Failed back surgery syndrome is a complication of spine surgery that leads to chronic pain and disability, often with disastrous emotional consequences to the patient.
AimTo compare the profile of patients whose first surgery was performed in our hospital versus a group that underwent first spine surgery in a different centre.
Materials and methodsRetrospective study with 65 patients; 18 formed group I (first spine surgery performed in our institution), and 47 patients in group II (first surgery performed in another hospital). Background, demographic, clinical features and functional status were compared. In group I the majority of the cases had a previous diagnosis of lumbar stenosis (group I 44.4% vs. group II 25.5% p=0.22), whereas disk herniation was the main diagnosis in group II (group I 22.2% vs. group II 61.7% p=0.001). The main cause of the syndrome in group I was technical error during surgery (61.1%), while in group II this cause represented only 6.3% (p=0.001). Among the patients of this latter group, misdiagnosis was highly prevalent (57.4%), against no cases in group I (p=0.001). The preoperative functional status between both groups and their recovery in the immediate postoperative period was similar (p=0.68).
ConclusionsThis study suggests that the diagnostic and treatment standards are different between healthcare centres, specifically between academic centres vs. private practice.
El síndrome de columna multioperada es una complicación de la cirugía de columna vertebral lumbar que resulta en dolor crónico y discapacidad, y tiene consecuencias emocionales para el paciente.
ObjetivoComparar el perfil de pacientes con síndrome de columna multioperada cuya primera cirugía se realizó en nuestro hospital, contra otro grupo operados por primera vez en otros centros.
Material y métodosEstudio retrospectivo de 65 sujetos; 18 conformaron el grupoI (inicialmente operados en nuestra institución) y 47 pacientes el grupoII (operados en otro hospital). Se comparó su perfil demográfico, antecedentes, características clínicas y estado funcional. En el grupoI la mayoría de los casos fueron diagnosticados como estenosis lumbar (grupoI 44.4% vs. grupoII 25.5%; p=0.22), mientras que el diagnóstico de hernia discal fue el principal en el grupoII (grupoI 22.2% vs. grupo II 61.7%; p=0.001). La principal causa del síndrome en el grupoI fue el error técnico (61.1%), mientras que para el grupoII esta etiología solo estuvo presente en el 6.3% (p=0.001). En este último grupo la principal causa fue el error diagnóstico (57.4%), contra ningún caso en el grupo de pacientes operados primariamente en nuestro hospital (p=0.001). El estado funcional preoperatorio entre los grupos y su recuperación en el periodo postoperatorio inmediato fue similar (p=0.68).
ConclusionesEste estudio sugiere que las prácticas diagnósticas y terapéuticas difieren entre los centros hospitalarios, pero especialmente entre centros académicos respecto al medio privado.
Failed back surgery syndrome is defined as lumbar or radicular pain persisting after one or more surgeries performed to treat some alteration to the lumbar spine (disc, narrowing of the lumbar canal, tumour, etc.). It is also known as post-laminectomy syndrome or FBS (Failed Back Syndrome).1–5
The development of minimally invasive procedures, such as chemical nucleolysis, automated percutaneous discectomy, radiofrequency percutaneous nucleoplasty, electro-thermal and laser disc ablation, have failed in their attempt to preserve the spine's function and structure; furthermore, a higher proportion of long term reoperations has been proven. The continued search for new techniques is due to its complexity and unsatisfactory results.6
The consequence of a disc surgery must be acknowledged as a structural and functional damage, for instance, out of 2353 patients subject to a microdiscectomy procedure, 100% presented decreases of more than 30% of disc height in the postoperative stage. This means that the disc surgery, as minimal as it is, always changes the structure and, therefore, the stability of the operated segment.7 The success of this surgery varies, ranging from 60 to 90% in the medical bibliography; the remaining proportion constitutes the so-called failed back surgery syndrome.8
There is evidence that psychosocial factors may have a significant influence in the perception of pain and pain chronicity, which may explain the reason why lumbar surgery may not be successful, even when morphological problems have disappeared after a surgical intervention.9–13
It has been published that the percentage of reoperations after the first lumbar surgery varies from 5 to 18% in conventional surgeries, and reaches 30% in percutaneous surgeries,14–17 with poor results in these cases as regards the decrease of pain and functional improvement, with reinstatement to the same work position varying from 65 to 98%.14–16
In the United States of America, 250,000 cases are operated annually, and out of those, 37,500 (6.6%) require surgical reintervention.18 This figure varies, since in percutaneous discectomy reoperation is more likely.19
In the definition of the syndrome, an iatrogenic aetiology attributable to a diagnostic error, surgical technique error or bad indication of surgery is recognised.1,2 Additionally, almost 50% of patients with failed back surgery syndrome have shown psychological alterations, which had not been identified before the surgery.20
Although failed back surgery syndrome is well known and even feared by spine surgeons, it is hard to understand it integrally, because it has multiple factors. A proper diagnosis is essential, selecting the proper patient to operate, selecting and performing the best customised surgical treatment.21,22 In Table 1, we can see the predictive factors of revision surgery results in failed back surgery syndrome cases.23
Predictive factors in the prognosis of lumbar spinal surgery.
