Laparoscopic cholecystectomy is a safe and effective treatment and remains the gold standard in patients with benign disease. However it presents difficulties such as: the limited movement range of the instruments, the loss of depth perception, haptic feedback and the fulcrum effect. Previous training can optimise surgical performance in patients to master basic skills.
ObjectiveAssess the effectiveness of surgeons warming up with an endotrainer before performing laparoscopic cholecystectomy.
Material and methodsSingle-blind controlled clinical trial with 16 surgeons who performed 2 laparoscopic cholecystectomies, the first according to standard practice and the second with warm-up comprising 5 MISTELS system exercises. Patient and surgeon demographics were recorded, in addition to findings and complications during and after surgery for each procedured.
ResultsWe found a decrease in surgical time of 76.88 (±18.87) minutes in the group that did not warm up to prior to surgery compared with 72.81 (±35.5) minutes in the group with warm-up (p=0.0196). In addition, increased bleeding occurred in the procedures performed with warm-up 31.25 (±30.85) ml compared with the group that had no warm-up 23.94 (±15.9) (p=0.0146).
ConclusionPerforming warm up on a MISTELS system endotrainer before performing laparoscopic cholecystectomy reduces the operating time of surgery for all surgeons. Surgery bleeding increases in operations performed by surgeons with less experience in laparoscopic surgery.
La colecistectomía laparoscópica es un tratamiento seguro y efectivo, siendo el estándar de oro en pacientes con enfermedad benigna. Sin embargo presenta dificultades como son: el rango limitado de movimiento de los instrumentos, la pérdida de la percepción de la profundidad, la retroalimentación háptica y el efecto fulcro. El entrenamiento previo puede optimizar el desempeño quirúrgico en pacientes al dominar destrezas fundamentales.
ObjetivoValorar la eficacia del calentamiento con endotrainer en médicos cirujanos previo a la realización de colecistectomía laparoscópica.
Material y métodosSe realizó un ensayo clínico controlado ciego simple con 16 médicos cirujanos que practicaron 2 colecistectomías laparoscópicas, la primera con práctica habitual y la segunda con calentamiento previo con 5 ejercicios del sistema MISTELS. Se registraron los datos demográficos de los pacientes y cirujanos así como los hallazgos y complicaciones transquirúrgicas y posquirúrgicas de cada procedimiento.
ResultadosEncontramos una disminución de tiempo quirúrgico de 76.88 (±18.87)min en el grupo que no tenía calentamiento previo a la cirugía comparado con 72.81 (±35.5)min en el grupo que tenía calentamiento previo (p=0.0196). Además, observamos aumento el sangrado en los procedimientos que se realizaron con calentamiento previo, 31.25 (±30.85)ml, comparado con el grupo que no tuvo calentamiento 23.94 (±15.9) (p=0.0146).
ConclusiónLa realización de ejercicios de calentamiento en endotrainer con el sistema establecido MISTELS previo a la realización de colecistectomía laparoscópica disminuye el tiempo quirúrgico de la cirugía en todos los cirujanos. El sangrado de la cirugía aumenta en los cirujanos que cuentan con menos experiencia en cirugía laparoscópica.
