Gallbladder cancer ranks fifth among oncological diseases affecting the gastrointestinal tract; nevertheless, it is the world's most common malignant tumour of the bile ducts. It is usually diagnosed after cholecystectomy and tends to have bad prognosis. Adenocarcinoma is the main histological finding, although other rare histologic types have been described among the actual literature. Poorly differentiated squamous-cell neuroendocrine gallbladder carcinoma is an extremely rare neoplasm. A poor prognosis is associated with this histological type.
AimThe aim of this paper is to show that performing a systematic exploration of the entire peritoneal cavity in all laparoscopic surgeries can lead to find completely unexpected changes related to an unidentified disease. Also, a detailed review of our unexpected finding is made: The neuroendocrine small cell carcinoma of gallbladder.
Clinical caseWe hereby report the case of a 40-year-old patient with a ruptured ectopic pregnancy that underwent emergency laparoscopic surgery, presenting the incidental finding of a small-cell carcinoma of the gallbladder.
ConclusionsOur surgical group advised that by introducing the laparoscope, the entire peritoneal cavity must be systematically reviewed, in search of differential diagnoses and unidentified pathologies. We must use the diagnostic and therapeutic qualities of laparoscopy. Bile duct endocrine tumours tend to remain silent until advanced stages, making the prognosis usually unfavourable, especially when they are unresectable. Endocrine neoplasias of the gallbladder, although uncommon, should be taken into account as possible diagnoses due to its therapeutic and prognostic implications.
El cáncer de vesícula biliar ocupa el quinto lugar entre los cánceres que afectan al tracto gastrointestinal; mundialmente es el tumor maligno más frecuente de las vías biliares. El adenocarcinoma es el hallazgo histológico principal. Se han referido en la literatura variedades histológicas menos frecuentes. El carcinoma neuroendocrino pobremente diferenciado de células pequeñas de la vesícula biliar es una neoplasia extremadamente rara y esta estirpe histológica se asocia a un pronóstico muy precario.
ObjetivoDemostrar que realizando una exploración sistemática de toda la cavidad peritoneal, en la totalidad de las cirugías laparoscópicas que se realicen, es posible encontrar cambios completamente inesperados, relacionados con una enfermedad no identificada. Además, se realiza una revisión detallada de nuestro hallazgo inesperado, el carcinoma neuroendocrino de células pequeñas de vesícula biliar.
Caso clínicoPresentamos el caso de una paciente de 40 años de edad con un embarazo ectópico roto, que fue tratado mediante cirugía de urgencia, abordada laparoscópicamente. Se encontró como hallazgo incidental un carcinoma de células pequeñas en la vesícula biliar.
ConclusionesNuestro grupo quirúrgico aconseja que, al introducir el laparoscopio, se revise sistemáticamente toda la cavidad peritoneal, en busca de diagnósticos diferenciales y enfermedades no identificadas. Deben aprovecharse las cualidades exploratorias, diagnósticas y terapéuticas de la laparoscopia. Los tumores endocrinos biliares suelen permanecer silentes hasta estadios avanzados. El pronóstico suele ser desfavorable, especialmente cuando son irresecables. La neoplasia endocrina de vesícula biliar, a pesar de ser infrecuente, debe tenerse en cuenta como posibilidad diagnóstica ante las implicaciones terapéuticas y pronósticas.
Laparoscopic surgery is amongst first line technological advances which have aided the introduction of new surgical techniques. Their development has therefore been lauded as a historical milestone leading to a new era of technology-dependant surgery. Despite the controversy which has accompanied the implementation of laparoscopic surgery, in just two decades this technique has revolutionised surgical practice, to the point where it surpasses all initial expectations. The influence of laparoscopic surgery has had an effect on all surgical specialities, and this technique is currently firmly established in surgical practice. Laparoscopic surgery has matured in many ways and is now an essential surgical tool, due to lower morbidity in procedures such as cholecystectomy, appendicectomy, fundoplication, abdominal and inguinal hernia repair and even in gastric bypass surgery. The dual power of laparoscopy is that it may be used for diagnostic purposes such as cancer staging, acute abdominal pain diagnosis, chronic condition diagnosis and for other general reviews, examination of complications and therapeutic purposes. Both laparoscopic approaches should always be used because, as seen from our case, there may be unimaginably favourable benefits for the patients.
