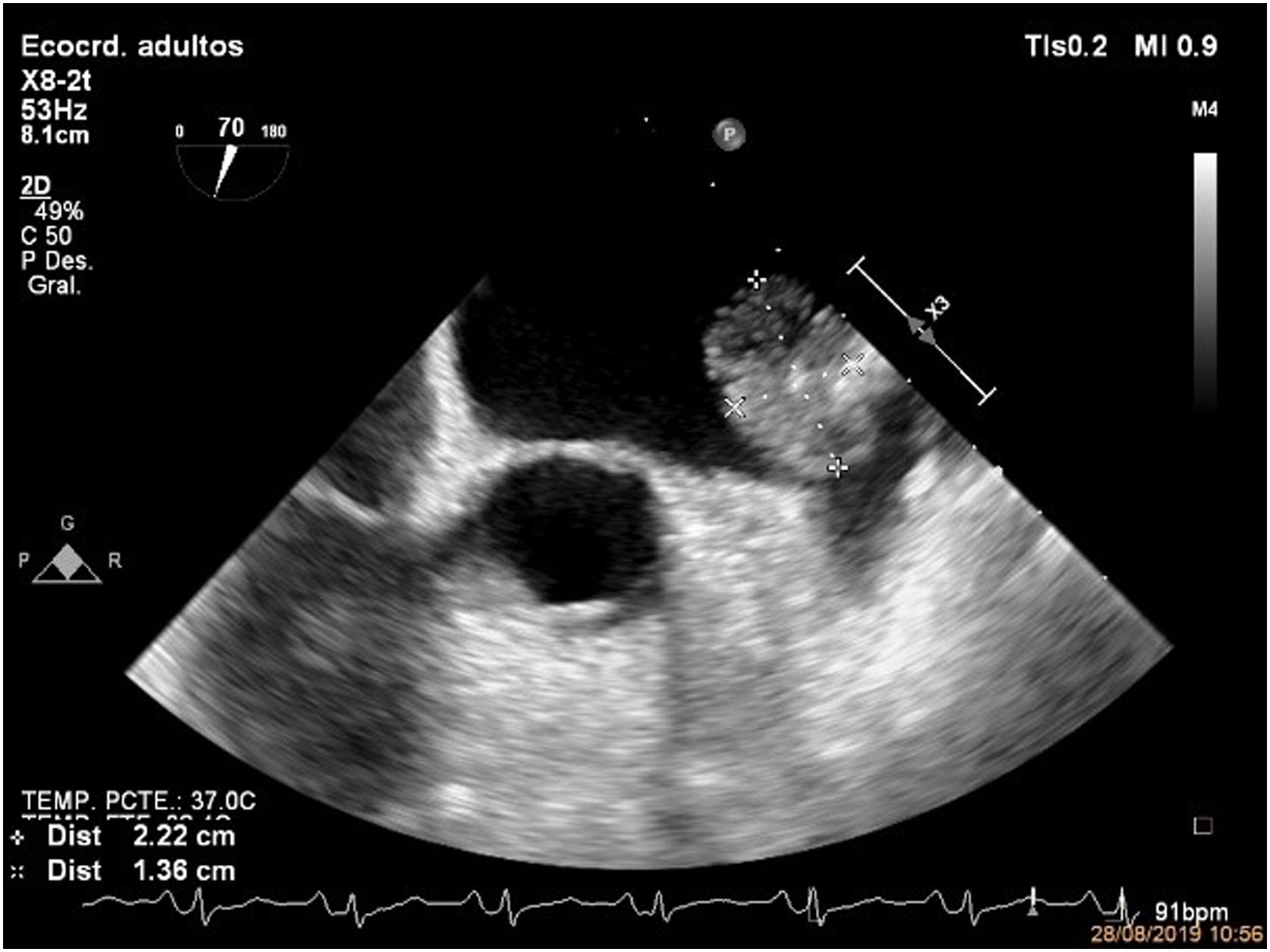
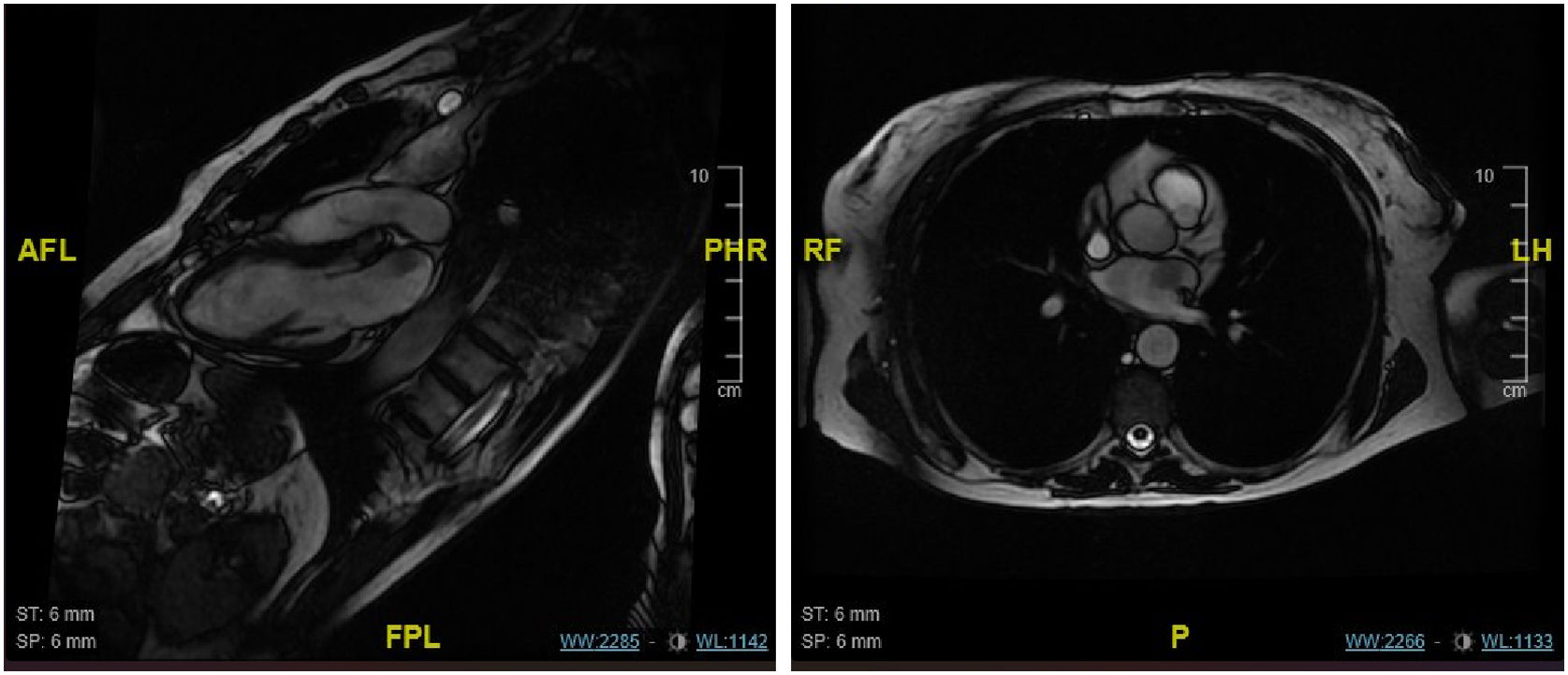
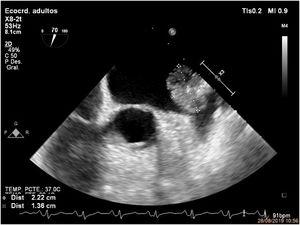
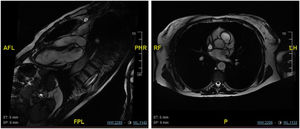
Five days after admission and without new symptoms, a control cerebral computed tomography revealed a new established ischemic lesion in the left parahippocampal gyrus and hemorrhagic transformation in the left frontal operculum. Due to high suspicion of cardiac source of emboli, a transesophageal echocardiography (TEE) was performed revealing a mobile, echogenic, 20mm×15mm pedunculated mass adhered to the ligament of Marshall (Fig. 1). An MRI was also performed for better characterization of the mass (Fig. 2).