Surgical interventions of the biliary tree are amongst the most common abdominal surgical procedures. Laparoscopic cholecystectomy is a safe and effective form of treatment which is the gold standard in patients with benign disease.1–3
Laparoscopic surgery has revolutionised the practice of the majority of surgical subspecialties during the last 2 decades.4 In general, the outcome of laparoscopic surgery is smaller and less painful scars after surgery and a fast recovery compared with laparotomy and as a result it is currently the best option.4–6
It has been calculated that at present over 90% of cholecystectomies are performed with a laparoscopic approach.1 However, this method has been associated with an increase in complications relating to open surgery, in a range between 0.4% and 2%, and in emergency surgery there may be a significant rise in morbidity and mortality, which may reach up to 40%–70%.7 There is still a substantial variation in the conversion rates reported between laparoscopic cholecystectomy with open cholecystectomy which ranges from 2% to 10%,8 and with a higher percentage when emergency surgery is performed.9
Morbidity for laparoscopic cholecystectomy is calculated at 10% with mortality under 0.5%.2,10
Within the complications related to laparoscopic extirpation of the gallbladder are biliary tree injuries and non-biliary injuries (intestinal, gallbladder, diaphragmatic or vascular injury), which have repercussions on morbidity and mortaility11 and are potentially preventable.12 There may also be complications from surgery such as haemorrhaging, retained stones, pancreatitis, infections from surgical wounds and incisional hernias.11
There is controversy surrounding determining the number of operations necessary for a surgeon to be considered an expert in laparoscopic cholecystectomy, taking as the cut off point the number of procedures in which a reduction of the frequency of complications has arisen, with the estimate being between 50 and 200 procedures, depending on the literature.13
Laparoscopic surgery presents difficulties such as: the limited movement range of the instruments, the loss of depth perception, haptic feed-back and the fulcrum effect.14–16 Therefore, owing to the general acceptance of minimally invasive techniques the development of new and complex technical skills have been required. Major skills are required in laparoscopic surgery, such as hand-eye coordination and the perception of three-dimensional visual space through a monoocular view system, where everything is easy to reproduce in an inanimate system.17
Up until recently learning any surgical procedure was based on its practice, which was initially supervised, on the actual patients.
This entailed a long learning curve with higher rates of morbidity and possibly mortality, and also poorer long term outcomes. Furthermore, learning increased surgical costs due to prolongation of surgery. To speed up learning, training labs have been developed where practices can be performed using virtual reality with physical simulator systems.18–20
Prior training may optimise surgical training on patients as essential skills are gained and the experienced surgeon can then concentrate on making intraoperative decisions without any lack of expertise becoming a distraction.21
Several inanimate and virtual reality systems were designed to facilitate the improvement of laparoscopic techniques and to assess the skills of students and surgeons as described in McGill's inanimate system for the training and evaluation of laparoscopic skills (MISTELS), which consists in a series of standardised tasks undertaken in a training box using an optics system and evaluating speed and precision.22 It has been shown that 15–20min warm-up leads to a global reduction of 33% in errors in a series of exercise which simulate surgical skills but it is however unclear as to whether performing these tasks leads to an improved performance in the operating theatre.17
Given that training in a simulator requires an investment in both equipment and time required for training, it is important that this investment is justified and that it demonstrates its value in the skills needed in the operating theatre.23
In this study we evaluate the efficacy of warm-up with the end trainer in surgeons, prior to undertaking laparoscopic cholecystectomy.
Material and methodsA single blind controlled clinical trial was performed in the General Surgery Unit of the “Dr. Fernando Quiroz Gutierrez” of the Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado during the period between 1st September and 20th December 2015. The study was submitted and authorised by the ethics committee of the same hospital. 16 doctors from the general surgery speciality were included, with habitual practice in laparoscopic cholecystectomy (Table 1), and patients hospitalised for carrying out programmed surgery with diagnosis of cholelithiasis or chronic lithiasic non-acute cholecystitis, with an age range of between 18 and 85 years with ASA I–III (Table 2). Patients diagnosed with gallbladder dyekinesia were excluded, as were surgical procedures that were converted to open surgery and those which were associated with other surgical events.
