Minimally invasive aortic valve replacement (AVR) benefits avoiding sternal wound complications, prolonged hospitalization and reduced postoperative pain has been widely reported. The benefits of a small sternal incision in obese patients decreases the potential risk of sternal dehiscence otherwise present on a conventional sternotomy. Here we report the case of a 76-year-old woman with moderate obesity who was referred to our institution with severe degenerative aortic stenosis. She underwent aortic valve replacement with a novel technique for annulus enlargement through upper ministernotomy.
El reemplazo de la válvula aórtica mediante cirugía mini-invasiva ha demostrado disminuir las infecciones del sitio quirúrgico y reducir la estancia hospitalaria, así como el dolor postoperatorio. Estos beneficios se han demostrado aun en pacientes obesos. Reportamos el caso de una paciente de 76 años con obesidad que fue referida a nuestro centro con estenosis aórtica severa sintomática. Dicha paciente fue sometida mediante mini-esternotomía a reemplazo de la válvula con ampliación de anillo con una novedosa técnica (técnica de Yang).
AVR through mini-invasive approaches have been gaining acceptance by many surgeons around the world. Upper ministernotomy and right minithoracotomy are the most common techniques.1–3 Several studies have shown the benefits of this surgeries. Mini-approaches for AVR have been shown to reduce hospital stay, the use of blood components, have better esthetic acceptance and provide rapid recovery to the patient.4,5 Recently, a meta-analysis showed that AVR via upper ministernotomy may have lower mortality compared with minithoracotomy.6
Comorbidities such as morbid obesity increase postoperative complications in cardiac surgery (more mortality, infections, respiratory complications). Full sternotomy causes greater respiratory restriction in these patients, which increases the possibility of complications.7
We describe an AVR via upper ministernotomy in a 76-year-old woman with moderate obesity using the novel annulus enlargement technique first described by Yang.8
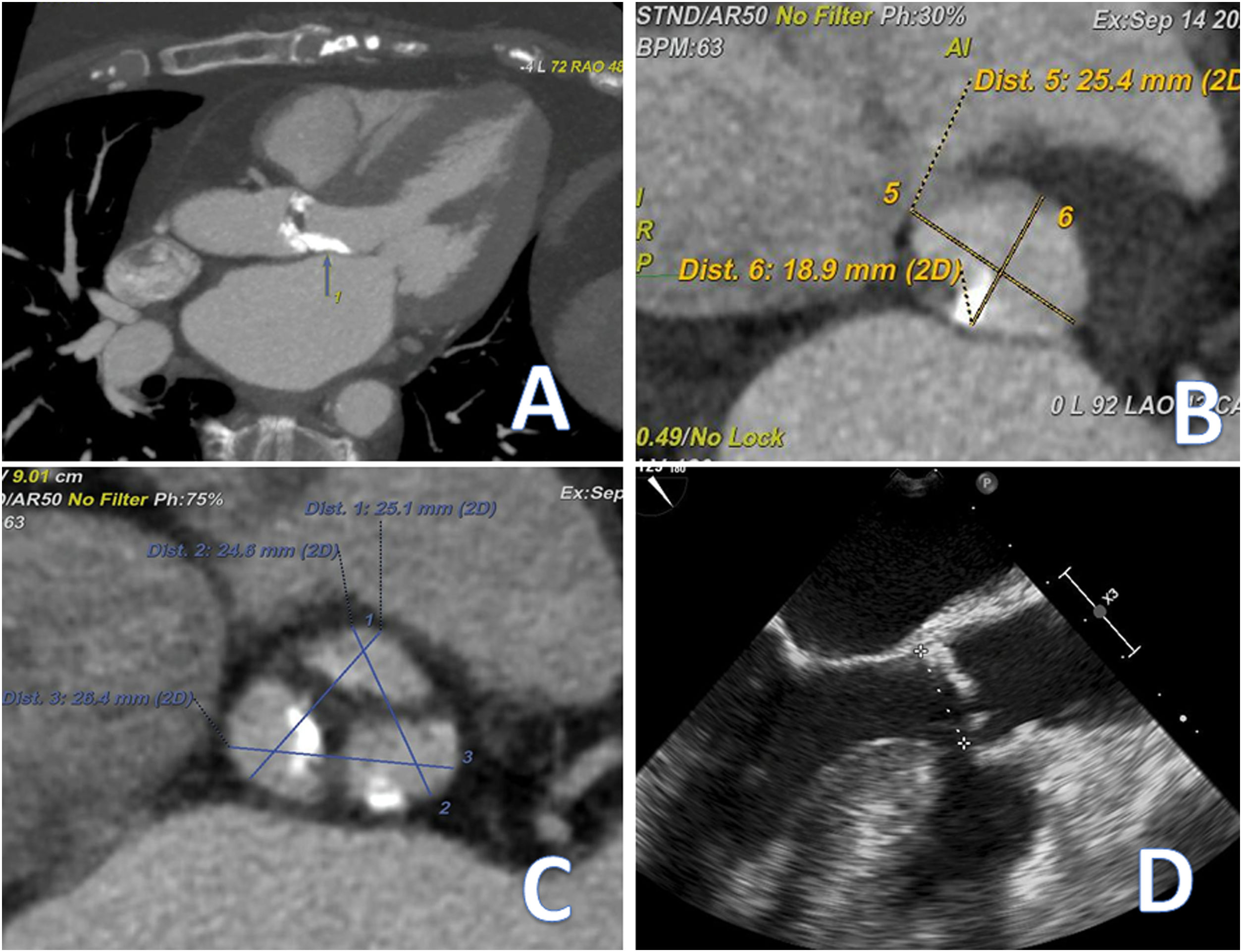
Case reportA 76-year-old woman with history of dyspnea, angina and syncope was referred to our institution for severe AV stenosis on transthoracic echocardiography. Her medical history was notable for hypertension, hyperlipidemia and obesity (weight: 80kg and height: 150cm; BMI: 35kg/m2). Diagnostic workup inside our Institution included a transthoracic echocardiography which demonstrated LVEF: 61%, peak gradient: 129mmHg, mean gradient: 81mmHg, AV area: 0.45cm2, indexed AV area: 0.25cm2/m2 and AV annulus: 18mm. Coronariography did not find coronary disease or abnormality and the right catheterization found postcapillary hypertension (pulmonary artery pressures: 48/15mmHg, mean: 27, wedge pressure: 25, pulmonary vascular resistance: 0.3 Woods). Contrast-enhanced CT and preoperative transesophageal echocardiography measured the AV annulus at 19mm (Fig. 1A–D).