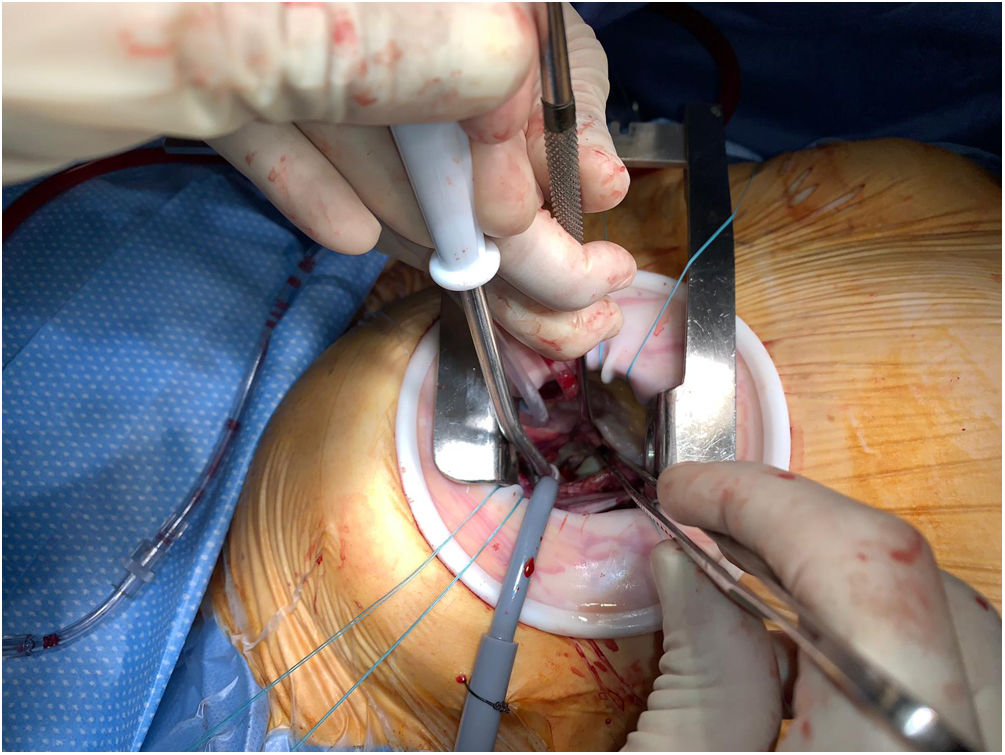
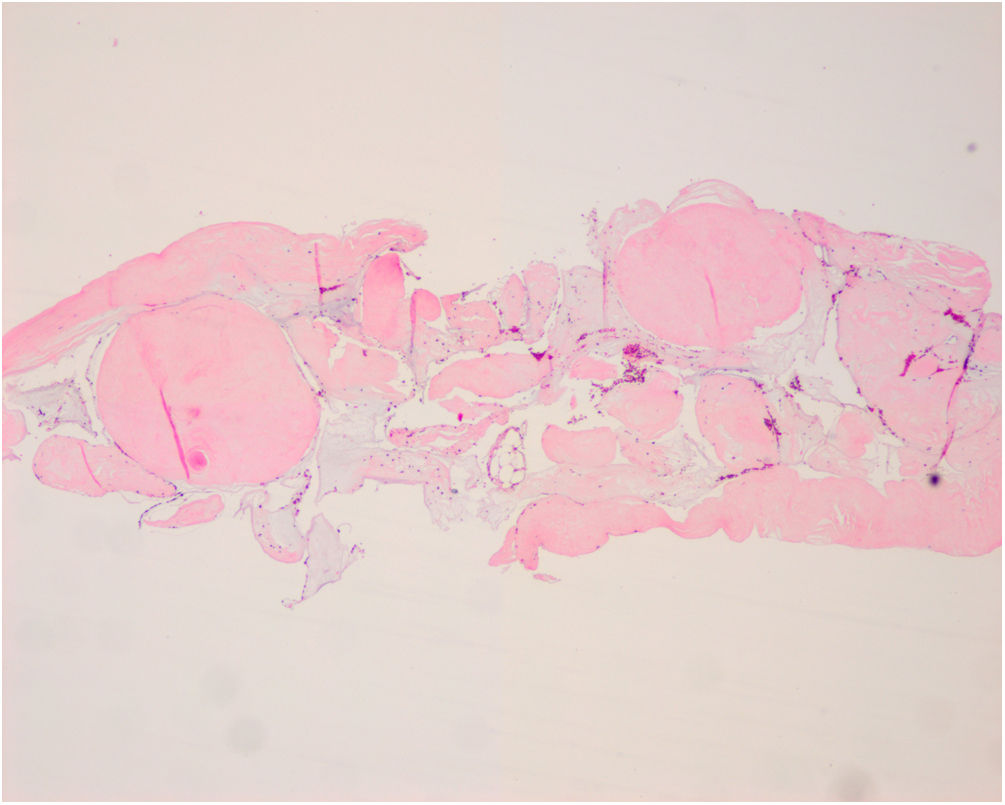
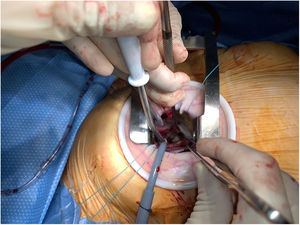
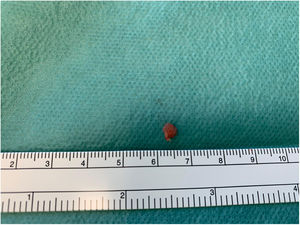
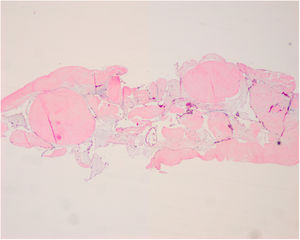
The patient underwent complete surgical excision of the mass through minimally invasive approach (right anterior thoracotomy), with cardiopulmonary bypass (Fig. 3). Complete resection was confirmed by intraoperative TEE. Posterior histopathologic examination confirmed the diagnosis of PFE (Figs. 4 and 5).