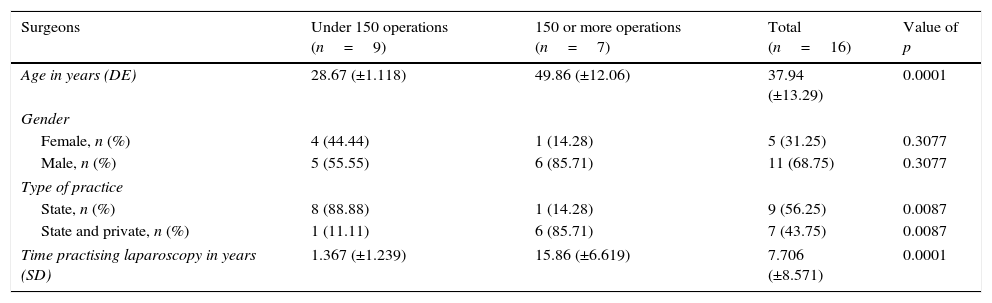
Demographic surgeon data.
| Surgeons | Under 150 operations (n=9) | 150 or more operations (n=7) | Total (n=16) | Value of p |
|---|---|---|---|---|
| Age in years (DE) | 28.67 (±1.118) | 49.86 (±12.06) | 37.94 (±13.29) | 0.0001 |
| Gender | ||||
| Female, n (%) | 4 (44.44) | 1 (14.28) | 5 (31.25) | 0.3077 |
| Male, n (%) | 5 (55.55) | 6 (85.71) | 11 (68.75) | 0.3077 |
| Type of practice | ||||
| State, n (%) | 8 (88.88) | 1 (14.28) | 9 (56.25) | 0.0087 |
| State and private, n (%) | 1 (11.11) | 6 (85.71) | 7 (43.75) | 0.0087 |
| Time practising laparoscopy in years (SD) | 1.367 (±1.239) | 15.86 (±6.619) | 7.706 (±8.571) | 0.0001 |
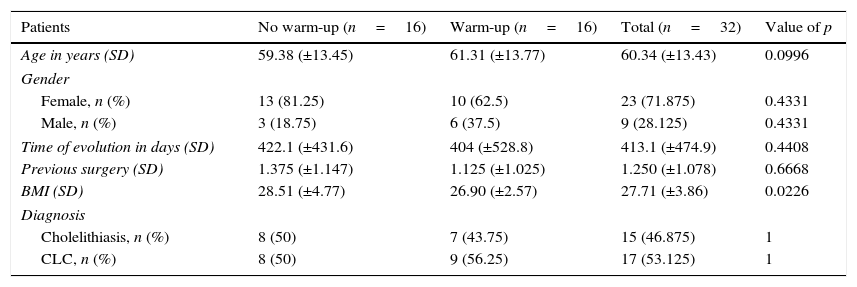
Clinical and demographic data of patients undergoing surgical laparoscopic procedures.
| Patients | No warm-up (n=16) | Warm-up (n=16) | Total (n=32) | Value of p |
|---|---|---|---|---|
| Age in years (SD) | 59.38 (±13.45) | 61.31 (±13.77) | 60.34 (±13.43) | 0.0996 |
| Gender | ||||
| Female, n (%) | 13 (81.25) | 10 (62.5) | 23 (71.875) | 0.4331 |
| Male, n (%) | 3 (18.75) | 6 (37.5) | 9 (28.125) | 0.4331 |
| Time of evolution in days (SD) | 422.1 (±431.6) | 404 (±528.8) | 413.1 (±474.9) | 0.4408 |
| Previous surgery (SD) | 1.375 (±1.147) | 1.125 (±1.025) | 1.250 (±1.078) | 0.6668 |
| BMI (SD) | 28.51 (±4.77) | 26.90 (±2.57) | 27.71 (±3.86) | 0.0226 |
| Diagnosis | ||||
| Cholelithiasis, n (%) | 8 (50) | 7 (43.75) | 15 (46.875) | 1 |
| CLC, n (%) | 8 (50) | 9 (56.25) | 17 (53.125) | 1 |
CLC: chronic lithiasic cholecystitis; BMI: body mass index (kg/cm2).
