Concomitant cholelithiasis and choledocholithiasis is a disease where incidence increases with age and can have serious complications such as pancreatitis, cholangitis and liver abscesses, but its management is controversial, because there are minimally invasive laparoscopic and endoscopic surgical procedures.
ObjectiveTo compare the efficiency in the management of cholelithiasis and choledocholithiasis with laparoscopic cholecystectomy with common bile duct exploration vs. cholangiopancreatography endoscopic retrograde+laparoscopic cholecystectomy.
Material and methodRetrospective analysis of a five year observational, cross sectional multicenter study of patients with cholelithiasis and concomitant high risk of choledocholithiasis who were divided into two groups and the efficiency of both procedures was compared. Group 1 underwent laparoscopic cholecystectomy with common bile duct exploration and group 2 underwent cholangiopancreatography endoscopic retrograde+laparoscopic cholecystectomy.
Results40 patients, 20 were included in each group, we found p=0.10 in terms of operating time; when we compared hospital days we found p=0.63; the success of stone extraction by study group we obtained was p=0.15; the complications presented by group was p=0.1 and the number of hospitalizations by group was p≤0.05 demonstrating statistical significance.
ConclusionsBoth approaches have the same efficiency in the management of cholelithiasis and choledocholithiasis in terms of operating time, success in extracting stone, days of hospitalization, postoperative complications and conversion to open surgery. However the laparoscopic approach is favourable because it reduces the number of surgical anaesthetic events and the number of hospital admissions.
La colelitiasis y coledocolitiasis concomitante es una enfermedad que aumenta su incidencia con la edad y puede presentar complicaciones graves como: pancreatitis, colangitis o abscesos hepáticos. Su manejo es controversial, ya que existen métodos de mínima invasión laparoscópicos y endoscópicos.
ObjetivoComparar la eficiencia en el manejo de colelitiasis y coledocolitiasis con colecistectomía laparoscópica con exploración de vía biliar vs. colangiopancreatografía retrógrada endoscópica+colecistectomía laparoscópica.
Material y métodoAnálisis retrospectivo de 5 años observacional, transversal, multicéntrico, de pacientes con colelitiasis y alto riesgo de coledocolitiasis, quienes se dividieron en 2 grupos, y se comparó la eficiencia de ambos procedimientos. El grupo 1 fue manejado con colecistectomía laparoscópica con exploración de vía biliar y el grupo 2 con colangiopancreatografía retrógrada endoscópica+colecistectomía laparoscópica.
ResultadosSe incluyó a 40 pacientes, 20 de cada grupo, se encontró una p=0.10 en cuanto al tiempo quirúrgico, al comparar los días de hospitalización se encontró una p=0.63, el éxito de la extracción de litos por grupo de estudio obtuvo una p=0.15, las complicaciones presentadas por grupo mostraron una p=0.1 y el número de hospitalizaciones por grupo presento una p ≤ 0.05, demostrando significación estadística.
ConclusionesAmbos abordajes presentan la misma eficiencia para el manejo de la colelitiasis y coledocolitiasis en cuanto al tiempo quirúrgico, éxito en la extracción de lito, días de hospitalización, complicaciones postoperatoria y conversión a cirugía abierta, sin embargo, el abordaje laparoscópico es favorable, ya que disminuye el número de eventos anestésico-quirúrgicos y el número de internamientos hospitalarios.
In Western societies cholelithiasis is present in approximately 15% of patients. Incidence of choledocholitiasis is between 5% and 10% in patients who have undergone laparoscopic cholecystectomy due to symptomatic cholelithiasis,1,2 between 18% and 33% in patients with acute biliary pancreatitis and between 21% and 34% when choledocholitiasis is secondary to spontaneous stone migration. Choledocholithiasis increases in incidence with age, and is higher than 80% in elderly people over 90.3,4
Within the natural evolution of this disease, there are complications such as biliary pancreatitis, cholangitis or liver abscesses.3,5–7
During primary evaluation liver function tests should be included8,9 and ultrasound images, which have a sensitivity rate of 77–87% to detect dilatation of the bile duct, an event which is commonly associated with choledocholitiasis patients.3,10
Other imaging studies are computed tomography, which has a sensitivity rate of between 65% and 88% and specificity of 73–97% for choledocholitiasis, and cholangioresonance with sensitivity of between 85% and 92% and specificity between 93% and 97% for the detection of choledocholitiasis. However, this sensitivity drops down to 33–71% in the presence of stones under 6mm. Endoscopic ultrasound has a sensitivity of between 89% and 94% and specificity of between 94% and 99% to detect choledocholithiasis. Laparoscopic ultrasound sensitivity is between 71% and 100% and specificity between 96% and 100%. However, all of these studies are higher in cost than ultrasound.8,11
