Right hepatic artery (RHA) injury after laparoscopic cholecystectomy (LC) may go unnoticed clinically, but can sometimes cause necrosis of the right lobe. Exceptionally, when the necrosis spreads to segment IV, fulminant liver failure (FLF) may occur, and an urgent liver transplantation (LT) may be required.
Patients and methodWe provide a review of the literature on patients with indication for an LT due to vascular damage caused by bile duct injury following LC. The case reported herein is the fourth described in the specialized literature of LT due to RHA injury after LC and the second of FLF after RHA injury.
ResultsLT due to RHA injury was performed in 3 of 13 patients reported in the literature: one LT was performed at 3 months due to FLF, after an extended right hepatectomy was performed, and the remaining two were performed due to secondary biliary cirrhosis. Our patient was transplanted due to FLF 15 days after the injury.
ConclusionsRHA injury after LC may require LT due to FLF. Although exceptional, this possibility should be considered when there are RHA complications that may require occlusion.
La lesión de la arteria hepática derecha (AHD) tras colecistectomía laparoscópica (CL) puede pasar desapercibida clínicamente, aunque a veces ocasiona una necrosis del lóbulo derecho. En situaciones excepcionales, cuando la necrosis se extiende al segmento IV, podría ocurrir un fallo hepático fulminante (FHF) y requerir un trasplante hepático urgente (TH).
Pacientes y métodoPresentamos una revisión de la literatura médica de los pacientes en los que se indicó TH debido a una lesión vascular secundaria a lesión biliar por CL. También presentamos el cuarto paciente descrito en la literatura especializada que precisó TH secundario a lesión de la AHD tras CL, el segundo por FHF.
ResultadosEl TH debido a la lesión de la AHD se realizó en 3 de 13 pacientes recogidos en la literatura médica: uno se realizó a los 3 meses de la lesión por FHF, tras realizar una hepatectomía derecha ampliada y los otros 2 debido a cirrosis biliar secundaria. Nuestro paciente se trasplantó a los 15 días de la lesión por FHF.
ConclusionesLa lesión de la AHD tras CL puede requerir TH por FHF, aunque es excepcional, es necesario pensar en esta posibilidad ante complicaciones de la AHD que requieran su oclusión.
Since the introduction of laparoscopic cholecystectomy (LC), the incidence of iatrogenic common bile duct injury (ICBDI) has doubled compared with open cholecystectomy (OC), and it is usually more complex (located higher and with frequent disappearance of bile duct segments).1–14 In addition, there has been an increase of associated vascular injury (between 17% and 40% of serious ICBDI after LC is associated with vascular injury), especially right hepatic artery (RHA) injury, crossing the common bile duct towards the right liver lobe (RLL).15–24 More serious injuries have also been reported that can affect the common hepatic artery (CHA)25,26 and the portal vein (PV) or any of its branches.18,27–33
RHA lesions may be due to occlusion during surgery or late lesions with the formation of pseudoaneurysms that may cause delayed rupture, manifesting in haemobilia and/or haemoperitoneum. RHA lesions often go unnoticed because patients are asymptomatic, although sometimes there is an elevation in liver enzymes or late RLL atrophy. These cases are resolved with conservative treatment. Less commonly, arterial ischaemia leads to necrosis and intrahepatic abscess that may require a right hepatectomy. It is rare for an isolated lesion of the RHA to cause liver failure leading to an indication for a liver transplant (LT). Bacha et al.,34 published in 1994 the first case of urgent LT due to RHA injury. Schmidt et al.15 and De Santibañes et al.32 published the cases of 2 patients undergoing a LT due to secondary biliary cirrhosis (SBC) after biliary and RHA injury.15
The aim of our study was to present a review of the literature for patients indicated a LT due to vascular injury secondary to biliary injury (RHA, common hepatic artery and portal vein lesions, alone or combined). We also describe the fourth patient described in the literature requiring a LT secondary to RHA injury after LC.