ObjectiveWe wish to demonstrate that by performing a systematic exploration of the entire peritoneal cavity, in all laparoscopic surgeries performed, it is possible to find completely unexpected changes related to unidentified diseases. Furthermore, a detailed review of this unexpected finding led to a diagnosis of neuroendocrine small-cell carcinoma of the gallbladder.
Clinical caseWe present the case of a 40-year-old female, with the following clinical history: diabetes mellitus type two genetic load, with no genetic load for oncological conditions; no smoking habit; a social drinking habit without ever being inebriated; no other drug addictions. Her blood group was O Rh (+), COMBE test negative. Educational level: a law graduate. Obstetrics and gynaecological background: began menstruating at 12 years of age, irregular rhythm, and delayed menstruation with cycles of 36–37×6 days, an active sexual life and without the use of any birth control methods. She stated that her last menstruation had presented 38 days prior to consultation. Pregnant 3 times, 2 caesarean sections, 1 abortion. Her last smear test and mammography tested with no signs of malignancy, as stated by the patient. No signs of allergies, She had undergone 2 caesarean sections with no trauma or blood transfusions or chronic degenerative. The patient stated she suffered from migraine which she treated with ibuprofen and caffeine.
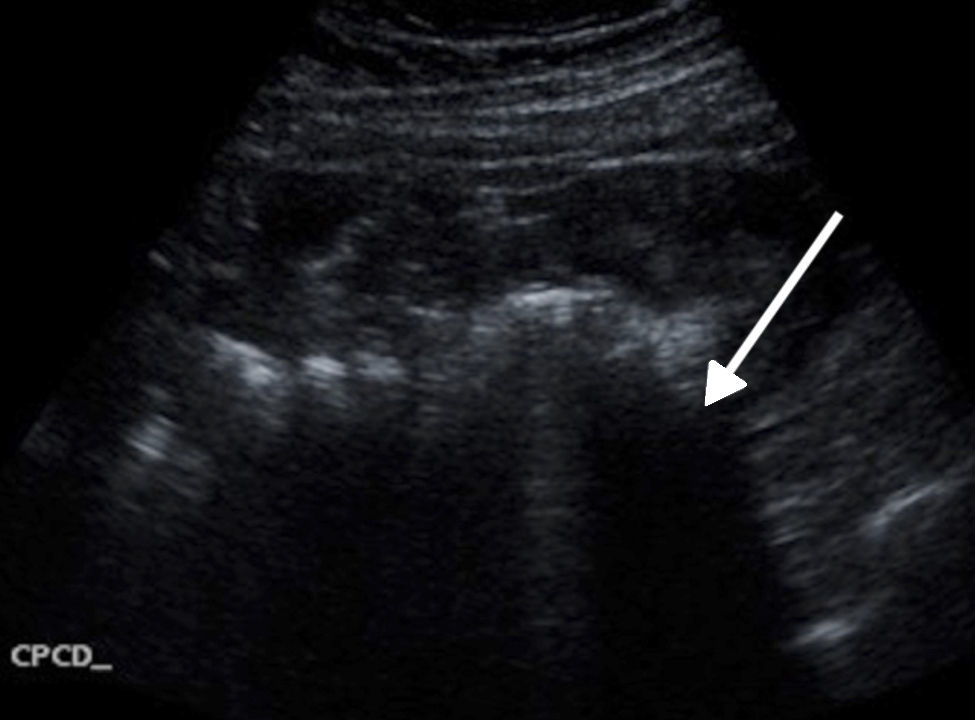
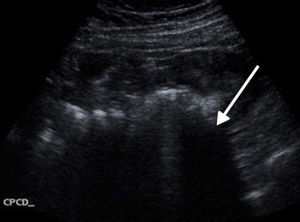
The patient went to the emergency service after presenting with a 2 week long colicky abdominal pain which was intermittent and of 5/10 intensity, which began in the hypochrondrium and spread to the right-handside of the back, without exacerbating. On the day of consultation she had been suffering from abdominal pain for several hours, located in a lower hemi-abdomen, predominantly in