Hepatic steatosis is a common anomaly detected in imaging studies. There are highly prevalent forms such as diffuse hepatic steatosis and other less common ones like multinodular hepatic steatosis, which is a very uncommon condition that causes difficulty in the differential diagnosis.
We present the case of a patient with focal liver lesions that were suspected adenomas on radiology tests.
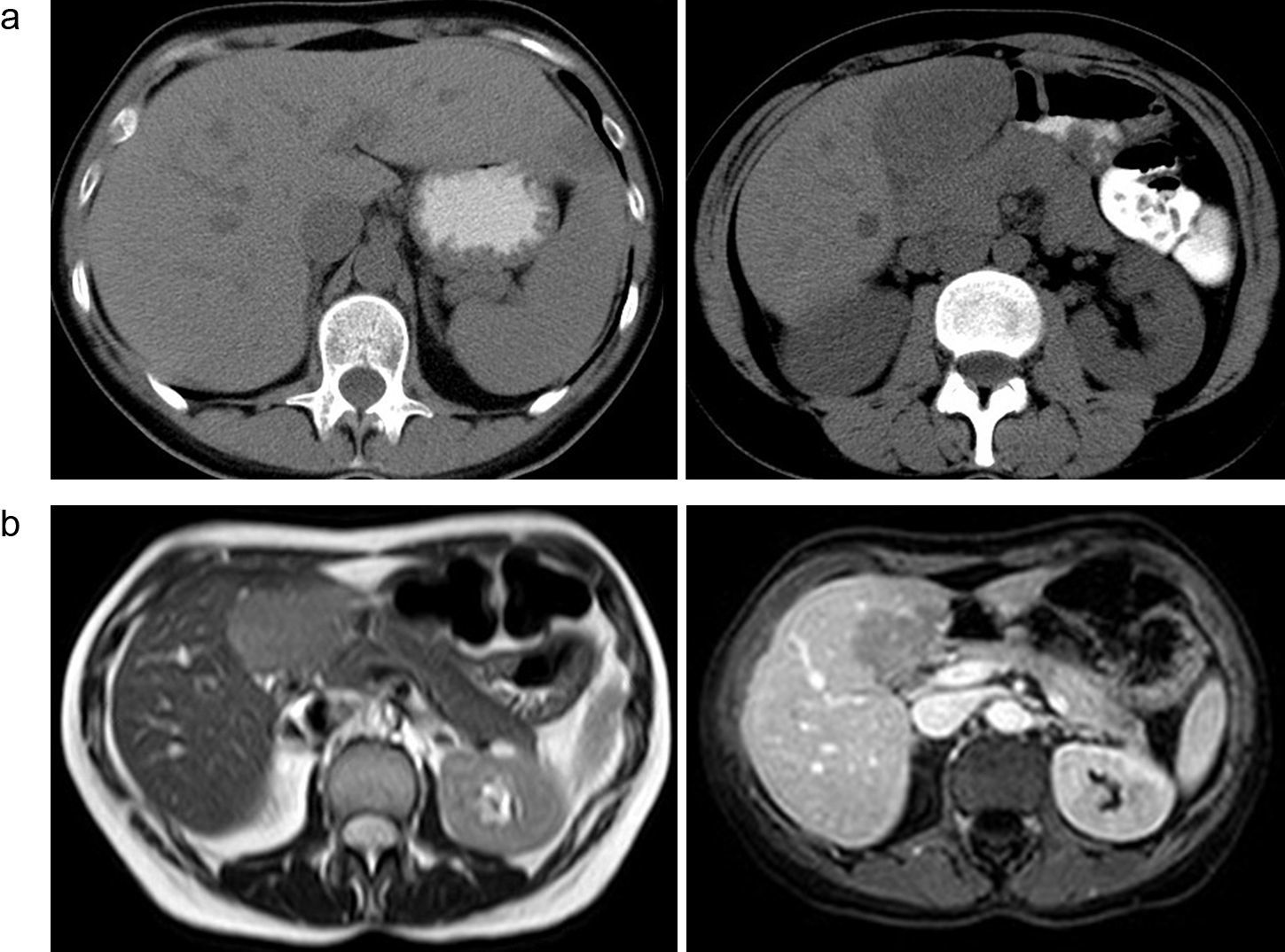
The patient is a 46-year-old woman with no medical-surgical history of interest and a body mass index within normal range who was referred to our department for hepatic lesions. The patient was asymptomatic and showed no alterations in the liver function tests, hemogram or increased acute-phase reactants. Abdominal computed tomography (CT) was ordered, which detected hepatomegaly and several space-occupying lesions (SOL) that were hypodense compared to the liver parenchyma and especially large: one measured 2.5cm in segment II, and another was 6cm in diameter and proximal to the caudate lobe (Fig. 1A). In the triphasic computed tomography (CT) scan, the 3 largest lesions presented progressive, homogenous enhancement in the late phase and contrast washout after 5min, which was also homogeneous. The diagnostic impression was hepatic adenomas. The study was complemented with an abdominal magnetic resonance (MRI) study that revealed 3 solid round liver lesions that were mildly hyperintense compared to the normal tissue in T2. During in-phase/opposed-phase imaging, they presented a drop in signal intensity (Fig. 1B). After the administration of intravenous contrast, the lesions showed slight peripheral enhancement.
(A) Hepatic tomography showing multiple hypodense focal lesions, two of which are especially large: one measuring 2.5cm in segment II and another measuring 6cm proximal to the caudate lobe; (B) Magnetic resonance showing mildly hyperintense liver lesions in the in-phase T1 sequence (a) and a notable loss of signal in the opposed-phase T1 sequence (b), where they appear hypointense.