Materials and MethodsLiterature ReviewWe reviewed the medical literature regarding the clinical course and management of bile duct injuries after LC, associated with a RHA lesion, CHA lesion, or in combination with a PV injury. These articles were searched especially for those patients with an indication for a LT due to fulminant hepatic failure (FHF), sepsis or SBC, as long as it was secondary to associated biliary or vascular injury. The articles were obtained via PubMed using the keywords “laparoscopic bile duct injury and vascular injuries”; “laparoscopic bile duct injury and hepatic artery injuries”; “laparoscopic bile duct injury, vascular injuries and FHF”; and “laparoscopic bile duct injury and liver transplantation”.
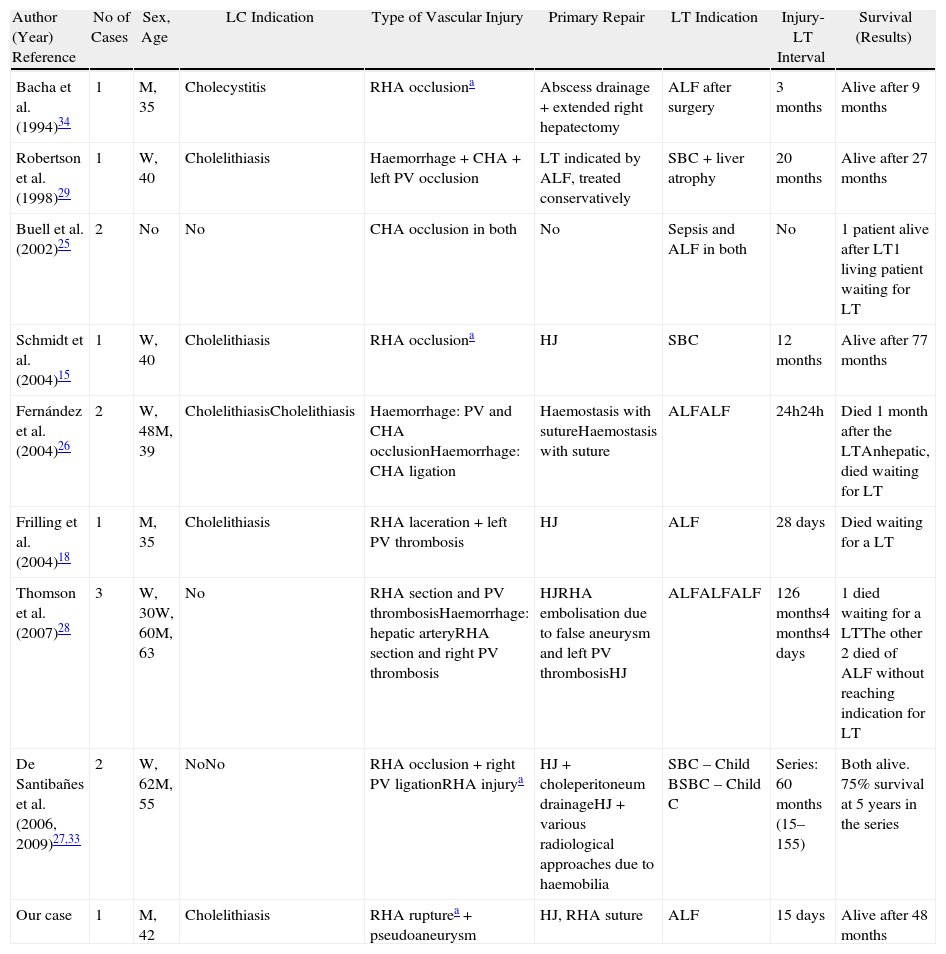
There were 13 patients found with an indication for a LT due to ICBDI and associated vascular injury (table 1), of whom 7 underwent a transplant and 6 died waiting. The vascular injuries leading to the indication for a LT were as follows: (A) The LT was performed in 3/13 patients due to a RHA lesion, one at 3 months after the injury, after an extended right hepatectomy34 who was alive 9 months after the LT; LT was performed in the other 2 patients due to secondary biliary cirrhosis, 1 was alive 21 months after the LT and the other one was alive 77 months after the operation. Our patient with the RHA injury who underwent a LT 15 days after iatrogenic biliary injury due to FHF was alive 48 months later. (B) LT indicated due to simultaneous portal and arterial injury for 6/13 patients: 2 patients underwent a transplant due to SBC and were still living, and 4 due to FHF who died (3 while waiting for a LT and the other one 1 month after the transplant). (C) LT was indicated due to CHA injury and FHF in 4/13 patients; 1 patient was living after LT and 3 died waiting, one of who was anhepatic.