hypogastrium and right iliac fossa, of great intensity from the start, and which scored 7/10 on the verbal analogue scale. The pain began suddenly, was of growing intensity, persistent, colicky in type, incapacitating with no clear attenuation or exacerbation, no irradiation, and accompanied by shivering, no fever, with nausea and retching without vomiting. The patient denied any urinary changes, alterations of intestinal habits or vaginal fluid. On physical examination the patient was found to be haemodynamically stable with the following vital signs: heart rate of 90 beats per minute, 20 breaths per minute, blood pressure of 135/88mmHg, oxyhaemoglobin saturation levels of 95% with pulse oxymetry and temperature of 36.8°C, alert, conscious, orientated, pale and with dehydrated mucosa. Physical examination revealed a swollen abdomen at the expense of fat thickness and distension, with muscular resistance and pain on general surface palpation. There were signs suggestive of peritoneal and tympanic irritation and hypoactive peristalsis. Preclinical tests were therefore requested with the following findings: haemoglobin 12.9mg/dl, platelets 236,000mm−3, leukocytosis of 20,700mm−3 at the expense of neutrophilia 18,800mm−3, glucose 148mg/dl. A general urine study tested negative and quantitative determination of human chorionic gonadotrophin fraction was 1,464 mUI/ml. We decided to perform a transvaginal and abdominal ultrasound where abundant free fluid was observed in the abdominal cavity, compatible with probable haemoperitoneum (Fig. 1).
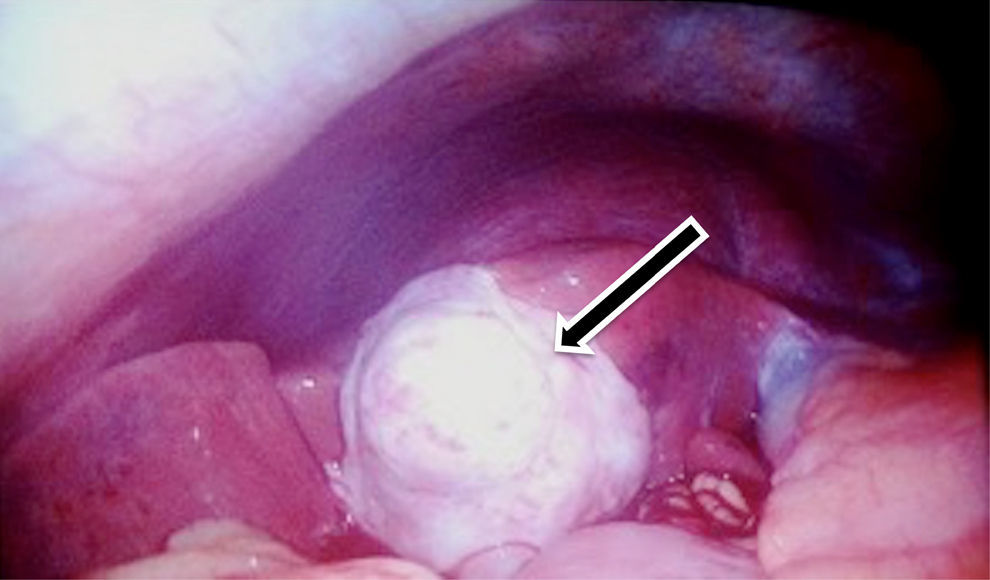
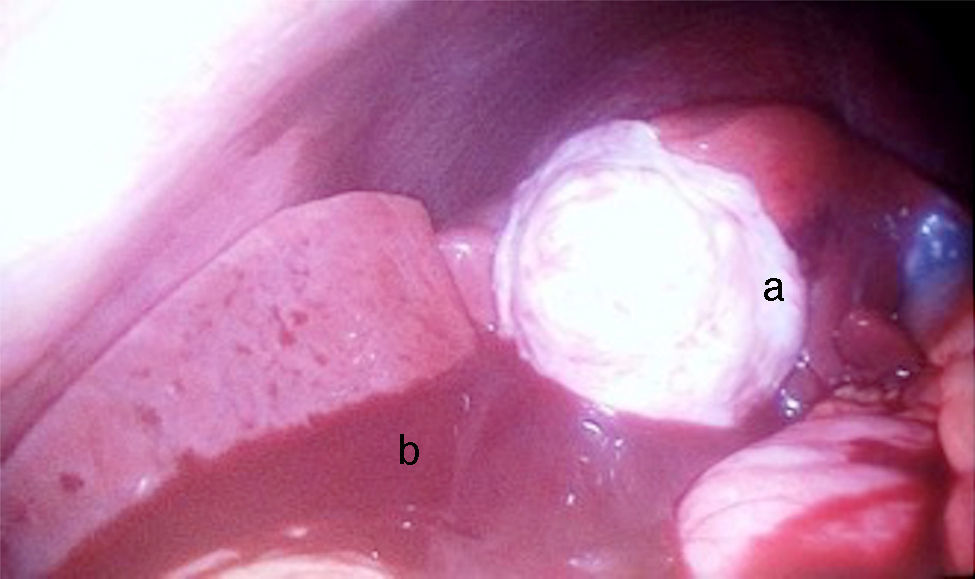
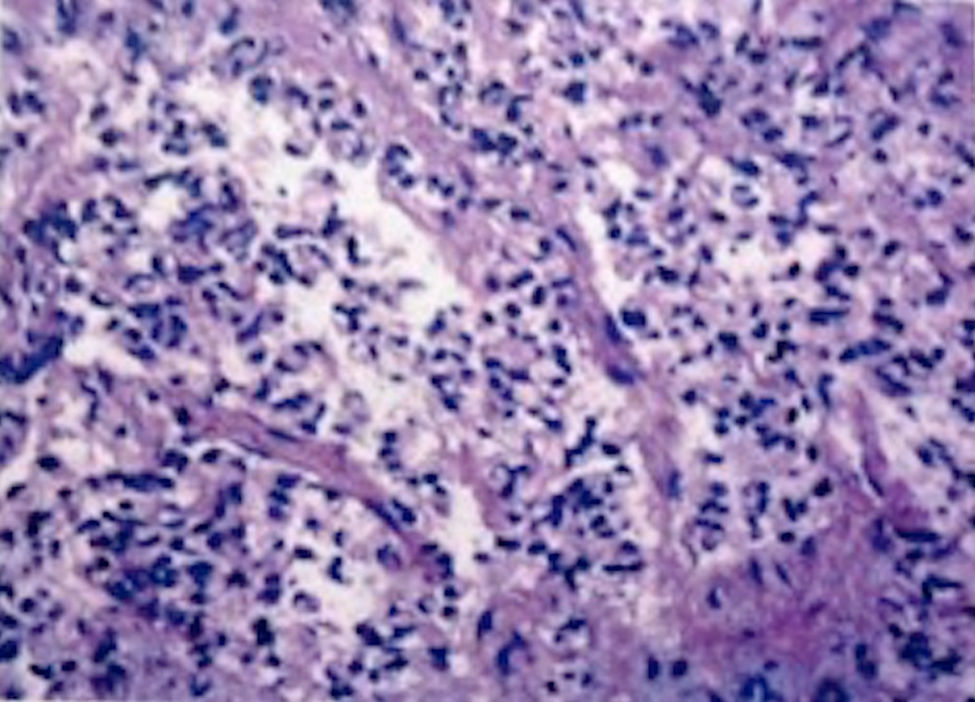
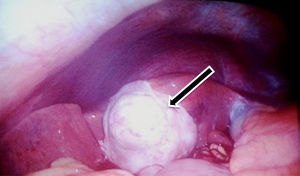
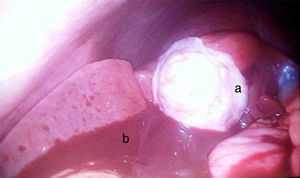
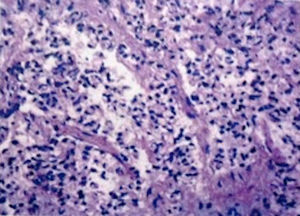