The patient underwent scheduled surgery, during which several SOL were observed in the liver, the largest being 6cm in segment IVb and 2.5cm in segment II, which were soft in consistency and well encapsulated. The intraoperative ultrasound demonstrated 7 liver lesions larger than 1cm and several superficial lesions measuring 1–2mm. The intraoperative biopsy determined the absence of malignancy. With the suspicion of adenoma, the 2 largest tumours were resected.
The patient had an uneventful recovery and was discharged on the fifth day post-op.
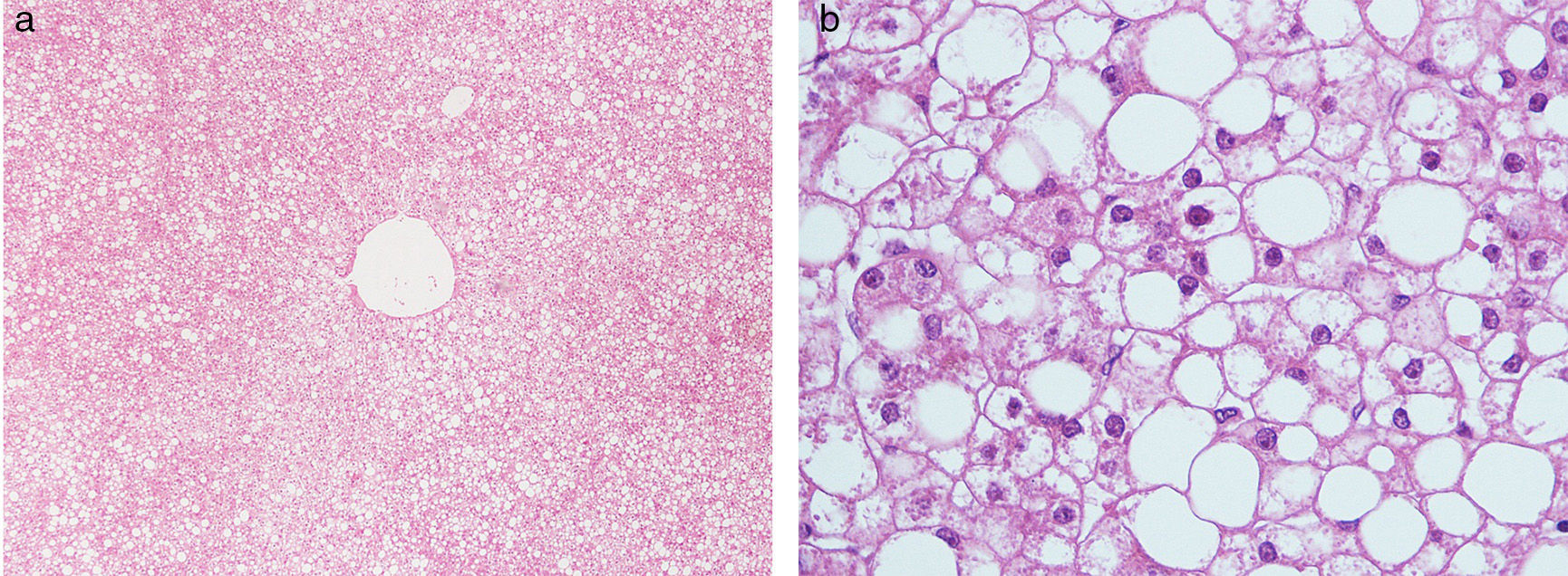
The pathology results reported multinodular focal hepatic steatosis (Fig. 2).
Hepatic steatosis is a clinical entity that involves an accumulation of triglycerides within the cytoplasm of normal hepatocytes. Its prevalence in the general population is 15%, although this increases to 45%–95% in populations at risk.1,2 Predisposing factors that have been described are: alcoholism, diabetes, obesity, steroid therapy, endocrinopathies, metabolic pathologies and parenteral nutrition, cystic fibrosis and pregnancy.3,4
Patients are usually asymptomatic, but they can occasionally present hepatomegaly, portal hypertension and alterations in liver function.
Radiologically, multinodular focal steatosis usually presents as hyperechoic lesions due to the interface of fatty/non-fatty tissue. On CT, they are hypodense4 and less enhanced than the liver.3 MRI provides the definitive diagnosis in most cases. In-phase/opposed-phase T1 sequences are the most specific for detecting intralesional fatty content.1,4 The contrasts used are gadolinium, an extracellular contrast with distribution similar to that of iodine contrast in CT, or mangafodipir trisodium (Mn-DPDP), a contrast material that is selectively captured by hepatocytes. It is usually used to characterise non-hepatocellular lesions and focal hepatic lesions such as adenoma or focal nodular hyperplasia.
