The indications for adrenalectomy could be changing by the availability of laparoscopy and the growing detection of incidentalomas. The Endocrine Surgery Section of the Spanish Association of Surgeons conducted a survey to analyse the current indications for adrenalectomy and their results in Spanish surgical departments.
Material and methodsData were gathered as regards the type of hospital and department, volume of procedures, localisation studies and pre-surgical preparations, indications, surgical approach, and results in terms of morbidity and hospital stay. The results of the centres were compared as regards their volume of activity using the Mann–Whitney Test for the quantitative variables and chi squared for the qualitative ones.
ResultsThirty-six centres completed the questionnaire and 301 adrenalectomies were reported to be performed in 2008. Most frequent indications were pheochromocytoma (25.2%), non-functioning adenoma (16.2%), aldosteronoma (15.9%), Cushing adenoma (11.2%), metastasis (10.3%), myelolipoma (5.6%), and carcinoma (4.9%).
Laparoscopic adrenalectomy was performed in 83.7% of cases (6.7% required conversion to laparotomy). The mean hospital stay was 3.9 days for laparoscopic adrenalectomy and 7.4 days for laparotomy. High-volume units (more than 10 per year) used more frequently the laparoscopic approach (P=.019), and had a shorter overall hospital stay (P<.0001. Laparoscopic adrenalectomy was also associated with a shorter hospital stay (P<.0001).
ConclusionsLaparoscopy for adrenalectomy has become the standard practice in Spain, with good results in terms of morbidity and hospital stay. High volume centres have better results as regards the use of minimally invasive surgery and hospital stay.
Dada la disponibilidad del abordaje laparoscópico y la creciente detección de incidentalomas, las indicaciones de suprarrenalectomía pueden estar cambiando. La Sección de Cirugía Endocrina de la Asociación Española de Cirujanos diseñó una encuesta para analizar las indicaciones actuales de la suprarrenalectomía y sus resultados en los servicios de cirugía españoles.
Material y métodosSe recogieron datos respecto al tipo de hospital y servicio, volumen de procedimientos, estudios de localización y preparación preoperatoria, indicaciones, técnica quirúrgica, instrumental utilizado, y resultados en términos de morbilidad y estancia hospitalaria. Se compararon los resultados de los centros en función de su volumen de actividad, utilizando las pruebas de Mann-Whitney para variables cuantitativas y de la chi al cuadrado para las cualitativas.
ResultadosTreinta y seis centros cumplimentaron el cuestionario e incluyeron 301 suprarrenalectomías realizadas en 2008. Las lesiones extirpadas más frecuentes fueron feocromocitoma (25,2%), adenoma no funcionante (16,2%), aldosteronoma (15,9%), adenoma de Cushing (11,2%), metástasis (10,3%), mielolipoma (5,6%) y carcinoma (4,9%).
Se realizó un abordaje laparoscópico en el 83,7% de casos (el 6,7% requirió conversión a laparotomía). La estancia media hospitalaria fue de 3,9 días para suprarrenalectomía laparoscópica y 7,4 para la laparotómica. En las unidades con un número elevado de casos intervenidos (más de 10 por año) se observó una mayor proporción de pacientes tratados por laparoscopia (p=0,019), con una menor estancia global (p<0,000), así como en los que se realizó una suprarrenalectomía laparoscópica (p<0,000).
ConclusionesEn España, el abordaje laparoscópico para la suprarrenalectomía es la norma, con buenos resultados en términos de morbilidad y estancia hospitalaria. Los centros de volumen alto tienen mejores resultados en relación con el uso de cirugía mínimamente invasiva y la estancia hospitalaria.