Each surgeon practised 2 laparoscopic cholecystectomies, the first with the standard practice with direct entry into the surgery and the second on a different day and with a different patient, with a warm-up of 5min prior to the surgical procedure commencing. The warm-up was carried out by an endotrainer (LAPA-PROMR) (Fig. 1) which consists of a training box with 2 12mm trocars in suitable angles each side of the lens. The optic system is formed by a camera and a video monitor which is placed in line with the operator. The instrument used for the exercises is the same as that used in real surgery (grasper, meryland, scissor, low knots and needle holder). The warm-up exercises are based on the MISTELS system which consists in the execution of 5 tasks: Transference. With the use of 2 pincers, the operator are required to lift each of the 6 nails on a panel, transfer to the other pincer and then place it on the second panel within an expected time of 300s. Cut. This requires cutting a 5cm pre-sketched circle onto a double sided 10×10cm gauze, in 300s. Endoloop. A predesigned slilpknot is placed along a circumferential line marked in a tubular foam attachment at an expected time of 180s. Extracorporeal knot. Suture of 12cm in length is placed at an extracorporeal technique using a knot pusher, at an expected time of 300s. Intracorporeal knot. 12cm suture is used to make an intracorporal knot within 300s.23,24 (Fig. 2).
A record identifying the surgeon and patients was made for each of the laparoscopic procedures and also the intraoperative and postoperative events and complications.
Statistical analysisThe information was collected using the Excel programme (Microsoft Corporation, USA). For statistical calculations the software Graph Pad Prism V-6.01 (GraphPad Software, San Diego, Cal., USA.) was used. Distribution of the continuous variables was expressed as a mean±standard deviation (SD) and percentages. The Mann–Whitney U tests were used to compare continuous variables and the Kruskal–Wallis test to analyse the means of multiple groups and the difference in individual groups was confirmed with the Friedman post hoc test. p<0.05 was regarded as a statistically significant value.
Results16 surgeons took part as this was the maximum availability within the hospital, 5 (31.25%) of whom were women and 11 (68.75) men. They were divided into 2 groups based on the number of laparoscopic cholesystectomies they had performed when the study took place (under 150 and over 150). The age of the surgeons was 37.94 (±13.29) years (Table 1). With regard to the type of practice observed, only state hospital practice was observed in 9 (56.25%) surgeons and both state and private was observed in 7 (43.75%) Time in years of laparoscopic tube practice was at a mean of 7.706 (±8.571) at the time of the study (Table 1).
Out of a total of 32 patients who were scheduled for laparoscopic cholecystectomy, a divison into 2 groups was made, with and without pre-surgical warm-up. Out of the total of patients 23 (71.875%) were women and 9 (28.125%) men. With regard to diagnosis, 15 (46.875%) presented with cholelithiasis and 17 (53.125%) with chronic lithiasic cholecystitis. Age was 60.34 (±13.43). The time of evolution of the disease was 413.1 (±474.9) days. The number of previous abdominal operations was 1.250 (±1.078). BMI was 27.71 (±3.86) (Table 2).