Hepatic adenomatosis is a little-known disease of unclarified aetiology.5,6 It involves a high rate of complications (necrosis, haemorrhage, malignisation).6 It is usually more frequent in women (3:1)6 and oral contraception is an aetiological factor in many cases.5 Diagnosis is usually reached due to hepatomegaly, the appearance of complications, or as an incidental finding during laparotomy.6 The definitive diagnosis of adenoma made by imaging techniques is difficult, as they are usually lesions with a nonspecific semiological pattern. Therapeutic options include liver resection or transplantation.7,8
In the clinical case that we present, multifocal nodular fatty infiltration of the liver was erroneously diagnosed as hepatic adenomatosis. MRI revealed the existence of intralesional fatty content in the study in T1 in-phase/opposed-phase. The behaviour of the lesions in the triphasic CT study suggested the existence of adenomas, and it was decided to schedule a surgical intervention due to the risk of complication that these lesions present and considering their size.
Multinodular focal hepatic steatosis is a pathology that we should include within the differential diagnosis of focal liver lesions. We should consider the patient's medical history and study morphological factors, echogenicity, attenuation, signal intensity, extracellular contrast uptake and cell-specific uptake on MRI. On many occasions, these data can provide the diagnosis of hepatic steatosis without the need for biopsy.
Please cite this article as: Gallarín Salamanca IM, Galeano Díaz F, Rubio Fernández A, Blanco Fernández G. Esteatosis hepática focal multinodular. Cir Esp. 2016;94:240–241.