| Favourable factors | Unfavourable factors |
|---|---|
| More than 6 months of improvement after the previous surgery | Less than 6 months of improvement after the previous surgery |
| Radicular pain more severe than lumbar or thoracic pain | Presence of fibrosis in the previous surgery |
| Radicular compression from the disc or bone | Radiology with evidence of arachnoiditis |
| Correlation between clinical signs and contrast techniques | Poor psychological profile |
| Neurological deficit | Labour or compensatory litigation proceeding |
| No labour or compensatory proceeding | Multiple prior operations |
| Prior abuse of toxic substances or medication |
In our area, the work with the clearest approach to the subject of failed back surgery syndrome was published in 2007. That study included 20 subjects (16 women and 4 men, with an average age of 53.2 years) where 40% had a previous surgery, 40% had two, 15% had three and 5% had four. The assessment with the Oswestry scale showed that during the preoperative stage 60% of patients had severe disability, and 2 years after 55% of all patients remained with a mild incapacity. Despite the persistent symptomatology in almost all patients and complications, the satisfaction index was 100%. Upon evaluation of the cases, it was discovered that the main causes for failed back surgery syndrome were a bad surgical indication+technical error (50%), error in the surgical technique (35%) and error in the indication (15%).24,25
ObjectiveIdentify the causes for failed back surgery syndrome in our population and compare the profile of patients with this disease both for patients with the first surgery performed at a well-known academic centre vs. a group of patients operated for the first time at other hospital centres.
Material and methodsRetrospective, observational, comparative study. Inclusion criteria: subjects more than 18 years of age, men and women, admitted from 1st January 2005 to 31st December 2011 into the Spinal Surgery Service of the National Rehabilitation Institute with diagnosis of failed back surgery syndrome, confirmed through clinical data of lumbar pain and/or persistent radicular alteration, after one or more lumbar surgeries carried out for the purposes of treating some type of alteration such as disc herniation, narrowing of the lumbar canal, tumour, etc. Radiographical data: X-ray studies, magnetic resonance and electromiography prior to the first lumbar surgery to confirm the initial diagnosis, as well as radiographic studies upon consultation at our institute to verify the current status of the patient, operated at this and other hospitals in the country.
A sample size was calculated taking into consideration the total of spinal surgeries performed per year in the service, the estimated prevalence at the institution of the diagnosis of failed back surgery syndrome (4.8%), 5% maximum error, and 95% reliability; resulting in 62 patients.
The diagnosis upon admission and discharge of the institution was verified, as well as the diagnosis of an expert spine surgeon to avoid duplication of files. Files of patients with revision surgery due to superficial infection of surgical wound with no lumber or radicular pain were excluded. Incomplete files were eliminated. The information was gathered from automated databases and electronic files of the National Rehabilitation Institute (Instituto Nacional de Rehabilitación) and the Spinal Surgery Service.
To evaluate diagnosis error in patients at our institution and other institutions (private or public) each of the cases was sent to an academic session. The panel of experts consisted of 4 experienced spinal surgeons (3 of them with academic background in orthopaedics and one of them in neurosurgery) and one experienced neuroradiologist. Clinical histories were analysed, as well as X-ray studies, magnetic resonance and electromiography of each patient before the first surgical intervention and recent analyses, all with measurements of the relevant parameters for narrowing of lumbar canal, spondylolisthesis, instability, and the nomenclature and classification of lumbar disc pathology of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology19 were used.