A laparoscopic approach was used where the following intraoperative findings were made: (a) haemoperitoneum of approximately 1500–2000cc, secondary to ruptured right ampullary ectopic pregnancy. Right salpingectomy with strict application of hemostasis, irrigation and drainage of abdominal cavity was performed; (b) caecal appendix of normal appearance and (c) new vessel growth at the expense of the whole gallbladder, which was white, with an uneven surface area, firm, grainy, extending to the IV A hepatic segment (Couinaud classification), which had invaded the vesicular pedicle, part of the duodenal knee and part of the stomach (Figs. 2 and 3). The diagnostic laparoscopy did not reveal any sign of metastases, and an incisional biopsy was thus obtained from the laparoscopy and the specimen was sent to the laboratory. The clinical report showed: (a) the ectopic pregnancy had several tissue fragments which together measured 3cm×2cm×1cm and were irregular to one another; 2cm×1.3cm salpinx of red-brown serosa. When cut dilated light with haematic matter was observed. The final diagnosis was of ruptured ectopic pregnancy. (b) During the transoperative period an irregular fragment of tissue described as gallbladder tissue which measured 0.7cm×0.6cm×0.5cm and was grey in colour of firm consistency, was sent for testing. Neuroendocrine small-cell carcionoma was diagnosed (Fig. 4), and immunohistochemical analysis confirmed the diagnosis. Immunostaining for chromogranin and synaptophysin were intense and diffusely positive, whilst the immunostaining for CD56 was negative.
Once the diagnosis had been established and the particular patient conditions established, we decided to terminate the surgical procedure and requested medical and oncological interconsultation to define final patient management with the surgical team.
