The most common zoonosis in the world is brucellosis, which is caused by microorganisms of the genus Brucella. Brucella are gram-negative aerobic bacteria with the in vivo capability to behave like facultative intracellular parasites.1 They affect animals and can cause systemic infections in humans with acute, subacute or chronic forms.2,3
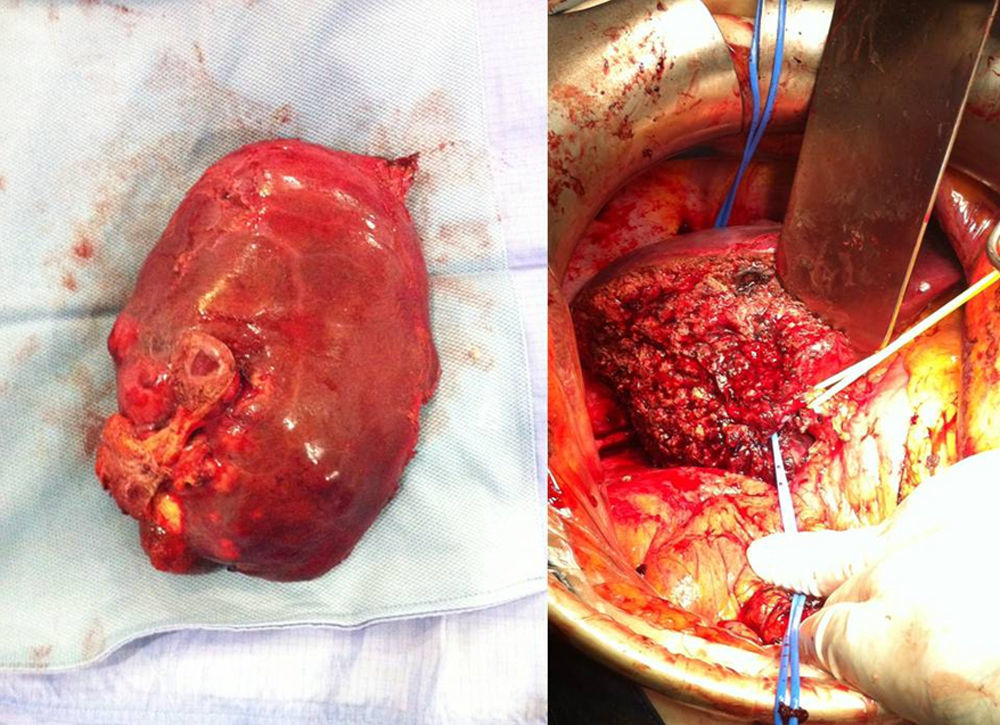
We present the clinical case of a 48-year-old male with a history of brucellosis at the age of 14. He had been diagnosed with a recurrence of hepatic brucellosis that persisted in spite of being treated, first of all, with doxycycline in association with aminoglycoside and afterwards, until surgery, with doxycycline, ciprofloxacin and rifampicin, the latter of which had to be withdrawn due to the loss of finger sensitivity. Because of poor clinical–radiological progress (fever and anorexia with weight loss, as well as increased number and size of hepatic lesions) and a failed attempt at percutaneous drainage, the patient was referred to our hepatobiliary-pancreatic surgery unit, at which time we decided to operate. During surgery, a large liver mass was found that occupied segments 5, 6 and 4B, with infiltration of the anterior abdominal wall and diaphragm. We performed extended right hepatectomy and en bloc resection of a fragment of the infiltrated abdominal wall and diaphragm (Fig. 1). Macroscopic and microscopic studies reported a hepatectomy specimen weighing 960g and measuring 19cm×16cm×7cm, which presented edges with an irregular yellowish-white area that was fibrinopurulent in appearance and measured 12cm×14cm×6.5cm, where necrotising epithelioid granulomas were observed.4 The postoperative period progressed favourably, without complications. Upon discharge, the patient continued with antibiotic treatment (doxycycline and ciprofloxacin). After 7 months of follow-up, the patient is asymptomatic, has gained weight and shows no clinical, analytical or radiological signs of disease recurrence.