Characteristics of Patients With an Indication for a Liver Transplant Due to Associated Vascular Injury.
| Author (Year) Reference | No of Cases | Sex, Age | LC Indication | Type of Vascular Injury | Primary Repair | LT Indication | Injury-LT Interval | Survival (Results) |
| Bacha et al. (1994)34 | 1 | M, 35 | Cholecystitis | RHA occlusiona | Abscess drainage+extended right hepatectomy | ALF after surgery | 3 months | Alive after 9 months |
| Robertson et al. (1998)29 | 1 | W, 40 | Cholelithiasis | Haemorrhage+CHA+left PV occlusion | LT indicated by ALF, treated conservatively | SBC+liver atrophy | 20 months | Alive after 27 months |
| Buell et al. (2002)25 | 2 | No | No | CHA occlusion in both | No | Sepsis and ALF in both | No | 1 patient alive after LT1 living patient waiting for LT |
| Schmidt et al. (2004)15 | 1 | W, 40 | Cholelithiasis | RHA occlusiona | HJ | SBC | 12 months | Alive after 77 months |
| Fernández et al. (2004)26 | 2 | W, 48M, 39 | CholelithiasisCholelithiasis | Haemorrhage: PV and CHA occlusionHaemorrhage: CHA ligation | Haemostasis with sutureHaemostasis with suture | ALFALF | 24h24h | Died 1 month after the LTAnhepatic, died waiting for LT |
| Frilling et al. (2004)18 | 1 | M, 35 | Cholelithiasis | RHA laceration+left PV thrombosis | HJ | ALF | 28 days | Died waiting for a LT |
| Thomson et al. (2007)28 | 3 | W, 30W, 60M, 63 | No | RHA section and PV thrombosisHaemorrhage: hepatic arteryRHA section and right PV thrombosis | HJRHA embolisation due to false aneurysm and left PV thrombosisHJ | ALFALFALF | 126 months4 months4 days | 1 died waiting for a LTThe other 2 died of ALF without reaching indication for LT |
| De Santibañes et al. (2006, 2009)27,33 | 2 | W, 62M, 55 | NoNo | RHA occlusion+right PV ligationRHA injurya | HJ+choleperitoneum drainageHJ+various radiological approaches due to haemobilia | SBC – Child BSBC – Child C | Series: 60 months (15–155) | Both alive. 75% survival at 5 years in the series |
| Our case | 1 | M, 42 | Cholelithiasis | RHA rupturea+pseudoaneurysm | HJ, RHA suture | ALF | 15 days | Alive after 48 months |
The indication of a LT for FHF (9 cases) had higher mortality (7 cases, 6 waiting for a LT and 1 died a month after the LT) than LT for SBC (with none of the 4 cases dying).
Below, we briefly describe a patient operated upon in our unit due to RHA injury associated with a bile duct injury that ended in an urgent LT.
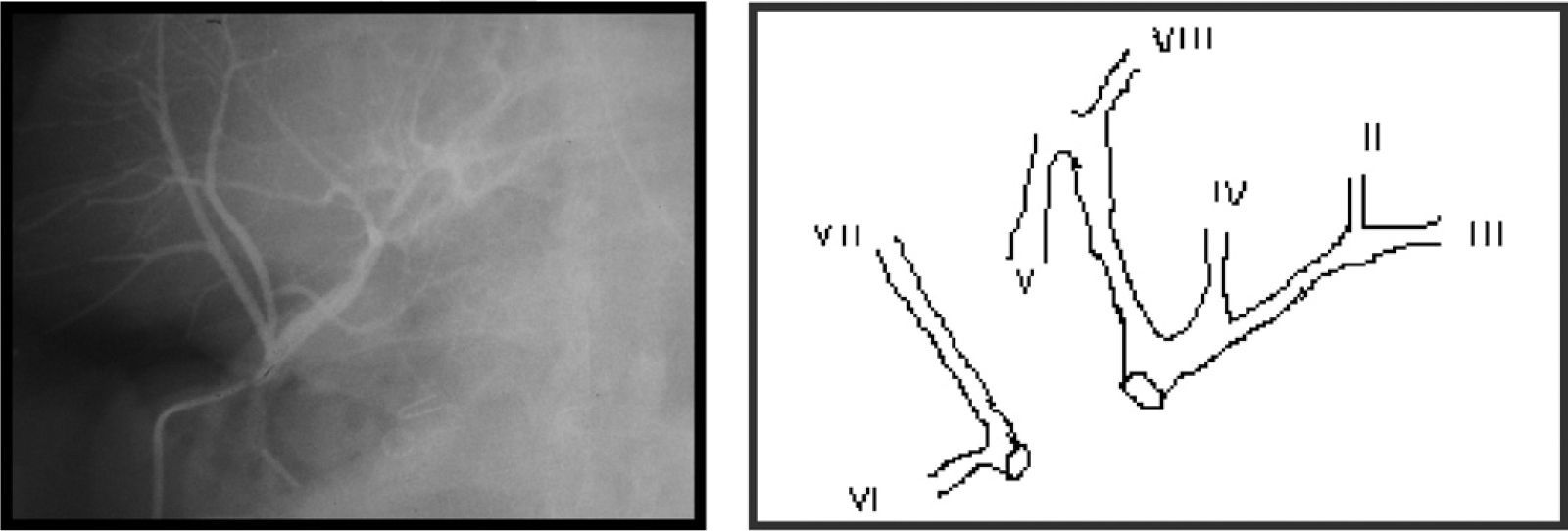