For the study of patients with suspected choledocholithiasis a combination of clinical and laboratory features (liver function tests) are required, together with ultrasound imaging to determine that the patient is at high risk of presenting with choledocholithiasis.8,12
Patients with high risk choledocholithiasis may be treated with a laparoscopic approach (cholecystectomy with common bile duct exploration) via transcystic or transcholedoch route. Success rates are above 90%, morbidity between 8% and 15% and mortality 1%. The necessary material for performing this operation is a cholangiocatheter, choledoscope, Dormia basket, Fogarty catheter, extractor balloon and a team experienced in advanced laparoscopic surgery. This material is not available in all hospital centres. Should this approach fail conversion to laparotomy with exploration of the biliary duct or postoperative endoscopic retrograde cholangiopancreatography with spherincterotomy may be used.1,2,6,13,14 The complications associated with this approach are: bile leak (2–6%), sub-hepatic abscesses (0.7%), residual stones (3–6%), surgical site infection and when there is a T-probe: wrenching or accidental traction of it, infection, obstruction of the bile duct, cholangitis and hydro-electrolyte imbalance.6,15–17
The second approach is through endoscopic retrograde cholangiopancreatography with spherincterotomy, where there is 90% sensitivity and specificity of 8%. Success in stone extraction is between 74.4% and 100%. The rate of morbidity is 5%.3–5,8,18–20 It may be preoperative, interoperative or postoperative, without any differences regarding stone extraction.8,13,15,18 The most frequent complications include: pancreatitis (1.6–15.7%), haemorrhage (1–3%), perforation (0.1–0.6%) and infection in under 1%.21 In terms of public health, efficiency is defined as the use of measures which satisfy to a maximum quantitative or qualitative ends whilst efficacy refers to outcome in terms of goals and the meeting of objectives.22
The aim of this study was to compare the efficacy of laparoscopic cholecystectomy with biliary exploration vs. endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy for the management of patients with cholelithiasis and concomitant choledocholithiasis.
The secondary objective was to compare conversions, the reason for procedure conversion and the number of hospitalisations per procedure.
Material and methodA five-year retrospective analysis was carried out which took place from January 1st 2010 to 31st December 2014 in the Hospitales Centrales de Petróleos Mexicanos (PEMEX): the study was transversal (with a single measurement), observational, analytical and multi-centric. Sample size was obtained out of convenience in a non probabilistic manner. Inclusion criteria included: patients aged 21 or older who had been diagnosed with cholithiasis which had been confirmed by ultrasound and those with concomitant high risk of choledocholithiasis. Exclusion criteria were patients who were: anticoagulated, with a background of chcolecystectomy and with an incomplete record for obtaining the necessary data for the study.
For this study, the variables used to determine the efficiency of the different approaches were: time in surgery, day in hospital, success in stone extraction and postoperative complications. The procedure with at least 3 of these variables with statistical significance was defined as efficient. The patients were divided into 2 groups: group 1 was managed through laparoscopic cholecystectomy with biliary exploration. To do this the hospital had personnel who were skilled in advanced laparoscopic surgery and with the following equipment: choledoscopy, Dormia baskets, Fogarty catheters and extractor balloons. Group 2 was managed through preoperative endoscopic retrograde cholangiopancreatography+laparoscopic cholecystectomy, for which the hospital had a gastrointestinal endoscopy service.
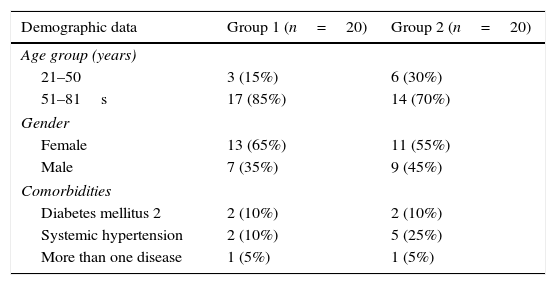
A descriptive demographic analysis was made of both groups by age, gender and comorbidities.
Time in surgery was divided into operations which lasted under 120min and those lasting over 120min, due to the increased anaesthetic-surgical risk with prolonged surgery. Regarding hospital stay 3, groups were formed: the first was for those patients who stayed 1–3 days, defined as the ideal hospital stay; the second group was for 4–7 days and the third group over 7 days. The latter was considered to be a prolonged stay.
Success in stone extraction was defined as complete stone extraction. Postoperative complications studied in this study were as follows: bile leak, pancreatitis post endoscopic retrograde cholangiopancreatography, perforation, cholangitis and infection of the surgical wound.
Ethical issuesThis research study was based on the Helsinki guidelines, the General Law of Health in Research Material for Health (Title V, single chapter, Arts. 96-103) and its Act, the Mexican Official Standard PROYNOM-012-SSA3-2007, and the Code of Ethics for Academic Staff of the Institute of Biomedical Investigations, UNAM, presented in 2005 and revised in 2007; approved by the Committee of Bioethics in the Hospital Central Norte de Petróleos Mexicanos.
