Catecholamine-producing tumors are uncommon and called pheochromocytomas when their origin is intra-adrenal and paragangliomas when they are extra-adrenal.1 The symptoms of pheochromocytoma include maintained or paroxysmal hypertension, headaches, palpitations and sweating. However, its symptoms can vary greatly, which is why it has been called “the great simulator”.1 Pheochromocytoma is rarely a cause of peripheral ischemia, but when this occurs it can lead to necrosis or gangrene, due in most cases to extreme vasoconstriction or diffuse arterial vasospasms induced by hypercatecholaminemia.1–10 This vasospasm induced by catecholamines can easily be overlooked if the patient does not present other symptoms characteristic of pheochromocytoma; some patients may even have a history of intermittent claudication, a situation that can hinder and delay diagnosis.1–10
We report the case of a patient with a pheochromocytoma that presented multiple clinical manifestations and severe ischemic involvement of both the upper and lower limbs.
The patient is a 76-year-old woman with a history of hypertension under treatment for many years, ischemic stroke 20 years earlier with recovery and minimal sequelae, and gastric surgery for a bleeding ulcer 10 years ago. In the emergency room, she reported persistent intense headache for the previous 5 days associated with dizziness, nausea and vomiting. At this time, she was diagnosed with a hypertensive crisis, which subsided with medical treatment. She returned 24h later and reported the same symptoms as before, in addition to epigastralgia radiating toward the thorax and diaphoresis. Upon examination, blood pressure was 185/90mmHg, electrocardiogram showed a decrease in ST and negative T waves, and lab work-up detected elevated myocardial ischemia enzymes, so the patient was diagnosed with hypertensive crisis and acute coronary syndrome. 36h after admission, the patient presented neurological deterioration with a Glasgow index of 12 and subsequent acute renal failure and respiratory failure, so she was transferred to the intensive care unit and intubated. Abdominal computed tomography (CT) scan showed a right adrenal mass measuring 8cm in diameter; urine analysis demonstrated increased catecholamines (metanephrine 857μg/24h [Nr: 60–350]; noradrenaline 99μg/24h [Nr: 12–86]; adrenaline 45μg/24h [Nr: 2–23]). Blood pressure was controlled with iv labetalol during the 24h of intubation, after which the treatment was changed to phenoxybenzamine and oral antihypertensive drugs. The patient presented an episode of atrial fibrillation that reverted to sinus rhythm with amiodarone. Renal failure and encephalopathy progressively improved.
During the hospital stay, the patient presented progressive acral ischemia of the 4 limbs, with necrosis of the fingers and toes (Fig. 1). Treatment was initiated with acetylsalicylic acid and perfusion of buflomedil. One month after admission to the hospital, right adrenalectomy was performed, initially by laparoscopy but then requiring conversion to subcostal laparotomy due adhesions caused by previous gastric surgery. The patient presented a favorable postoperative period, with progressive remission of the symptoms. The ischemic lesions of the 4 limbs became localized, and 53 days after admission, the patient required bilateral supramalleolar subcondylar amputation and