After analysis by the heart team, surgery was decided, patient was deemed for surgery using a minimally invasive approach (transcatheter aortic valve replacement was ruled out due to the bicuspid morphology and also the small annulus of the valve).
Operative techniqueAfter induction of general anesthetic and placement of a single lumen endotracheal tube, a J-shaped (third intercostal space) upper miniesternotomy was performed. The right common femoral vein was dissected and prepared for peripheral cannulation (venous 25 Fr, high flow cannula, LivaNova, London, UK). Arterial cannulation was performed directly on ascending aorta using a 21 high flow cannulae (LivaNova, London, UK). After comfortable exposure of pericardium, placement of aortic root cardioplegia needle and right superior pulmonary vein vent and initiation of cardiopulmonary bypass, the aorta was cross-clamped and HTK cardioplegia solution was administered. An oblique aortotomy was performed, ending 2cm above the left and non-coronary commissure. Traction sutures were placed on the aorta for better exposure. A tricuspid very calcified valve was noted. Decalcification of annulus and removal of cusps was performed. Sizing of the annulus using the Livanova measure devices demonstrated a 19mm annulus. Due to the high risk of patient protesis mismatch, an annulus enlargement technique was in order.
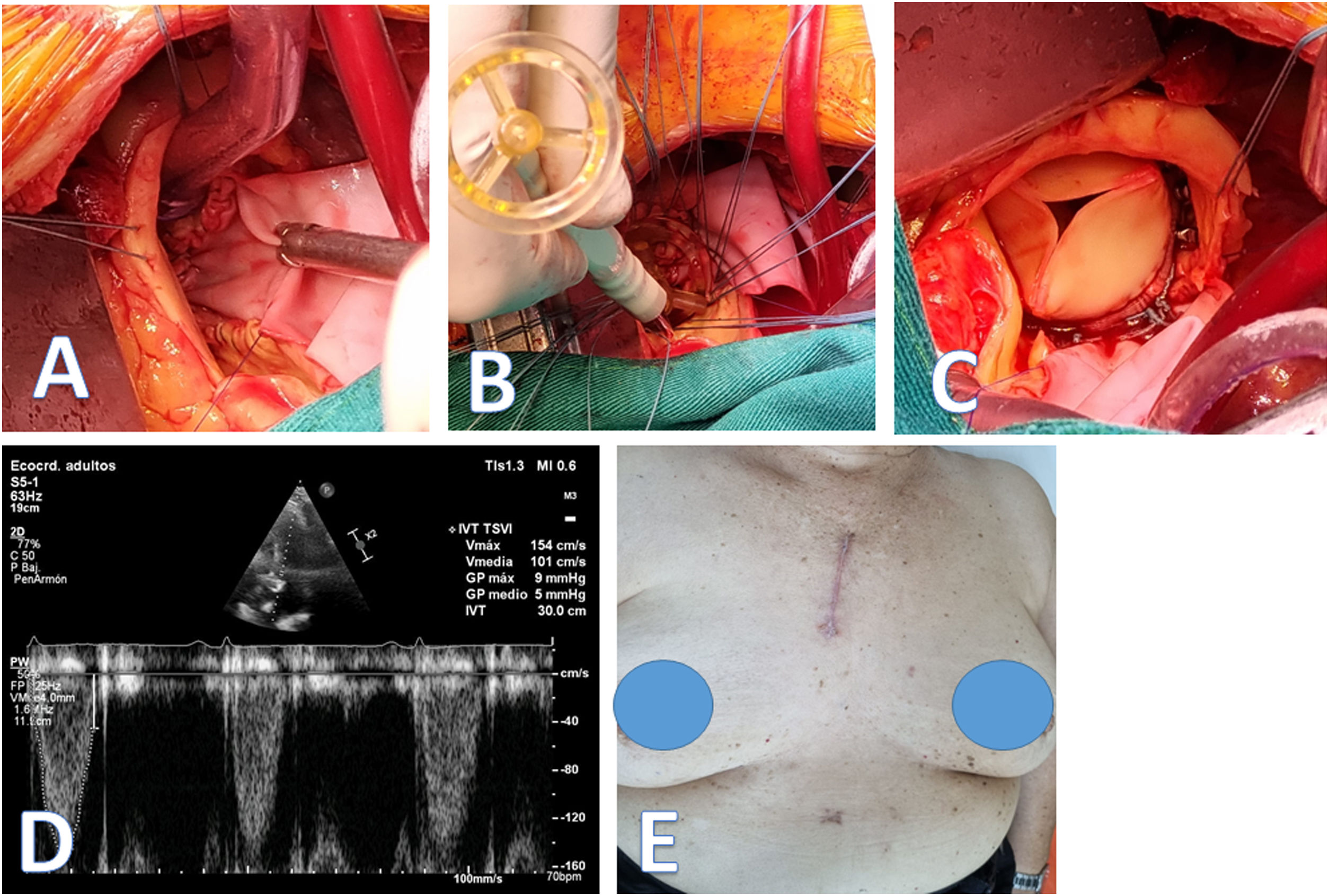
The initial aortotomy ending 2cm above the commissure between left and non-coronary cusp was extended below each cusp on the annulus on to the aorto mitral curtain and then to the right and left, making a “Y” pattern as described by Yang.8 A rectangular-shaped Bovine pericardial patch (Boston Scientific Corp, Natick, Mass) was trimmed in width slightly greater than the distance between the two cusp nadirs. This patch was sewn to the mitral annulus from left to right fibrous trigone with running 4-0 polypropylene suture (Fig. 2A). The suture line was positioned to the aortic annulus at the nadir of both left and non-coronary sinuses, sutured along the longitudinal length of the patch up to the level of the oblique aortotomy incision, and secured. The upsized valve sizer was placed in the enlarged root touching three nadirs of aortic annulus and the position of the sizer on the patch was marked to guide the placement of valve sutures. A 23mm biological aortic prosthesis was placed using an automated suture system (COR-KNOT®) (Fig. 2B and C). The aortotomy was then closed, incorporating the pericardium patch over the entire surface of the open aorta. Intraoperative transesophageal echocardiography demonstrated preserved left ventricular ejection fraction without any evidence of aortic regurgitation, peak AV gradient: 25mmHg, mean AV gradient: 12mmHg. Cardiopulmonary bypass and aortic cross-clamp times were 128 and 114min, respectively. The postoperative course was satisfactory, and patient was discharged home in good condition on the on the eighth postoperative day. After 3 months follow up, peak AV gradient: 9mmHg and mean AV gradient: 5mmHg (Fig. 2D and E).