Statistical analysisDescriptive demographic analysis was performed with central tendency measures (absolute frequencies, mode, percentages). For comparison between the 2 groups inferential analysis was performed with the use of the Pearson and Fisher Chi square test since nominal variables existed. Statistical significance for this study was defined as a p value of ≤0.05.
ResultsOut of the total of 52 patients with cholelithiasis and choledocholitiasis, 29 were found to have undergone endoscopic retrograde Cholangiopancreatography and laparoscopic cholecystectomy and 23 patients had undergone laparoscopic cholecystectomy with biliary duct exploration. Three patients of group 1 were excluded, because their medical file was incomplete. One patient who was anticoagulant was excluded from group 2 and 8 patients had incomplete files. 40 patients were included in the study, 16 (40%)males and 24 (60%) females. The patients were grouped in ages from 21 to 50 and 51 to 81. 10 of the patients were in the same age group, 71–80. Comorbidities in this study were: diabetes mellitus 2 in 4 patients (10%), systemic hypertension in 7 patients (17.5%) and 5% of patients presented with more than one comorbidity (Table 1).
Demographic data per study group.
| Demographic data | Group 1 (n=20) | Group 2 (n=20) |
|---|---|---|
| Age group (years) | ||
| 21–50 | 3 (15%) | 6 (30%) |
| 51–81s | 17 (85%) | 14 (70%) |
| Gender | ||
| Female | 13 (65%) | 11 (55%) |
| Male | 7 (35%) | 9 (45%) |
| Comorbidities | ||
| Diabetes mellitus 2 | 2 (10%) | 2 (10%) |
| Systemic hypertension | 2 (10%) | 5 (25%) |
| More than one disease | 1 (5%) | 1 (5%) |
Laparoscopic cholecystectomy with biliary duct exploration was performed on group 1 (n=20) and endoscopic retrograde cholangiopancreatography+laparoscopic cholecystectomy was performed on group 2 (n=20).
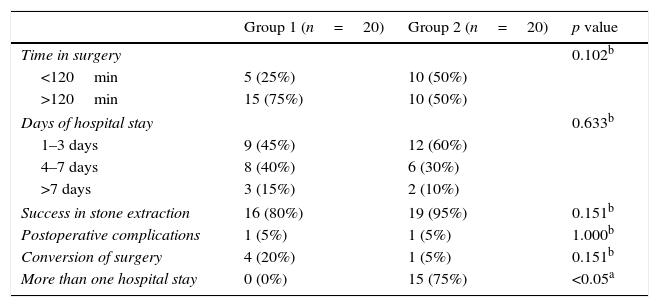
Time in surgery by procedure: In group 1 for 75% (15 patients) of patients the procedure lasted >120min and in group 2 for half of the patients (50%) the procedure lasted >120min. The Chi square test was performed with p=0.10.
Hospital stay by procedure. 21 patients (52.5%) stayed in hospital for 1–3 days, and of these 9 (45%) were from group 1 and 12 (60%) from group 2. In the second group, there were 14 patients (35%) who stayed from 4 to 7 days, 8 (40%) from group 1 and 6 (30%) from group 2. In the third group >7 days, there were 5 patients (12.5%): 3 (15%) from group 1 and 2 (10%) from group 2. When the Chi-square test was performed, p=0.63.
Success of stone extraction according to procedure: In group 1 in 80% (16 patients) of patients the extraction of the stone was achieved and in group 2 success rate was 95% (19 patients), with p=0.15.
Postoperative complications by procedure: In Group 1 there was only one complication (5%), which was bile leak. This was resolved with conservative management. In group 2 a complication arose (5%), pancreatitis post endoscopic retrograde cholangiopancreatography, which evolved favourably with the corresponding medical management. A p=0.1 value was obtained here.
When comparing the conversion of surgery with the procedure used it was found that in group 1, 4 conversions (20%), were made, 3 due to the inability to extract the stone and these patients were treated with conventional bile duct exploration. The stone was therefore extracted and in one patient a Mirizzi syndrome presented with duodenal perforation and it was therefore decided that conversion to surgery and primary closure of the duodenum should be performed. The patient's evolution was satisfactory. In group 2 only one conversion took place (5%) due to anatomical distortion. When the Pearson Chi-square test was performed a value of p=0.151 was obtained.
The number of hospital stays per study group was analysed, where 20 (100%) patients from Group 1 recovered from cholelithiasis and choledocholithiasis during their first stay whilst in group 2, 5 (25%) patients recovered from their pathology in the first stay and 15 (75%) were hospitalised more than once to resolve their problem. The exact Fisher test was performed where a p≤0.05 (Table 2) value was obtained.