Post surgical laboratory findings showed: Hb 10.3mg/dl, Hto 30.6%, platelet count 142,000mm−3, leukocytes 10,300mm−3, Na+ 129mmol/l, K+ 3.1mmol/l, glucose 108mg/dL, Cr 0.3mg/dL, Alb 2.3g/dL, TB 1.98mg/dL, LB 1.75mg/dL, TGO 26U/l, TGP 31U/l, LD 125U/l, GGT 21U/l and AP 35U/l.
The oncology department decided to let the patient convalesce from the surgery performed and readmit her in one or 2 weeks to perform a El PET-CT scan and from those results, define which procedure to follow. If the disease was localised surgery would be performed or if metastases was identified she would initiate chemotherapy with paclitaxel+carboplatin+etoposide. The treatment options were discussed with the patient and her family members. As the patient was not covered by a medical insurance, it was decided that she should be transferred to a National Health Hospital.
The patient's current condition is unknown owing to the fact contact with her was lost.
DiscussionThe advantages of performing diagnostic laparoscopy as standardThe emergence of laparoscopy has been a surgical milestone, progressively transforming the era of open abdominal surgery to that of minimally invasive surgery. Laparoscopy is performed with the therapeutic intention of confirming a diagnosis established through a different method but may in itself be diagnostic and when performed with diagnostic intentions may often become therapeutic and in many cases lead to a complete resolution of the patient's disease through minimally invasive methods. The exploratory, diagnostic and therapeutic qualities of laparoscopy should always be used. A laparoscopy can show a large part of the peritoneal surface area of intra-abdominal organs and simultaneously explore them. It also facilitates biopsy, the taking of cultures and even the assessment of deep areas of abdominal organs, which are not usually explored, to make expedited diagnoses, establish protocols, take decisions and consequent actions, with the provision of therapeutic intervention as a possible option.