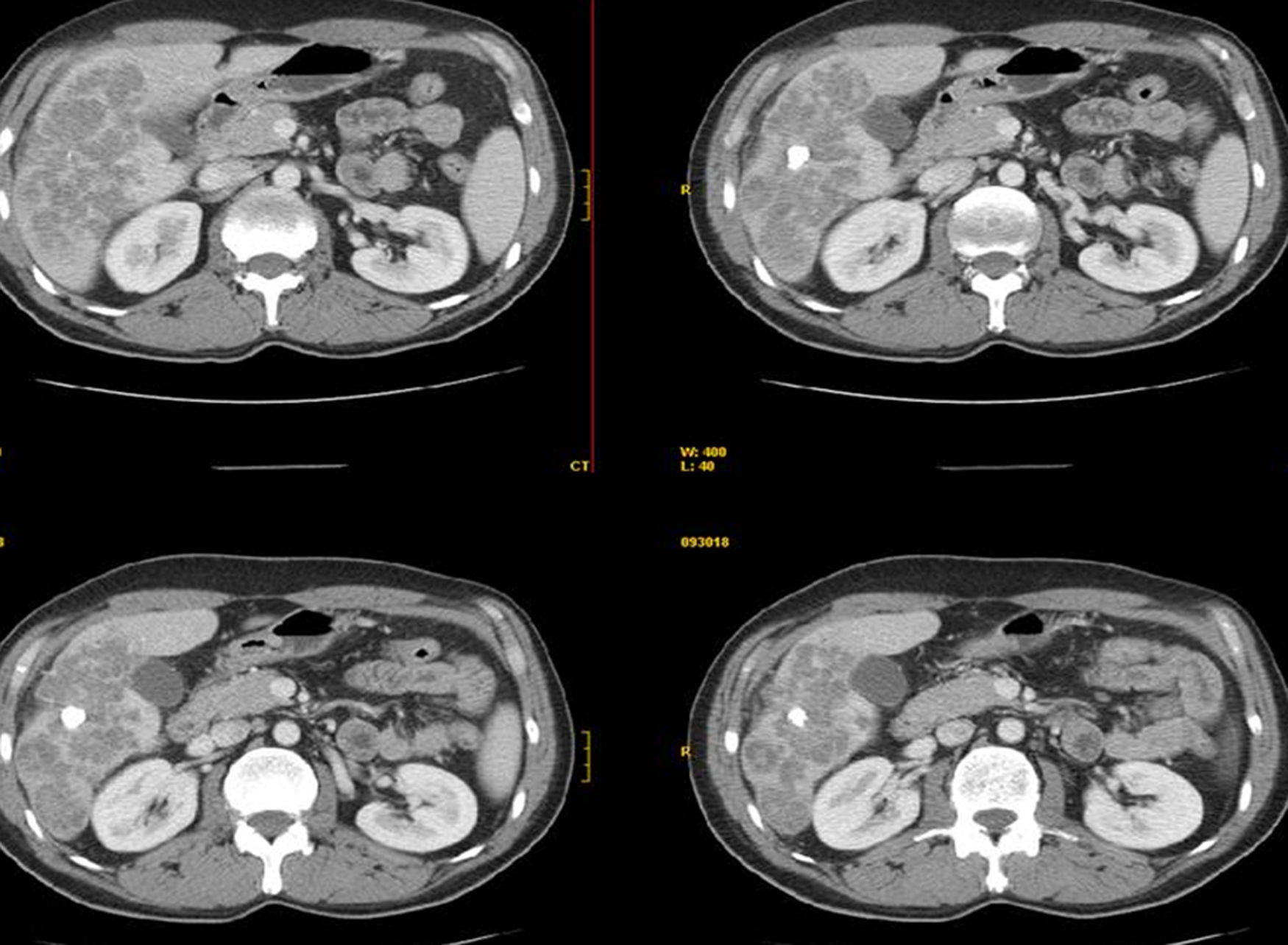
The difficulty to completely eradicate this disease, as well as the appearance of delayed focal complications, is due to its affinity for the cells of the mononuclear phagocyte system and capacity for cantonment.5 Hepatic brucellomas are usually rare complications that generally occur in adults with chronic forms of the disease. Radiologically, they are observed to be single lesions with a pseudo-tumoural appearance, poorly defined margins, irregular edges, heterogeneous content, possible cavitations and typically the presence of a central calcification6 (Fig. 2). Bacteriological cultures are usually positive in the acute phase of brucellosis, although in the case of brucellomas they are almost always negative (diagnostic performance 10%–30%), which makes it necessary to repeat serology tests.7,8 Serological testing is based on the detection of antibodies, done with rose Bengal stain. In spite of never having been completely validated for diagnosis in humans,1 the Coombs anti-Brucella test is thought to have the greatest sensitivity. Frequently, serology tests in brucellomas are not conclusive, so it is therefore recommended to use PCR assay, which is useful in blood as well as in purulent exudate or tissue samples.
We can conclude that, when faced with a space-occupying lesion in the liver with poorly defined margins, heterogeneous content and central calcification, the possibility of a hepatic brucelloma should be considered in the differential diagnosis. Furthermore, clinical studies should include the PCR technique for Brucella since serological testing in this phase of the disease is frequently inconclusive. Last of all, we would like to emphasise that the combination of hepatic surgery and specific antibiotic treatment for 6–8 weeks is ideal to guarantee the absolute eradication of this zoonosis in recurring clinical cases or patients with little therapeutic response to antibiotic treatment or percutaneous drainage.9
Conflict of InterestThe authors have no conflict of interest to declare.
Please cite this article as: Valero Liñán AS, Miota de Llama JI, González Masiá JA, Rueda Martínez JL, González Masegosa P. Bruceloma hepático: actitud terapéutica. Cir Esp. 2016;94:238–239.