A 42-year old male, undergoing a LC for a simple cholelithiasis. During the operation, a complete section of the bile duct was performed and the crochet technique. Surgery was converted to a laparotomy, with suture of the right biliary radical and Roux-en-Y hepaticojejunostomy (R-en-Y H) to the hilar plate. A biliary fistula was found in the immediate postoperative period with a discharge of 500ml/24h via the subhepatic drain. On the third day he was sent to our unit. After 24h he underwent emergency surgery due to bile peritonitis (diffuse abdominal pain, leukocytosis 18000, drainage of biliary discharge of 500ml/24h and abundant free abdominal fluid visible on the abdominal ultrasound). The suture of the right posterior radical (Fig. 1) and biliary necrosis with dehiscence of the R-en-Y H was observed. The local damage caused by the crochet technique was seen during surgery, but the arterial vascularisation was preserved. A new R-en-Y H was performed on 2 biliary radicals with guides. On the 5th post-operative day, a biliary fistula with a discharge of 100–200ml/24h appeared.
After 15 days with the biliary fistula, there was a massive haemobilia and haemoperitoneum with important haemodynamic repercussions and a haematocrit decrease to 18%, requiring a transfusion of 6 units of blood. Emergency surgery was required and haemorrhage from rupture of the RHA was seen near the insertion of the cystic artery clip, which was repaired with microsurgery. After 48h, the patient developed a FHF with renal, respiratory and haemodynamic failure; prothrombin activity fell to 20% despite the administration of plasma. The abdominal CT scan showed ischaemia, with signs of RLL necrosis extended to S. IV (Fig. 2). An extended right hepatectomy was attempted but was impossible due to excessive haemodynamic instability, so an urgent LT was indicated. This was performed 48h after inclusion (with the piggy-back technique, and the bile duct reconstructed with a new R-en-Y H). One week after transplantation, a high-flow biliary fistula was found. The patient was operated upon again and complete dehiscence of the R-en-Y H was found. Due to the poor state of the jejunal loop and inframesocolic space after previous peritonitis, it was decided to externalise the bile through a probe placed in the donor liver bile duct. The patient was re-operated 20 days after the LT by performing an end-to-end choledococholedocostomy with a nasobiliary drain as guide.
During 5 months of hospitalisation in the ICU, he presented nosocomial pneumonia, pleural effusion that required drainage, acute renal failure requiring haemofiltration and sepsis from Acinetobacter baumannii, Enterococcus faecalis and Pseudomonas aeruginosa. The patient was discharged, and was asymptomatic for 48 months after the LT.