DiscussionAortic valve stenosis due to degenerative disease is common among older patients. The annulus, root, left ventricle outflow tract tend to be calcified to which careful examination and decalcification is needed. Additionally, older women may usually present with a small root or small annulus. A small aortic root could also be defined as the aortic sinotubular diameter indexed for height, with cutoffs of <1.4cm/m in females and <1.5cm/m in males. There is a strong predilection for the female gender with 88–91% of patients receiving smaller prosthesis. A small aortic annulus which has been accepted as an annulus ≤21mm or some which would not accommodate a prosthesis larger than this size is frequent in this group.9,10
Techniques for annulus enlargement hence have been designed for this group of patients. Yang et al., originated his technique by observation of the increase in prosthesis diameter which could be inserted after reconstruction of aortic root in patients affected by endocarditis compromising the aorto mitral curtain or removal of old mechanical prothesis. It is, up to date, the technique with the maximum increase in annulus diameter. The patient presented in our case was affected with morbid obesity additionally to the very severe aortic stenosis and was target to a bioprosthesis, a substantial risk for patient prothesis mismatch and the degenerative structural damage to the valve which this process implies.
AVR with annulus enlargement through mini-invasive approaches is not new.4 However, this is the first report of a case performed with the Yang technique. In this case we accessed through ministernotomy due to the patient's obesity and because the ascending aorta was located in the midline and we cannulated the femoral vein to have better exposure of the structures to be manipulated. Ministernotomy could reduce ICU stay, bypass, cross-clamping time and reduced bleeding when compared with right thoracotomy.1–3
Although other reports have mentioned minimally invasive approach for aortic valve replacement including or not annulus enlargement, we believe this report is one of the few if not the only one in our region with the novel annulus enlargement technique proposed by Yang. This report emphasizes the need for careful consideration of this kind of techniques for minimizing the feared patient prosthesis mismatch more so in patient with additional risk factors, such as obesity.
Ethical approvalLocal Ethics Committee approved the publication of the case.
Informed consentWritten informed consent was obtained from the patient.
FundingThis work was supported by self-financing.
Conflict of interestsNone declared.