Comparison of variables per age group and p value.
| Group 1 (n=20) | Group 2 (n=20) | p value | |
|---|---|---|---|
| Time in surgery | 0.102b | ||
| <120min | 5 (25%) | 10 (50%) | |
| >120min | 15 (75%) | 10 (50%) | |
| Days of hospital stay | 0.633b | ||
| 1–3 days | 9 (45%) | 12 (60%) | |
| 4–7 days | 8 (40%) | 6 (30%) | |
| >7 days | 3 (15%) | 2 (10%) | |
| Success in stone extraction | 16 (80%) | 19 (95%) | 0.151b |
| Postoperative complications | 1 (5%) | 1 (5%) | 1.000b |
| Conversion of surgery | 4 (20%) | 1 (5%) | 0.151b |
| More than one hospital stay | 0 (0%) | 15 (75%) | <0.05a |
With technological advance, new minimally invasive approaches have been sought for different medical conditions, such as the case of patients with cholelithiasis and coledocolitiasis, where there are 2 major management choices: endoscopic and laparoscopic.
The main objective of this study was to compare the efficiency between both approaches regarding hospital stay, time in surgery, success of stone extraction and postoperative complications. When the Chi-square test was performed no statistically significant differences were found in any of the before-mentioned headings, and there efficiency was therefore the same on using either of the 2 before-mentioned approaches.
Few studies have been conducted comparing both techniques. There are 4 meta analyses in existence: 3 of them (Alexakis and Connor in 2012,16 Lu et al. in 201215 and Ainsworth et al. in 201321) where they compare both approaches with regards to the success of the extraction of the stone, the time in surgery, the conversion percentages, hospital stay, morbidity and mortality, with no statistical difference being found between both procedures. The latest meta analysis (Zhu et al.23) refers to the fact that greater success exists in stone extraction and lower time in surgery and shorter hospital stay using laparoscopic cholecystectomy with common bile duct exploration.
As may be observed, the results obtained in several studies are not yet conclusive regarding the approach of choice for this type of pathology. This is due to the fact that few studies have been conducted up until now in this regard, and the majority of those that have been conducted were used small and highly varied samples. Both endoscopic and laparoscopic approaches may therefore be recommended, as their efficiency is similar for the management of patients with concomitant cholelithiasis and choledocholithiasis. Success rates in stone extraction are high, combined with a low percentage in complications. It is important to note that for both procedures it is necessary to have skilled personnel, and a specialised team.
One of the secondary objectives of this study was to determine whether there was a relationship between the type of approach and the conversion to open surgery. No relationship was found. However, we did observe that the majority of conversions were due to the inability to extract the stone. Our study analysed the possible reasons for the inability to extract the stone, e.g. size.
The number of hospital stays required by the patients for complete resolution of the pathology was also analysed (cholelithiasis and choledocholitiasis). Statistically significant differences were found (p≤0.05) for patients who underwent a one-stage approach since they showed a lower number of hospital stays compared with the two-stage approach. In the literature no studies were found that compared the number of hospital stays per procedure used, which would be of vital importance, since reducing the number of readmittances would also reduce costs involved in this pathology. Reductions could also take place in readmittances to emergency services for recurrent bile disorders such as biliary colic, jaundice, biliary pancreatitis, choledocholithiasis and acute cholecistitis that increase patient morbidity and lead to the need to carry out additional procedures for the resolution of this pathology. When the operating theatres were equipped with ideal resources such as fluoroscope equipment, an available endoscopic surgeon, trans-surgical ultrasound equipment, as in several hospitals worldwide, the endoscopic retrograde cholangiopancreatography could be performed interoperatively and the problem of one-stage surgery could thus be resolved.
ConclusionsBoth the one-stage approach (laparoscopic cholecystectomy with bile duct exploration) and the two-stage approach (endoscopic retrograde cholangiopancreatography+laparoscopic cholecystectomy) present equal efficiency for the management of cholelithiasis and choledocholithiasis regarding time in surgery, success in stone extraction, hospital stay, postoperative complications and conversion to open surgery. However, in centres where there is sufficient staff and specialised equipment, the laparoscopic approach is preferred, since it reduces the number of surgical and anaesthetic events as well as the number of hospital admittances.
Both endoscopic and laparoscopic approaches are essential and complementary for patients with cholelithiasis and choledocholithiasis and when performed in well selected patients, present suitable outcomes.
It is necessary to carry out studies with a significant sample size due to the fact that up until now all studies conducted in this respect have small samples.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Herrera-Ramírez MA, López-Acevedo H, Gómez-Peña GA, Mata-Quintero CJ. Eficiencia del manejo laparoscópico vs. endoscópico en colelitiasis y coledocolitiasis. ¿Existe diferencia? Cir Cir. 2017;85:306–311.