Whilst performing systematic examination of the whole peritoneal cavity, in all laparoscopic surgeries performed, it is sometimes possible to find completely unexpected changes related to an unidentified disease. Our surgical team therefore recommends that when a laparoscopy is performed, the entire peritoneal cavity be systematically revised so that differential diagnoses and unidentified diseases may acknowledged.
In our clinical case study, the laparoscopic approach of the multidisciplinary surgical team was able to establish a completely unexpected diagnosis, within the context of an emergency patient situation, of neuroendocrine small-cell carcinoma of the gallbladder, thanks to the systematic revision of the entire abdominal cavity.
Neuroendocrine small-cell carcinoma of the gallbladder. ReviewGallbladder cancer includes: cholangiocarcinoma, cancer of the ampullar of Vater and gallbladder cancer. Gallbladder cancer ranks fifth among ongological diseases which affect the gastrointestinal tract but worldwide it is the most frequent tumour of the bile ducts. It is generally diagnosed following a cholescystectomy and is considered to be of poor prognosis.1 It has been estimated that the percentage of patients diagnosed with cancer of the gallbladder, after a cholecystectomy for suggested lithiasic cholescystopathy is 0.5–1.5%. The main histological finding is adenocarcinoma in 80–85% of gallbladder carcinomas, with several histological subtypes having been described: papillary, nodular and infiltrative. Less frequent histological types of gallbladder cancer have been referred to in the literature and these include: sarcoma, melanoma, lymphoma, carcinoid tumours and squamous cell cancer. Extrahepatic bile ducts are a rare site for presentation of extrapulmonary neuroendocrine carcinomas. Primary neuroendocrine tumours of the gallbladder are particularly rare, and only 278 cases were reported between 1975 and 2005 in the Surveillance, Epidemiology, and End Results Program (SEER) of the American National Cancer Institute. These represent 0.5% of all neuroendocrine tumours.2,3 Poorly differentiated neuroendocrine small-cell carcinoma of the gallbladder, described in 1984 by Dr. Albores Saavedra et al.,4 is a rare neoplasm belonging to the carcinoid tumours group,4,5 with 54 cases having been described in the worldwide literature. This histological ancestry is associated with an extremely precarious prognosis.6
The incidence of gallbladder cancer increases with age and is frequently diagnosed in patients over seventy. Mean age is between 62 and 66 years of age.7 It predominantly presents in females, with the exception of endocrine carcinomas which present more frequently in males and at an earlier age.8 Gallbladder cancer is generally found within the context of chronic inflammation. In the majority of patients this inflammation is explained by the presence of cholesterol gallstones. The mere presence of intravesical lithiasis increases the risk of gallbladder cancer between 4 and 5 times.9 Other unusual causes of chronic inflammation of the gallbladder are: infections, such as trematodes (Fasciola hepatica, Clonorchis sinensis), chronic infections from Helicobacter pylori, Salmonella typhi and paratyphi, and autoimmune conditions such as ulcerative colitis and primary sclerosing cholangitis.10–12
Occupational risk factors are present, as is the case of employees in paper factories, the petroleum industry, textile industry and footwear sector. The gallbladder is also at risk from employment in the porcelain industry; when gallstones over 1cm are present; from obesity; from drugs such as: isoniazid, oral birth control drugs and a-methyodopa; from the consumption of water contaminated with organic pesticides and from exposure to certain chemicals such as pesticides, cork, vinyl chloride, heavy metals and radiation.13,14