Adrenalectomy is a surgical procedure performed with increasing frequency, as shown by large US series analysing hospital discharge data since the 1980s.1–3 This can be explained by two related circumstances: firstly, the increasing detection of adrenal injury (whose prevalence is currently estimated at about 4%–7%) due to the widespread use and higher resolution of computed tomography; secondly, the widespread availability of laparoscopic equipment and professionals with experience in this surgical approach, increasing the likelihood that doctors recommend adrenalectomy to their patients.4 Currently, the procedure has a low mortality rate (<1%) and morbidity of 8%–19% in large cohorts.4–6
The amount of hospital activity has been positively associated with better postoperative outcomes after the implementation of various techniques, including thyroidectomy, parathyroidectomy, bypass surgery, aortic valve replacement, repair of abdominal aortic aneurysm, bariatric surgery, pancreaticoduodenectomy, oesophagectomy and colorectal cancer surgery.7–14 In the specific field of adrenal pathology, various US and European articles have also analysed the volume factor, whereby a lower rate of postoperative complications and hospital stay after adrenalectomy is found when it is performed by a surgeon and a hospital with a high volume of surgical activity.1–3,15
The endocrine surgery section of the Spanish Association of Surgeons (Asociación Española de Cirujanos, AEC) prepared a survey in 2009 to assess the current status of adrenal surgery in Spain regarding indications, techniques and results. It was expected to find out the relationship between the volume of hospital activity and morbidity, mortality and hospital stay after the procedure. A preliminary analysis of the results using data from a small number of hospitals was published in the official European Society of Endocrine Surgeons publication.16 The final results of this study are shown here.
Material and MethodsA prospective multicentre study analysed the 31 items in a survey prepared by the endocrine surgery section of the AEC regarding the type, size and ownership of the hospital, the type of unit where the adrenal surgery was performed, the department to which it belonged and the number of surgeons practising the technique in that unit. Other topics on which information was requested were: location testing, preoperative preparation, preoperative hospital stay, the total volume of procedures performed in 2008, the pathology types operated upon, the surgical approach and contraindications considered absolute or relative for the laparoscopic approach. Information was also sought on the technical details of the procedure: the number of ports used in endoscopic surgery, the type of laparoscope and haemostatic material used, the use of drains, the availability of laparoscopic ultrasound and robotic technology. Finally, the results for laparotomy conversion rates, morbidity, urgent re-operations, mortality and postoperative and overall hospital stay were requested. Complications were studied in aggregate, and classified into general, intra-abdominal and abdominal wall complications.
The survey questionnaire, with a cover letter, was emailed by the AEC secretariat to all its surgeons in July 2009. Two months later, a follow-up email was sent to the endocrine surgery section members. Data from the returned questionnaires were entered onto an Access 2003 database, and responses were accepted until December 2010. After excluding duplicate responses from the same unit, the data were exported to a SPSS version 15.0 file for statistical analysis.
To analyse the results according to activity volume, two groups were defined: high-volume centres (with 10 or more procedures in 2008) and low-volume centres (9 or less adrenalectomies performed in that year). The data from these subgroups were compared regarding the type of surgical approach (laparoscopy or laparotomy), the proportion of malignant tumours (primary or metastatic) in those lesions intervened and conversion rates to laparotomy. Other data analysed were the mortality rate, postoperative complications, urgent re-operations and hospital stay.
Statistical AnalysisThe chi-squared and Mann–Whitney U tests were used for differences between groups in categorical and continuous variables, respectively. All tests were two-tailed, and statistical significance was P<.05.