The sample consisted of 65 individuals, categorised as follows: group I consisted of 18 subjects operated initially at our hospital and group II consisted of 47 subjects who had their first surgery at another institution.
The analysed variables were: age, gender, diagnosis prior to the first surgery, cause of the failed back surgery syndrome (diagnosis error, transoperative error, technical error, bad application or bad indication), functionality according to the Oswestry scale and evolution period.
A descriptive statistic was performed with an analysis of data distribution. A non-parametric statistic with tests for χ2 to contrast categorical variables was performed. For data with normal distribution, a parametric statistic was performed using the Student's t test to compare the means of continued variables. For data with abnormal distribution, the non-parametric Mann–Whitney U-test was applied. The statistical analysis was carried out using the SPSS® programme, version 15.0 (SPPS Inc., Chicago, IL). A p≤0.05 value was considered statistically significant.
ResultsGroup I consisted of 18 overweight subjects (7 men and 11 women; age, 54±9.4 years) (BMI 29.9±4.5), and group ii consisted of 47 obese subjects (21 men and 26 women; 58±11.2 years) (BMI 32.9±6.3), most (66%) from the private sector (Fig. 1). The epidemiological and morphological features of both groups did not show statistically significant differences (Table 2). In group I, the main diagnoses were lumbar stenosis (44.4%), discal herniation (22.2%) and spondylolisthesis (16.7%), while in group II the main diagnoses were disc herniation (61.7%), lumbar stenosis (25.5%) and spondylolisthesis (8.5%) (Table 2). The difference in the frequencies of the diagnosis of disc herniation among the groups was significant (p=0.001).
Differences in the epidemiological, morphological and clinical profile among groups.
| Variable | Group I | Group II | p |
|---|---|---|---|
| Male/female | 7/11 | 21/26 | 0.88 |
| Age | 54±9.4 | 58±11.2 | 0.18 |
| BMI | 29.9±4.5 | 32.9±6.3 | 0.21 |
| Disc herniationb | 4 (22.2%) | 29 (61.7%) | 0.00a |
| Lumbar stenosisb | 8 (44.4%) | 12 (25.5%) | 0.22 |
| Spondylolisthesisb | 3 (16.7%) | 4 (8.5%) | 0.38 |
| Othersb | 3 (16.7%) | 2 (4.2%) | 0.12 |
BMI: Body mass index.
The time elapsed between the first surgery and the final surgery in group I was 1.2 years±2.9 and in group II it was 4.3 years±8.6 (p=0.14). Regarding the number of surgeries, in group I they were 2.3±2.9, and in group II, 3.5±5.6 (p=0.39).
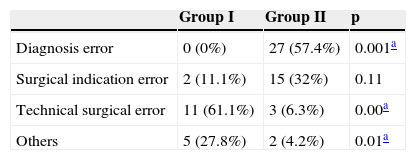
The main cause of failed back surgery syndrome in group I was technical error (61.1%), while for group II this aetiology was only present in 6.3% (p=0.001). In turn, in this last group the main cause was diagnosis error (57.4%), against no cases in the group of patients operated mainly at the National Rehabilitation Institute (p=0.001). The rest of aetiologies among groups are observed in Table 3.
Causes for failed back surgery syndrome among groups.
| Group I | Group II | p | |
|---|---|---|---|
| Diagnosis error | 0 (0%) | 27 (57.4%) | 0.001a |
| Surgical indication error | 2 (11.1%) | 15 (32%) | 0.11 |
| Technical surgical error | 11 (61.1%) | 3 (6.3%) | 0.00a |
| Others | 5 (27.8%) | 2 (4.2%) | 0.01a |
Error in the technical execution of the surgery was the main cause in group I, while error in diagnosis was the main cause in group II, both with statistically significant differences.
All patients presented high degrees of functional condition in the preoperative stage shown in Table 4, and both groups equally showed a significant improvement in the immediate postsurgical period (p=0.68).