Histopathologic study of the mass corresponding to papillary fibroelastoma. Multiple avascular branching papillary fronds covered by a single layer of endothelial cells with acellular fibrous and myxoid stroma. Focally, muscle tissue was observed and also foci of dystrophic calcification (hematoxylin and eosin staining).
Postoperative course was uneventful with progressive neurological improvement, persisting very mild dysphasia as a sequela. There was no evidence of residual mass on the TTE performed 1 week after the intervention, being discharged five days after surgery.
DiscussionPrimary cardiac tumors are very rare, with an incidence ranging from 0.0017% to 0.28%.1,4 Myxomas were traditionally thought to be the most common, nevertheless most of the supporting data was derived from autopsy series, reflecting a probable underdiagnosis.2,4 Recent studies report the PFE as the most frequent primary cardiac tumor in adults.1,2 In a study that was made in a reference center by Tamin et al., the frequency of PFE in patients undergoing TTE was greater than cardiac myxoma at a rate of approximately 2:1.1,2 The incidence is increasing probably due to higher quality of image with TEE, improvements in technology, enhanced awareness of PFE, and an aging population.1,2
PFEs have high thromboembolic rate due to either the tumor itself or from adherent thrombi localized within the fronds.1,2,4 Although most cases are asymptomatic and diagnosed incidentally, almost half of patients with symptomatic PFEs, presents as a transient ischemic attack or stroke (42–53%), which can be specifically recurrent.1,5 Tumor mobility has been reported as an independent risk factor for embolization.6 Thorough etiologic work-up after a stroke is crucial to identify the underlying cause. In a systematic review of international clinical practice guidelines in acute ischemic stroke7, the importance of the echocardiography is highlighted, especially when a cardiac source is suspected.
There are no current guidelines, protocols of conservative or surgical treatment, nor specific indication of anticoagulation therapy. Tamin et al.2 reported that patients without surgical intervention after diagnosis, presented an incidence of 8.9% for having recurrent stroke, with incremental risk over time.2,8 Sun et al.8 also observed high incidence (6%) on presenting a thromboembolic event after diagnosis of PFE. All of this data supports the indication for surgery in patients with suspected PFE, for an accurate diagnosis and to avoid embolism.
In almost a quarter of patients, the diagnosis is obtained by TEE, which was not observed by ETT.2 There are several studies describing the importance of cardiac imaging, including 3D TEE or cardiac magnetic resonance, for better characterization of the tumor, relationships with surrounding tissues, formulation of surgical approach, and for the differential diagnosis.3,5,9
The only curative treatment is complete surgical excision of the tumor, with high likelihood of valve preservation, especially if the patient is symptomatic and the tumor is on the left side of the heart.4 Surgery improves prognosis and reduces the risk of stroke substantially, especially when performing primary resection of the tumor (98%). Short- and long-term prognosis after surgical removal is excellent.4,10
ConclusionsCardiac tumors, like papillary fibroelastoma, should be considered as a differential diagnosis, even in unusual locations, after an ischemic stroke. PFE has significant risk for recurrent thromboembolic events and should be adequately diagnosed. The gold standard is the TEE, which should be performed because of its higher sensitivity. It is important to emphasize the extremely rare location of our patient's tumor. Complete surgical excision as soon as possible is the treatment of choice, because of the high risk of unpredictable embolization. Surgery reduces the risk of recurrent neurologic events and increases long-term postoperative prognosis.
Ethical considerationsThe patient gave her consent for clinical information relating to this case to be reported in a medical publication.
Conflict of interestThe authors declare they have no conflict of interest.