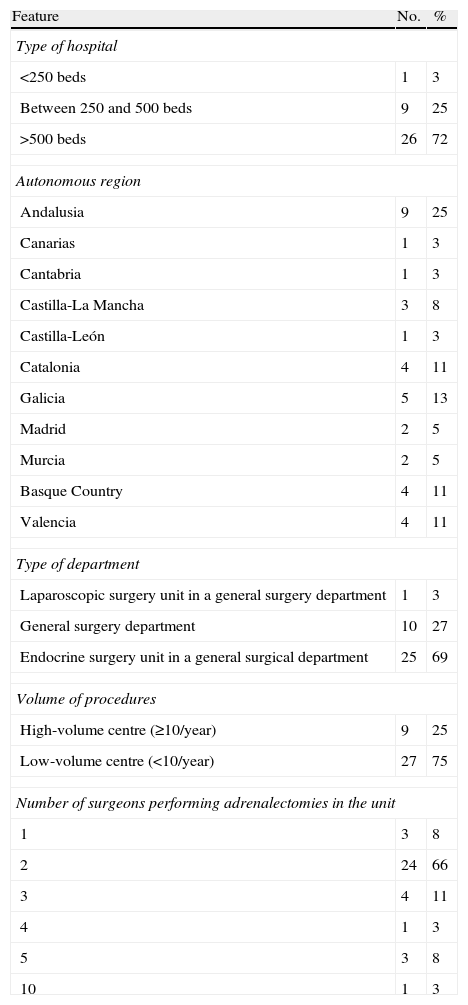
ResultsA total of 36 surgeons answered the questionnaire from different hospitals, 35 (97%) of whom belonged to public centres. The response rate was 10.4% of the 334 Spanish public hospitals registered in 2008.17Table 1 shows the different features of the hospitals and units, with all belonging to the general and digestive surgery departments. Of the 9 high-volume hospitals, 8 (89%) had over 500 beds and one between 250 and 500 beds.
Features of Participating Centres.
| Feature | No. | % |
| Type of hospital | ||
| <250 beds | 1 | 3 |
| Between 250 and 500 beds | 9 | 25 |
| >500 beds | 26 | 72 |
| Autonomous region | ||
| Andalusia | 9 | 25 |
| Canarias | 1 | 3 |
| Cantabria | 1 | 3 |
| Castilla-La Mancha | 3 | 8 |
| Castilla-León | 1 | 3 |
| Catalonia | 4 | 11 |
| Galicia | 5 | 13 |
| Madrid | 2 | 5 |
| Murcia | 2 | 5 |
| Basque Country | 4 | 11 |
| Valencia | 4 | 11 |
| Type of department | ||
| Laparoscopic surgery unit in a general surgery department | 1 | 3 |
| General surgery department | 10 | 27 |
| Endocrine surgery unit in a general surgical department | 25 | 69 |
| Volume of procedures | ||
| High-volume centre (≥10/year) | 9 | 25 |
| Low-volume centre (<10/year) | 27 | 75 |
| Number of surgeons performing adrenalectomies in the unit | ||
| 1 | 3 | 8 |
| 2 | 24 | 66 |
| 3 | 4 | 11 |
| 4 | 1 | 3 |
| 5 | 3 | 8 |
| 10 | 1 | 3 |
No.: number of units; %: percentage.
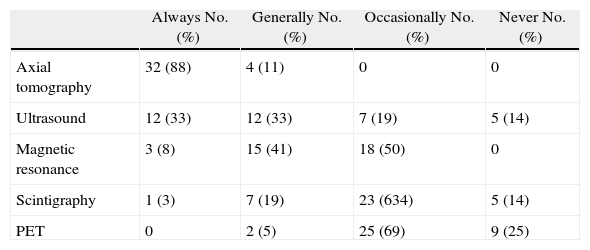
Table 2 summarises the degree of use of different preoperative location techniques, with the most widely used being axial tomography. All units carried an alpha-blockade followed by a beta-blockade for the preoperative preparation of pheochromocytoma, with 28 centres (77%) using phenoxybenzamine and the remaining 8 (22%) using doxazosin as the alpha-blocker. Calcium antagonists were considered as an alternative in 3 hospitals (8.3%). The average preoperative hospital stay for this preparation was 2.7, range 0–10, standard deviation [SD] 2. The preoperative hospital stay for the rest of pathologies, however, was 0.7 days (range 0–2, SD 0).
Use of Different Location Techniques in the Participating Units.
| Always No. (%) | Generally No. (%) | Occasionally No. (%) | Never No. (%) | |
| Axial tomography | 32 (88) | 4 (11) | 0 | 0 |
| Ultrasound | 12 (33) | 12 (33) | 7 (19) | 5 (14) |
| Magnetic resonance | 3 (8) | 15 (41) | 18 (50) | 0 |
| Scintigraphy | 1 (3) | 7 (19) | 23 (634) | 5 (14) |
| PET | 0 | 2 (5) | 25 (69) | 9 (25) |
No.: number of units that perform the technique in question; PET: positron emission tomography.