metacarpophalangeal amputations of the fingers of both hands and interphalangeal amputations in the 2 thumbs. The patient recovered adequately. Vasculopathy and peripheral tissue ischemia are exceptional manifestations of pheochromocytoma and are due to the intense vasoconstriction of the cutaneous vessels in response to sympathetic overstimulation.1,2 Early diagnosis of these cases is important to avoid vasoconstrictive medication, which may worsen the distal ischemia of both the upper and lower extremities.3–8
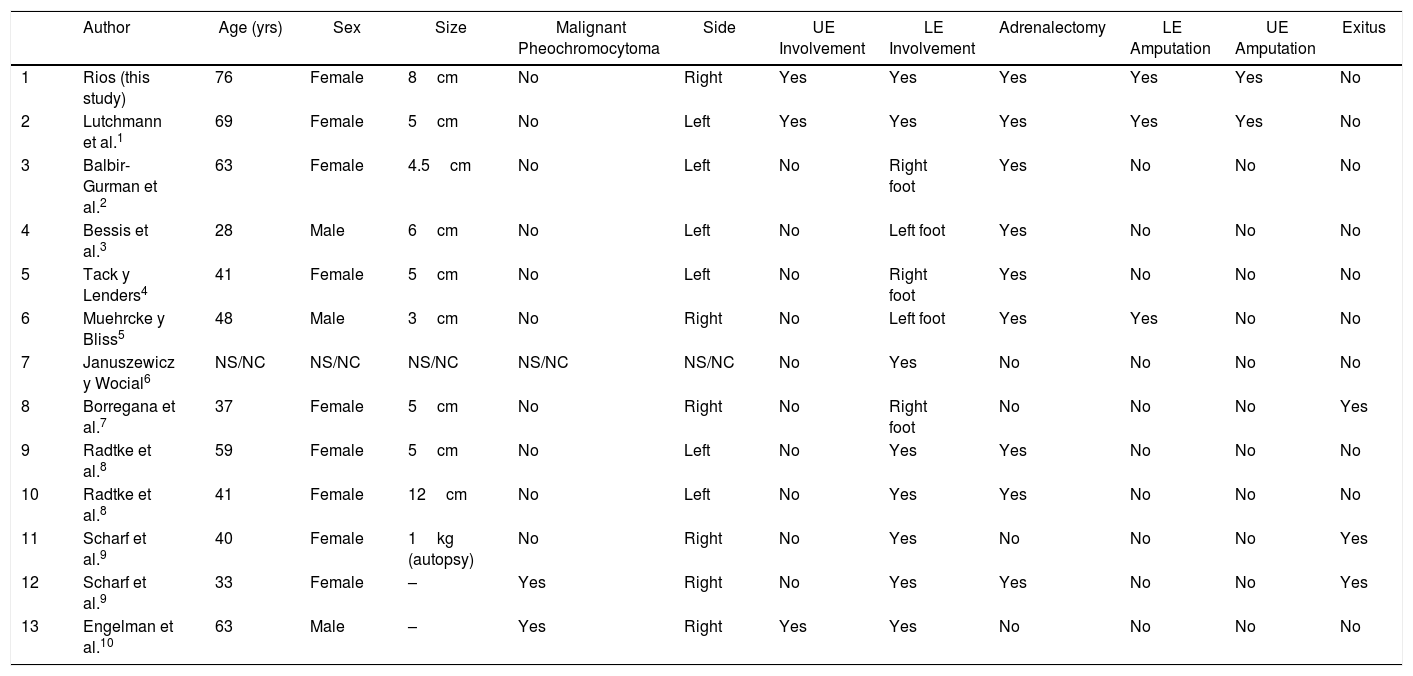
There is little experience worldwide in cases as dramatic as the one we present here, and fewer than 15 cases have been reported (Table 1). It is not a condition that exclusively affects older patients who present pheochromocytomas. Thus, almost half of case reports occur in patients under 45 years of age, as can be seen in Table 1. This indicates that it is more related with the production of catecholamines and the vasoconstrictor effect than the patient's baseline disease. It is observed that, in the majority of cases. acral ischemia mainly affects the lower limbs. However, in patients over the age of 60, it can also affect the upper limbs, as in our case.1–10 The treatment in all cases is adrenalectomy, which is usually performed laparoscopically. Regarding the treatment of distal acral ischemia, it should be as conservative as possible so that the patient maintains as much personal autonomy as possible.1–10 In conclusion, we can say that ischemia of distal acral areas, although rare, can occur in pheochromocytoma. Therefore, the diagnosis and early treatment of this disease is the way to avoid extensive amputations of the upper and lower limbs.
Cases of Pheochromocytomas With Distal Acral Involvement.
| Author | Age (yrs) | Sex | Size | Malignant Pheochromocytoma | Side | UE Involvement | LE Involvement | Adrenalectomy | LE Amputation | UE Amputation | Exitus | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Rios (this study) | 76 | Female | 8cm | No | Right | Yes | Yes | Yes | Yes | Yes | No |
| 2 | Lutchmann et al.1 | 69 | Female | 5cm | No | Left | Yes | Yes | Yes | Yes | Yes | No |
| 3 | Balbir-Gurman et al.2 | 63 | Female | 4.5cm | No | Left | No | Right foot | Yes | No | No | No |
| 4 | Bessis et al.3 | 28 | Male | 6cm | No | Left | No | Left foot | Yes | No | No | No |
| 5 | Tack y Lenders4 | 41 | Female | 5cm | No | Left | No | Right foot | Yes | No | No | No |
| 6 | Muehrcke y Bliss5 | 48 | Male | 3cm | No | Right | No | Left foot | Yes | Yes | No | No |
| 7 | Januszewicz y Wocial6 | NS/NC | NS/NC | NS/NC | NS/NC | NS/NC | No | Yes | No | No | No | No |
| 8 | Borregana et al.7 | 37 | Female | 5cm | No | Right | No | Right foot | No | No | No | Yes |
| 9 | Radtke et al.8 | 59 | Female | 5cm | No | Left | No | Yes | Yes | No | No | No |
| 10 | Radtke et al.8 | 41 | Female | 12cm | No | Left | No | Yes | Yes | No | No | No |
| 11 | Scharf et al.9 | 40 | Female | 1kg (autopsy) | No | Right | No | Yes | No | No | No | Yes |
| 12 | Scharf et al.9 | 33 | Female | – | Yes | Right | No | Yes | Yes | No | No | Yes |
| 13 | Engelman et al.10 | 63 | Male | – | Yes | Right | Yes | Yes | No | No | No | No |
LE: lower extremity; UE: upper extremity.
Please cite this article as: Ríos A, Pinzón LF, Rodríguez JM, Parrilla P. Isquemia acral secundaria a feocromocitoma. Cir Esp. 2018;96:589–591.