DiscussionThe incidence of ICBDI after LC is nearly twice that for OC (0.3%–0.6% vs 0.1%–0.3%),1–14,22–25 with more complex lesions (more severe, higher location and frequent disappearance of bile segments). It is sometimes associated with vascular injury and its actual incidence is not known, although numerous articles15–17,19,25,35–37 have suggested that it is higher than that of OC. In a multicentre study by Deziel et al.35 of 77604 patients with LC, 44 RHA lesions were found (0.006% of the total and 12% of those with IBDI). By selective angiography in 55 patients with IBDI, Alves et al.17 demonstrated that 26 (47%) had vascular lesions: 20 with RHA disruption, 2 had pseudoaneurysm of the RHA, 3 had PV injury, and 1 had PV and hepatic artery injury.
The Bismuth–Strasberg38 classification is the most accepted for these lesions, although the Hannover39 is preferred when there is associated vascular injury. Vascular injury after LC is primarily associated with high bile duct injury (E4–E5 in the Bismuth–Strasberg classification; our patient had E4 biliary type injury with 2 independent intrahepatic ducts), with the most frequent being RHA injury. It occurs during dissection in Calot's triangle or when a fragment of the common bile duct is removed (when confused with the cystic duct), as the RHA crossing this bile duct is injured.17,18,27–33 The RHA may be clipped, sectioned or cauterised, either by being confused with the cystic artery or during bleeding episodes when performing haemostasis blindly. After conversion to laparotomy, total stitching in the liver hilum can be implemented, injuring the common bile duct and/or hepatic hilar vessels.26 Late RHA injury is seen as pseudoaneurysms or rupture of this artery, which often causes haemobilia or gastrointestinal or intraperitoneal bleeding,28,40–42 as in our patient who presented with a haemobilia and haemoperitoneum with haemodynamic instability. The pathogenesis of the pseudoaneurysm causing arterial rupture is unknown. It may be related to the possible intraoperative injury of the RHA wall by diathermy leaving it devitalised,42,43 or due to a fungal infection44 eroding the arterial wall. Occasionally, the arterial injury may be more severe and affect the CHA.25,26 Less common is the combination of portal and arterial injury, but is of greater clinical severity.18,26,28–30 Portal and biliary injury, without arterial injury, is less common.
The consequences of RHA injury are unpredictable and are related to hepatic vascularisation, as the liver blood flow is maintained through the PV and left hepatic artery. Thus, in the Alves et al.17 cohort, all patients with occlusion of the RHA, neovascularisation of the right liver through the left hepatic artery was seen in the arteriography. However, ischaemia may have 2 types of effects: first, on the RLL, which may have diverse clinical manifestations;30,36 and, secondly, on the extrahepatic bile duct, since biliary vascularisation comes from the RHA. This factor has been associated with the failure of biliary reconstruction, stenosis, or biliary fistulas.
From a clinical standpoint, patients with RHA injury may be asymptomatic in most cases, with minimal abnormalities in analytical tests or RLL atrophy. Less commonly, the RLL ischaemia may progress to necrosis, liver abscess and sepsis.15,17,18,25 There are late lesions with ruptured pseudoaneurysms which may cause haemobilia and intraperitoneal haemoperitoneum.39,41 The development of FHF after RHA injury has been reported only by Bacha et al.,34 with our patient being the second case described in the literature. If associated with a portal injury,18,26–33 it is more severe and manifests with FHF due to liver ischaemia.
Vascular injury can be diagnosed during LC or when converting to OC to repair biliary injury. It is mostly diagnosed at a late stage in a patient with biliary injury referred to a specialist centre for late repair or after primary repair failure.19,26,28 Doppler ultrasound is not very reliable25 due to local conditions after ICBDI. CT with IV contrast3,13,19 and celiac arteriography confirm the absence of flow and status of the liver parenchyma.3,16 Arteriography has not been shown to be required in all ICBDI cases,15,25,41 although if clinical suspicion is high it must be investigated.17 Some authors13,19 attach great importance to magnetic resonance imaging with vascular reconstruction.
According to some authors,2,15,16,19,25,30,45 vascular injury diagnosed in intraoperative LC treated by direct arterial repair offer good results, as long as it is carried out in specialist centres. Schmidt et al.15 described 54 patients with 11 arterial lesions (20%). No patient developed FHF, and immediate direct revascularisation was possible in 2/11 cases, although it was impossible in cases diagnosed late. Bachellier et al.19 reported 3 arterial lesions in 15 patients who developed no complications, 2 of whom were able to be given direct repair. Therefore, associated arterial lesions which may require immediate repair should be identified in specialist centres. However, other authors16 suggest that arterial injury should be ignored during primary biliary repair, as the consequences of ligation of the RHA on a healthy liver can escape clinical detection in most cases.