Behaviour of the functional state before and after the final surgery among groups.
| Degree of disability (Oswestry) | Group I | Group II | ||
|---|---|---|---|---|
| Pre-surgical | Post-surgical | Pre-surgical | Post-surgical | |
| Minimum (0–20) | 0 | 11 (62%) | 0 | 35 (75%) |
| Moderate (21–40) | 7 (39%) | 6 (33%) | 0 | 10 (21%) |
| Severe (41–60) | 0 | 1 (5%) | 21 (45%) | 2 (4%) |
| Totally disabled (61–80) | 10 (56%) | 0 | 23 (49%) | 0 |
| Oswestry 80–100 | 1 (5%) | 0 | 3 (6%) | 0 |
Shows the severity of pre-surgical functional affectation in both groups, as well as its improvement in the post-surgical period immediately after the final surgery.
The most frequent complication during the final surgery was dural injury, with a frequency of 7 (38.8%) in group I and 21 (43.7%) in group II (p=0.78).
DiscussionThis study was carried out in a high speciality institution of the health sector, providing its services to the population without some kind of social security coverage. The aim is to report the clinical and epidemiological profile of patients with failed back surgery syndrome attending our spinal surgery academic centre.
We found 2 reports similar to ours, from 2002 in the United States of America, where the demographic profile of 180 patients was gathered from clinical files in one same institution, and another where a series of 267 files were reviewed in a multicentre study.17,18
Our population distribution differs from previous studies, with a predominance of female patients as compared to the male population reported. We found a high percentage of patients whose first lumbar surgery was performed at a private hospital. According to this finding we tried to elucidate the aetiology of this syndrome. The bibliography identifies an average age of 51.6 years, similar to our report of 54 years in group I and 58 years in group II. Group I consisted of overweight patients, while group II consisted mostly of obese patients. Gepstein et al.13 reported that the percentage of patients with “very low satisfaction” is significantly higher in obese patients, and that the increase in the body mass index has a negative impact in the perception of pain (more pain) and upon resuming daily activities after a spinal surgery. Furthermore, it has been reported that obesity also increases the risk of developing musculoskeletal pain and bad functional results after a spinal surgery. It is known that the relation between morbidity associated to obesity and health costs is a relevant public health problem.7
Taking into consideration the most common preoperative diagnosis, we observe that patients initially assisted at an academic institution were documented as narrow lumbar canal (44.4%), disc herniation (22.2%) and spondylolisthesis (16.7%), different to what was reported by Slipman et al.18 who stated that stenosis stands for 21.5% of its population, disc injuries 21.5% and spondylolisthesis 1.6%. However, patients whose first surgery was performed at other institutions, predominantly private, had a diagnosis of stenosis (25.5%), disc herniation (61.7%) and spondylolisthesis (8.5%). It is known that the most frequent aetiology of failed back surgery syndrome includes diagnosis error, undiagnosed injuries, surgical indication error, surgery technical error (transurgical incidents or bad surgical technique).9,11,12 In our study we found that there was over-indication of surgical treatment for disc herniation. Upon review of the cases and previous studies in a professional session, we noted there is a frequent confusion between disc bulging and true disc herniation leading to radicular compromise, which we may consider as a diagnosis error.26
90% of causes of failed back syndrome in our study were due to surgical indications for disc herniation, with clear radiological evidence that no surgical treatment was required or without proper conservative treatment. As established by international bibliography, except for true emergencies, such as the cauda equina syndrome, the surgical treatment for lumbar disc herniation and symptomatic stenosis is an elective procedure following an established period of conservative treatment. It is known that a large number of patients will only improve with conservative treatment; as proved by the data of the Maine Lumbar Spine Study, which showed good results, sustained over time, on the long term after non-surgical treatment of this type of patients in a non-randomised prospective cohort study.4,20–22
In our study, 57% of cases were associated to diagnosis error and 33% to surgical indication error. In cases diagnosed as narrow lumbar canal or lumbar stenosis, procedures such as laminectomy+discectomy were the most used to relieve the symptoms of pain irradiated to pelvic limbs, numbness and weakness associated to the compression of neural structures. However, in some cases this type of decompression may compromise the structure of mobile segments of the spine and lead to more degeneration, abnormal or excessive movement, instability and deformity.26 In these cases not only proper decompression but also stabilisation of the segment shall be considered part of the surgical prescription.