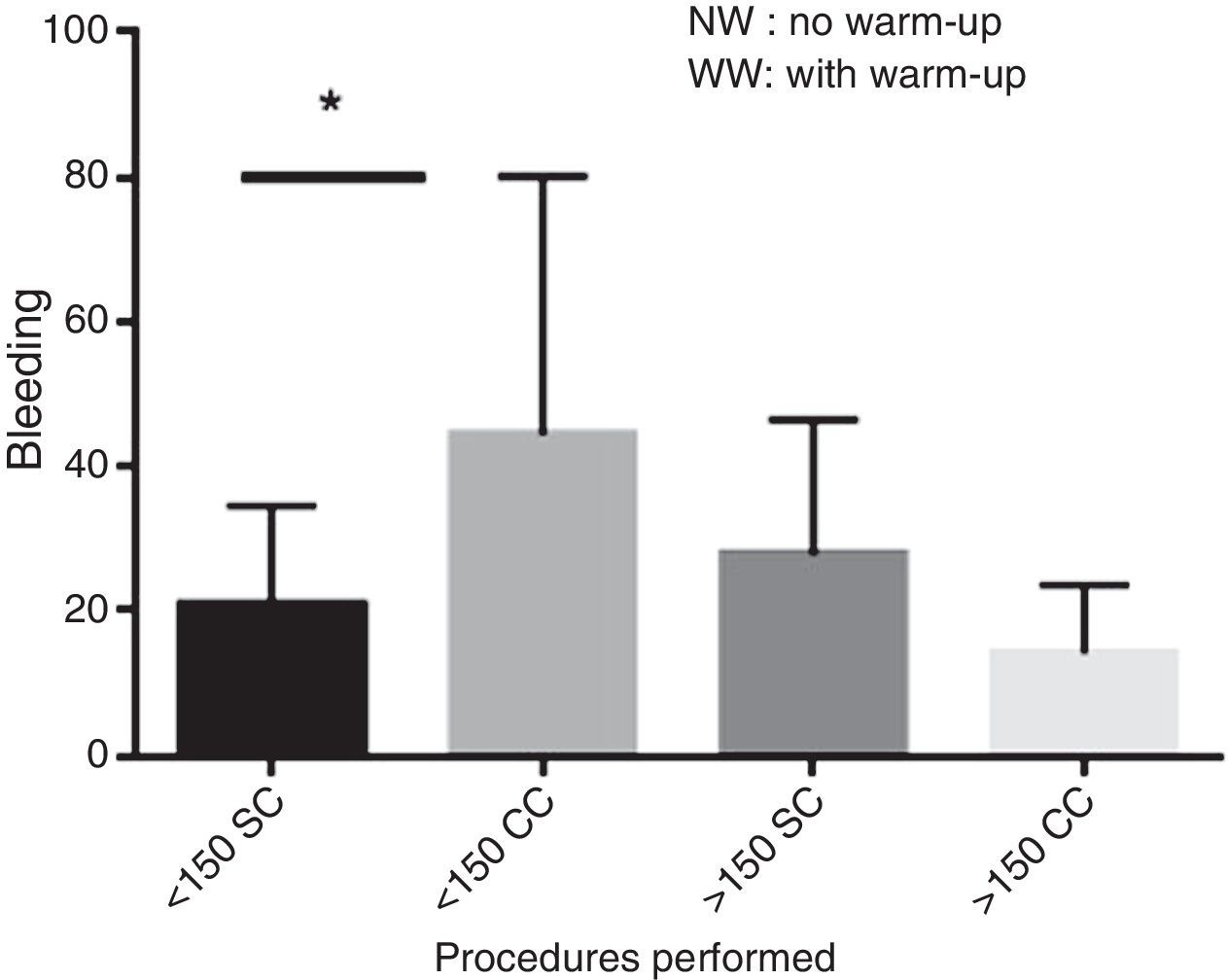
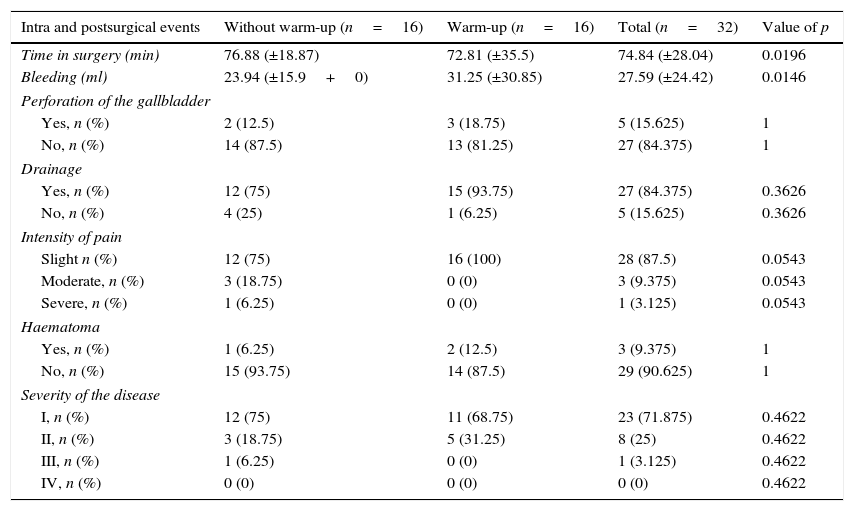
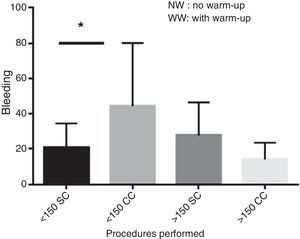
The results of the 2 groups with and without warm-up to surgery revealed that there was a reduction in surgery time of 76.88 (±18.87)min in the group which did not have a warm-up to surgery compared with 72.81 (±35.5)min in the warm-up (p=0.0196) group. There was an increase in total bleeding in procedures performed with warm-up, 31.25 (±30.85)ml, compared with that with no warm up 23.94 (±15.9) (p=0.0146) (Table 3). When bleeding was determined in accordance with the number of laparoscopic procedures performed by the surgeon we found that the group of under 150 procedures who did warm-up presented bleeding of 44.44 (±35.66)ml compared with those who did not do warm-up exercises, of 20.89 (±13.72)ml in the same group (p=0.014) (Fig. 3). In the group who had performed over 150 over laparoscopic procedures prior to surgery we found that those who had warmed up had bleeding of 14.29 (±9.32)ml compared with the non-warm-up group of 27.86 (±18.68) ml (p=0.150) (Fig. 3).
Intraoperative and postoperative events of laparoscopic procedures in groups with and without warm-up.
| Intra and postsurgical events | Without warm-up (n=16) | Warm-up (n=16) | Total (n=32) | Value of p |
|---|---|---|---|---|
| Time in surgery (min) | 76.88 (±18.87) | 72.81 (±35.5) | 74.84 (±28.04) | 0.0196 |
| Bleeding (ml) | 23.94 (±15.9+0) | 31.25 (±30.85) | 27.59 (±24.42) | 0.0146 |
| Perforation of the gallbladder | ||||
| Yes, n (%) | 2 (12.5) | 3 (18.75) | 5 (15.625) | 1 |
| No, n (%) | 14 (87.5) | 13 (81.25) | 27 (84.375) | 1 |
| Drainage | ||||
| Yes, n (%) | 12 (75) | 15 (93.75) | 27 (84.375) | 0.3626 |