If the arterial lesion is diagnosed with necrosis of the RLL in the late postoperative period, direct repair is less likely, and a right hepatectomy15–24,31–33 or other type of liver resection may be necessary. Madariaga et al.30 reported 5 arterial lesions in 14 iatrogenic biliary injury lesions. Repair was achieved in 1 of them and a right hepatectomy had to be performed in 2 others. The Alves et al. cohort of 19 RHA injury patients had 12 right hepatectomies, with a good outcome for all patients. Because of the extent of necrosis, an extended right hepatectomy was attempted in our case, but was impossible due to haemodynamic instability.
For cases of RHA injury with formation of a pseudoaneurysm, treatment depends on the clinical situation. Major bleeding requires emergency surgery for haemostasis, as occurred in our patient. Madanur et al.41 reported 4 pseudoaneurysms: 3 were resolved with embolisation of the RHA, and 1 with emergency surgery and suture of the RHA after rupture and haemoperitoneum. Thomson et al.28 described a case who died after embolisation of a pseudoaneurysm of the CHA who developed FHF and died waiting for a LT.
There are 3 cases in the literature of a LT injury secondary only to RHA injury, and only one of them for FHF. Bacha et al.34 published a case of necrosis of the RLL, initially treated with percutaneous drainage of intrahepatic collections. After 3 months, the patient underwent a right trisegmentectomy, after surgery presented a FHF and needed a LT. In our patient, the FHF developed because of the rupture of a pseudoaneurysm of the RHA 2 weeks after biliary repair. This was probably related to an arterial wall injury during cholecystectomy remaining weakened. The presence of a biliary fistula after the first repair could also have contributed to arterial rupture, as vascular lesions have been described in patients with biliary and/or pancreatic fistula. FHF may have contributed to the existence of liver disease (2 consecutive interventions, a recent biliary peritonitis and the presence of an external biliary fistula) and necrosis that affected the entire RLL extending to the S. IV (Fig. 2), with a small left lobe. The other 2 patients with RHA injury were transplanted due to SBC.15,32
An injury associated with RHA or CHA with PV injury or PV branch injury is more serious and complex.18,25–33 It occurs most often in situations of severe intraoperative bleeding. After conversion to laparotomy, clips are placed blindly or stitching of the hepatic hilum is performed with the intention of performing haemostasis. These cases may be serious, because, after the conversion, the surgeon usually has to perform stitching in the hepatic hilum due to bleeding, leading to arterial and portal occlusion and FHF within 12–24h. The patient may even die without the possibility of a LT (5 of the 7 cases with arterial and portal injury in our review died, and 2 of the 3 cases with LT and FHF due to the CHA injury died while waiting for a LT).
The main form of biliary reconstruction is R-en-Y H, as the injury is very high with no common bile duct segments. The most appropriate time to repair the biliary injury is open to discussion, especially if associated with vascular injury, as this has been associated with an increased incidence of fistulas and biliary stenosis.30,36 Some authors advocate delayed biliary repair where there is severe thermal injury, local sepsis, associated vascular injury or when the biliary radicals are widely separated.46 However, other authors have obtained good results with primary repair, with no differences in morbidity or mortality for patients with or without associated vascular injury,16,25 provided that the biliary reconstruction is performed in an experienced hepatobiliary centre. E4 and E5 type injuries require R-en-Y H intrahepatically or in separate ducts, and sometimes central liver resection.47,48
In conclusion, RHA injury after iatrogenic biliary injury usually goes unnoticed or may require right hepatectomy. However, occasionally it leads to a FHF that may require a LT. The association of CHA or portal injury is more serious and may lead to FHF. These lesions must be treated in tertiary hospitals with liver surgery and LT units.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please, cite this article as: Robles Campos R, et al. Hemorragia diferida de la arteria hepática derecha tras iatrogenia biliar por colecistectomía laparoscópica que precisó trasplante hepático por insuficiencia hepática aguda: caso clínico y revisión de la literatura. Cir Esp. 2011;89:670–6.