A clear difference was found in the number of surgeries performed before the final surgery to treat this syndrome and the average of prior surgeries was 1.5 in patients operated at the academic institution, as compared to those operated at other institutions, who reported up to 8 prior surgeries. Slipman et al.18 reported an average of 1.6 prior surgeries, with limits of 1–6.
The presence of accidents or incidents during surgery (with proper diagnosis and surgical indication) is attributed to technical incidents. Incidental durotomy is a relatively common incident in lumbar surgery, with a reported incidence from 1 to 16%. The rate of complications in microscopic lumbar surgery varies from 1.5 to 15.8%.23–26 The age, diagnosis of a degenerative condition, prior lumbosacral surgery, highly invasive surgery or revision surgery are the most significant risk factors for this type of complication. In our spinal surgery service, > 500 surgeries were performed per year; out of those, 300 are for lumbar disc herniation or narrow lumbar canal diagnosis. We reported 1% of cases of error due to technical incident. We suggest this may be due to the study protocol and standardised treatment of the institution: (a) the clear position of offering conservative treatment first, with medication and rehabilitation for at least 3 months prior to surgery; (b) never offering the surgical option as an emergency treatment, except in the event of a true emergency, and (c) proper choice of patients (clinical and imaging) as well as strict surgical indication to perform minimally invasive procedures. It has been reported in the international bibliography that the frequency of poor results after lumbar surgeries decreases to 66% when performed at spinal surgery academic services, compared to the national average reported in some countries.18 The satisfactory functional results measured through significant changes in the Oswestry scale were evident in both groups.
When a new surgery has to be performed, the favourable and unfavourable factors related to the patient must be evaluated (Table 1).24 For instance, a patient with no clinical improvement during the last 6 months and who is going through litigation proceeding or secondary compensation at work is not the ideal candidate for a revision surgery, unless there is clear evidence of anatomical and structural causes leading to pain and disability in the site of the previous surgery; however, other causes, such as diagnoses with non-surgical treatment, non-organic causes for the lumbar pain and psychological factors, shall be taken into consideration.18,27 There is evidence that psychosocial factors have a significant influence on the perception of pain and pain chronicity. This may explain why lumbar surgery may not be successful even when there are no longer morphological problems after the surgery. For surgery to treat disc pathology, the success rate is high (> 80%) in patients with no complications, no related psychological factors and proper management of premorbid personality. It is important to note that countries with 100% coverage report the highest rates of disability due to failed back surgery.9,23,27–30 Several studies show the relation between litigation/compensation and high disability rates or high levels of post-treatment pain not related to medical or surgical treatment.18
Finally, it is not surprising to observe that > 50% of patients in our study come from private institutions where there is minor consensus on surgical indications and diagnoses than in third level institutes, where there are medical practice guidelines and standardised procedures in spinal surgery services; furthermore, the prescription and surgical planning rest, sometimes, on one surgeon only.
We identified 2 important limitations in this study. The first one is the risk of bias resulting from a retrospective study and based on the information of a third level institution, with the related sub-recording of complicated cases within the same centre. The second is that we had no psychological advisors as well as confirmation or dismissal of the patient's involvement in a litigation procedure for us to analyse these variables as an impact factor to identify more cases of failed back surgery syndrome in patients assisted in the private sector. We are currently working on a study design allowing for better control of these variables.
ConclusionThe impact of failed back surgery syndrome on individuals’ quality of life, as well as its economic and social impact, are considerable and even more incapacitating than other causes of chronic pain or other chronic medical conditions (neoplasias, diabetes, etc.).6,10 These findings emphasise the need to generate strategies to prevent the syndrome. This analysis of the most frequent causes for failed back surgery syndrome in relation to 2 different ways of studying and dealing with the patient may serve as an orientation to understand the clinical efficiency that may be attributed to the discussion of column cases as a team to decrease and/or prevent failed back surgery syndrome.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Romero-Vargas S, Obil-Chavarria C, Zárate-Kalfopolus B, Rosales-Olivares LM, Alpizar-Aguirre A, Reyes-Sánchez AA. Perfil del paciente con síndrome de columna multioperada en el Instituto Nacional de Rehabilitación. Análisis comparativo. Cir Cir. 2015; 83: 117–123.