| No, n (%) | 4 (25) | 1 (6.25) | 5 (15.625) | 0.3626 |
| Intensity of pain | ||||
| Slight n (%) | 12 (75) | 16 (100) | 28 (87.5) | 0.0543 |
| Moderate, n (%) | 3 (18.75) | 0 (0) | 3 (9.375) | 0.0543 |
| Severe, n (%) | 1 (6.25) | 0 (0) | 1 (3.125) | 0.0543 |
| Haematoma | ||||
| Yes, n (%) | 1 (6.25) | 2 (12.5) | 3 (9.375) | 1 |
| No, n (%) | 15 (93.75) | 14 (87.5) | 29 (90.625) | 1 |
| Severity of the disease | ||||
| I, n (%) | 12 (75) | 11 (68.75) | 23 (71.875) | 0.4622 |
| II, n (%) | 3 (18.75) | 5 (31.25) | 8 (25) | 0.4622 |
| III, n (%) | 1 (6.25) | 0 (0) | 1 (3.125) | 0.4622 |
| IV, n (%) | 0 (0) | 0 (0) | 0 (0) | 0.4622 |
Perforation of the gallbladders took place in 2 (12.5%) patients of the no warm-up to surgery group versus 3 (18.75%) patients of the group with warm-up (p=1). A Penrose type drainage was used in the no warm-up group in 12 (75%) of patients compared with 15 (93.75%) patients in the warm-up (p=0.3626) group. The intensity of pain in the first 12 hours after surgery was classified as minor, moderate and severe, and was found to be in the group which had no warm-up to surgery 12 (75%), 3 (18.75%) and one (6.25%) patients respectively compared with 16 (100%), 0 and 0 patients in the warm-up group (p=0.0543). 3 patients presented with haematoma in one of the surgical wounds representing 9.375%, of them 2 (12.5%) belonging to the group with warm-up to surgery and one (6.25%) in the group without warm-up (p=1). In accordance with the severity of the gallbladder disease, it was classified into grade I, II, III and IV, with 12 (75%), 3 (18.75%), one (6.25%) and 0 patients respectively in the non-warm-up group versus 11 (68.75%), 5 (31.25%), 0 and 0 patients respectively in the group with warm-up (p=0.4622) (Table 3).