Aetiology in neuroendocrine tumours is unclear. Several hypotheses exist regarding the origin of neuroendocrine tumours of the gallbladder. The first establishes that the normal gallbladder mucosa does not contain neuroendocrine cells, that neuroendocrine tumours only appear in the gallbladder mucosa with intestinal or gastric metaplasia, and that the metaplasia is secondary to choleliathiasis and chronic cholecystitis.3 The second establishes that it is also possible for neuroendocrine tumours to appear in ectopic pancreatic tissue, in heterotopic pancreatic tissues in the gallbladder, which is an extremely rare condition. The cells of the diffuse neuroendocrine system are embryological in origin, common in the neural crest (neuroectoderm); they are able to produce hormones and active peptides, many of which are active in a local environment, and which have no systemic influence. These cells are of particular metabolic characteristics, due to their affinity for the uptake and decarboxylation of amine precursors, for which they are named amine precursor uptake descarboxilase (APUD).15 They are located in several organs of the body, although respiratory tract and gastrointestinal cells (enteroendocrine and enterochromaffin cells) are particularly relevant due to their functional importance. The latter are especially concentrated in the stomach and small intestine. They also exist in the lower oesophagus, larger intestine, bile duct and pancreas.16 When they are found in a different site these cells may present, from an anatomopathological viewpoint, as hyperplasias, adenomatose hyperplasias, adenomas or carcinomas (APUDOMAS). This is the case of pheochromocytomas, paragangliomas and gastrinomas. All neuroendocrine tumours are potentially malignant. The neuroendocrine tumour group includes: those which are well differentiated (standard carcinoid tumours); well differentiated neuroendocrine carcinomas which are standard carcinoid tumours, well differentiated neuroendocrine carcinomas which are atypical or malignant carcinoids; poorly differentiated neuroendocrine carcinomas which are high grade carcinomas of small and large cells and the mixed endocrine-exocrine carcinomas.
Histologically neuroendocrine extrahepatic tumours represent 0.2% of the total, compared with 80–90% of adenocarcinomas. The most standard shapes are: papillary, nodular and tubular with unique implications in prognosis.17,18 Diagnosis of neuroendocrine carcinoma is dependent upon malignant epithelial elements including: atypias, mytosis or pleomorphic nuclei.19 Signs of dysplasia or adenocarcinoma in situ may be associated with neuroendocrine cancer.
The most sensitive immunohistochemical markers of small-cell gallbladder carcinoma are specific neuronal enolase which express 75% of carcinomas, synaptophysine and chromogranine A. Moreover, the serotonine or aderenocorticotropic hormone may on occasion be present. Neuroendocrine neoplasms of the gallbladder have atypical morphological features and are sensitive to chemotherapy.7 Clinically, gallbladder tumour symptoms are similar to those of biliary colic; they may present as a more general abdominal, persistent pain than the standard pain in the right hypochrondrium of gallbladder liathiasis, Jaundice, anorexia and weight loss generally indicate a more advanced stage of the disease. A physical examination may reveal: jaundice, palpable mass in right hypchrondrium with Courvoisier sign, periumbilical lymphadenopathy (Sister Mary Joseph nodule) or left supraclavicular adenopathy called Virchow nodule.
