We present the case report of an adult male patient who underwent laparoscopy for a suspected porcelain gallbladder, at which time hypoplasia of the gallbladder was found. The patient had been operated on after years of follow-up with suspicion of porcelain gallbladder based on tests that had been done previously. The indication for surgery was based on the presence of worsening cholestasis and the age of the patient as an attempt at a definitive solution for the pathology. We find the case to be interesting as this presentation is extremely rare in adults and is more typical of the first trimester of life, be it in its pure form or associated with hypogenesis of the bile duct. Furthermore, this case presented correct development of the cystic duct and artery, but there was absence of gallbladder development.
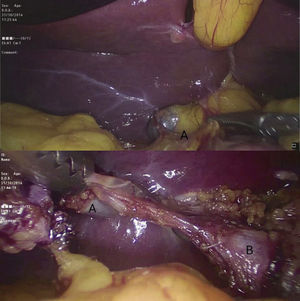
The patient is a 26-year-old male who was being followed-up in the outpatient setting for the previous 3 years due to mild intermittent hepatic colic, without requiring hospitalisation. Physical examination was normal at all times, but the lab work had shown a progressive deterioration of liver enzymes over the last year as well as a mild cholestatic pattern (alkaline phosphatase 187UI/L, total bilirubin 2.37mg/dL and gamma-glutamyl-transpeptidase 312UI/L). Given the evolution of the patient, we decided to extend the study with magnetic resonance cholangiopancreatography, which revealed a round image measuring 10mm located in the theoretical anatomic topography of the gallbladder that directly communicated with the common bile duct (Fig. 1). The image was compatible with porcelain gallbladder or gallbladder hypoplasia with lithiasis in its interior and no evidence of the cystic duct. Because of the worsening analytical parameters and intermittent symptoms, we decided on surgery. A conventional laparoscopic approach detected a hypoplastic gallbladder with lithiasis; the cystic duct and artery showed correct development and position (Fig. 2). The patient presented a favourable postoperative progress and was discharged 24h after the procedure. The histology study confirmed the existence of gallbladder hypoplasia (diameters 1cm×0.5cm) and presence of gallbladder sludge.
Intraoperative image showing the hypoplastic gallbladder (above, A) with no evidence of the gallbladder bed, as would be typical of porcelain gallbladder; the lower postoperative image shows (after dissection) the communication between the gallbladder (A) and the main bile duct (B), with the cystic duct and artery present.
Before the intervention, given the MRI findings, it was necessary to consider the differential diagnosis between gallbladder hypoplasia, type II (choledochal diverticulum) or type III (choledochocele) choledochal cyst1,2 and porcelain gallbladder, which is the diagnosis that was suspected from the start. In all these pathologies, symptoms can be similar and include intermittent pain in the right hypochondrium and a cholestatic pattern. In our patient, the diagnosis was reached intraoperatively when we observed the presence of a gallbladder that was miniscule in size and a cystic duct that communicated with the main bile duct, which definitively determined the diagnosis of gallbladder hypoplasia. Without surgical treatment, the progress of these patients usually presents progressive decline in liver function, which in turn leads to the development of difficult-to-manage liver disease. Therefore, surgical treatment is indicated as an initial therapeutic option, and laparoscopy is the treatment of choice.
The exceptional nature of this case lies in the low incidence of gallbladder hypoplasia3 and its presentation in an adult, as this disease usually initiates with symptoms and cholestasis in the first few months of life. In the literature, there are very few documented cases, most of which affect patients with cystic fibrosis4 or other more complex congenital alterations. Hypoplasia is less frequent than agenesis of the gallbladder and can be associated with other gallbladder malformations, such as multiseptate gallbladder,5–7 derived from an embryonic defect in the reabsorption of the tissue that occupies the gallbladder lumen during organogenesis. As in other congenital gallbladder alterations, it is usually diagnosed in children or young adults, although in some cases it may be an accidental discovery in older adults.
Conflict of InterestsThe authors have received no funding and have no conflict of interests regarding this study.
Please cite this article as: Gómez Contreras R, Roldán Villavicencio JI, Zaragoza Fernández C, Noguera Aguilar JF. Hipoplasia de vesícula biliar con cuadro colestásico como primera manifestación clínica. Cir Esp. 2016;94:242–243.