None of the patients presented with a biliary injury, or a vascular or visceral injury. During postoperative monitoring none of the patients had a fever nor were there any biliary liquid leaks.
DiscussionRecently, the general acceptance of minimally invasive techniques has required the development of new and complex technical skills. Moreover, the inanimate systems enable practice with the same instruments used in the operating theatre but in a more relaxed atmosphere and with no time limitations being present in the operating theatre.17
In our study we observed that the period of adaptation was lower, that a surgeon should have on beginning laparoscopic surgery based on visual perception and a combination of movements med, which was interpreted as a reduction in time in surgery in the group of surgeons who carried out, no warm-up to surgery, with a statistically significant difference between both groups (p=0.0196). The training box used in the study enables major laparoscopic characteristics to be recreated and with the same instrument which would be standard in that surgery.
With regard to total bleeding, during the surgical procedures there was an increase in bleeding in operations where the surgeon had performed warm-up, and this predominated in the group of surgeons with less experience, i.e. those who had performed under 150 operations, with a statistically significant difference between both groups (p=0.014). This may have been due to previous practice with inert exercises and materials and not in tissues, which could had led to greater movement and force in movement, compared with live tissue.
In this study we observed that there is a predominance of males within the surgical area of the hospital, and we also found that surgeons with greater experience in laparoscopic surgery work in both state and private practice. In patients there was a predominance of women which corresponds with the literature regarding the predisposition of this gender to present with a gallbladder lithiasic illness.25
In our sample we observed that patients in both study groups were obese patients, which also reflects the characteristics of the population who are undergoing surgery, with increased risk for complex laparoscopic cholecystectomy.26–28 Biliary injuries are reported in the literature with an incidence of as 0.4%–0.6%, but during the study no biliary, vascular or visceral injury presented.
The goals of these study plans based on the simulator are to provide an opportunity to learn and practice basic surgical skills such as the development of cognitive and psychomotor skills in a relaxed ambiance and low cost, to achieve a basic level of technical skills which may be transferred from the laboratory to the operating theatre. For this reason it is essential to conduct multicentric studies with both experienced surgeons and with resident doctors and to demonstrate the relevance of the warm-up exercises in a training box prior to laparoscopic surgery. This practice must be introduced into hospitals where these surgical events are carried out so as to improve medical practice.29
ConclusionsPerforming warm-up exercises in a training box with the MISTELS panel system prior to carrying out laparoscopic cholecystectomy reduces time in surgery for all surgeons. Bleeding in surgery increases for surgeons with less experience in laparoscopic surgery in comparison with those with greater expertise in this procedure. The number of surgeons evaluated needs to be increased to demonstrate the usefulness of warm-up exercises in a training box prior to laparoscopic surgery.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Our thanks to the staff in the surgical area of the General Hospital “Dr. Fernando Quiroz Gutiérrez” for the availability and facilities provided for this study.
Please cite this article as: Troncoso-Bacelis A, Soto-Amaro J, Ramírez-Velázquez C. Calentamiento en endotrainer previo a colecistectomía laparoscópica. Cir Cir. 2017;85:299–305.