Preoperative diagnosis of neuroendocrine carcinomas of the gallbladder is extremely difficult due to the fact that symptoms are nonspecific and may include pain or discomfort at right hypochrondrium level and weight loss. The presence of the carcinoid syndrome is rare and the majority of tumours are incidentally identified when laparoscopic cholecystectomy is performed for lithiasic cholecystopathy. In laboratory testing, the CA 19–9 tumour marker may be found to be high in cholangiocarcinoma and in gallbladder cancer. Tests for liver function, alkaline phosphatise and bilirrubins are often found to be high. On occasions patients suffer from anaemia, in cases with chronic disease or in patients with more advanced stages of the disease. It is known that measuring of Chromogranine A is useful for preoperative diagnosis of neuroendocrine tumours. Chromogranine A is raised in 90% of neuroendocrine tumours of the intestine and the levels are correlated to the tumour load and the possibility of recurrence and, therefore, Chromogranine A may be an effective biological marker for preoperative diagnosis of neuroendocrine tumours. Preoperative chromogranine testing for neuroendocrine tumours of the gallbladder is not cost-effective.20
Ultrasound imaging is the diagnostic tool of choice in patients with pain in the right quadrant, since in 50–75% of patients with gallbladder cancer a mass is located here. It is also useful to determine whether metastasis of the liver has occurred. Computed tomography may show how the tumour has spread onto the edges of the gallbladder and liver metastasis presents in 60% of patients. Magnetic resonance is useful for assessing metastasis, gallbladder invasion and for precision definition of how far the tumour has spread, together with whether there is any regional lymph node invasion. For gallbladder tumours abdominal ultrasound imaging may be used for diagnosis. CAT scanning, PET scanning and MRCP can determine tumour stage and spread. Endoscopic biopsy is mostly used for bile duct endocrine tumours because it facilitates staging, follow-up and diagnosis which is important for establishing the chemotherapy regimen and proposing adjuvant therapies, such as somostostatin analogues.
Cholecystectomy is the only treatment to offer a cure for this disease, provided that there is no local invasion or metastasis. Unfortunately the majority of patients are diagnosed in advanced stages. The neoplasms which also present metastases to nodes outside of the regional area (portal vein, gastrohepatic ligament and retroduodenal area) are not resectable. If the patient may be referred for tumour resection, the procedure must include cholescystectomy, hepatic resection and regional lymphadenectomy. The extension of hepatic resection at present is undefined. However, 25% of T2 tumours involve the liver, with poor prognosis of the latter.21 For bile duct endocrine tumours, complete resection is the treatment of choice and this will depend on location. They are frequently unresectable with metastases or vascular compromise. The most frequent operation is extra hepatic bile duct resection with hepatic and jejunum anatomosis, pancreaticduodenectomy or cholecystectomy, with possible need for hepatic resection or transplant.22,23 According to Moskal et al.24 the sites where the nuroendocrine carcinoma of the gallbladder most frequently metastasise are the lymph nodes (88%), liver (88%), lung (23%) and peritoneum (19%).
The role of chemo and radiotherapy in the treatment of small-cell neuroendocrine tumours of the gallbladder remains unclear. In general, this type of tumour is insensitive to standard radiotherapy. Chemotherapy agents used in several published case series include: cisplatin, gemcitabine and etoposide in addition to 5-fluorouracil which, according to the published studies, may lead to a partially palliative outcome with little marginal advantage.25,26
ConclusionOur surgical group advised that by introducing the laparoscope, the entire peritoneal cavity must be systematically reviewed, in search of differential diagnoses and unidentified pathologies. We must always use the explorative, diagnostic and therapeutic qualities of laparoscopy.
Bile duct endocrine tumours tend to remain silent until they metastasise or invade neighbouring organs, and diagnosis at initial stages is therefore infrequent due to low incidence, absence of serum markers and lack of hormonal symptoms.
Prognosis is unfavourable, especially when they are unresectable. Endocrine neoplasias of the gallbladder, although uncommon, should be taken into account as a possible diagnosis due to therapeutic and prognostic implications. In our case, it was thanks to routine diagnostic laparoscopy performed by the surgical team involved that a disease was detected which, had this not been the case, would have gone unnoticed and further worsened the patient's prognosis. As a result, we consider that diagnostic laparoscopy should be performed in all laparoscopic procedures, regardless of referral.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThere was no conflict of real, potential or potentially perceived interests which could result in a bias in the publication of this study.
Please cite this article as: González-Chávez MA, Villegas-Tovar E, González Hermosillo-Cornejo D, Gutierrez-Ocampo A, López-Rangel JA, Athié-Athié AJ. Carcinoma neuroendocrino de células pequeñas de vesícula biliar. Un hallazgo inesperado con el uso de laparoscopia diagnóstica. Cir Cir. 2017;85:168–174.