There were 301 adrenalectomies performed in these 36 centres in 2008, with an average of 8.3 interventions per centre (range 2–25, SD 5). High-volume centres performed 135 procedures, with an average of 15 per hospital (range 10–25, SD 5); while low-volume centres performed 166 adrenalectomies, with an average of 6.1 (range 2–9, SD 2).
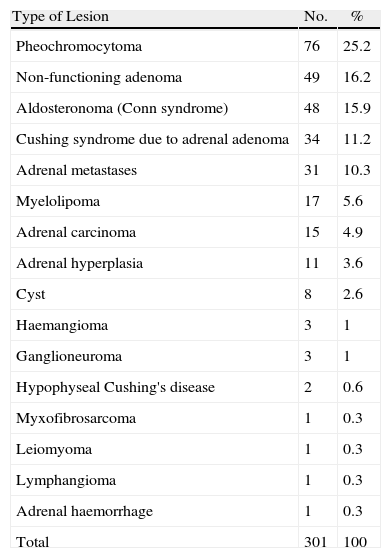
The most frequent indication (160 cases, 53.1% of all patients) was hormonal hypersecretion, followed by an adrenal incidentaloma (64 cases, 21.2%), suspicion of malignancy (51 patients, 16.9%) and adrenal mass with compressive symptoms (26 cases). The histological diagnoses of the excised lesions are shown in Table 3.
Diagnostic Pathology of The Excised Lesions.
| Type of Lesion | No. | % |
| Pheochromocytoma | 76 | 25.2 |
| Non-functioning adenoma | 49 | 16.2 |
| Aldosteronoma (Conn syndrome) | 48 | 15.9 |
| Cushing syndrome due to adrenal adenoma | 34 | 11.2 |
| Adrenal metastases | 31 | 10.3 |
| Myelolipoma | 17 | 5.6 |
| Adrenal carcinoma | 15 | 4.9 |
| Adrenal hyperplasia | 11 | 3.6 |
| Cyst | 8 | 2.6 |
| Haemangioma | 3 | 1 |
| Ganglioneuroma | 3 | 1 |
| Hypophyseal Cushing's disease | 2 | 0.6 |
| Myxofibrosarcoma | 1 | 0.3 |
| Leiomyoma | 1 | 0.3 |
| Lymphangioma | 1 | 0.3 |
| Adrenal haemorrhage | 1 | 0.3 |
| Total | 301 | 100 |
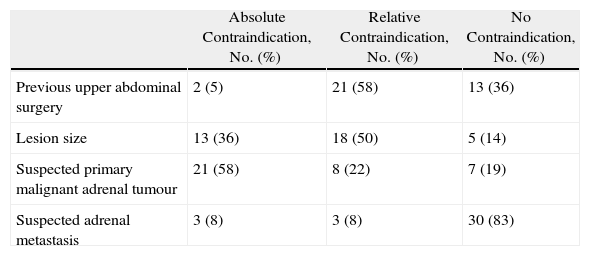
Adrenalectomy was performed through a laparoscopic transperitoneal lateral approach in 252 cases (83.7%), while 2 hospitals (5%) had not then implemented the laparoscopic approach. The incision of choice for laparotomic adrenalectomy was subcostal (72% of units), followed by midline laparotomy (22%) and the posterior approach (6%). Table 4 shows the opinion of surgeons regarding the different conditions that might preclude the laparoscopic approach. The maximum size of the endoscopically resectable adrenal lesion varied according to the different units and was defined in 16 of them: it was 15cm in 1 case, 12cm in another, 10cm in 7 units, 8cm in 4 and 6cm in 3 units.
Surgeons’ Opinions About Contraindications for the Laparoscopic Approach of Adrenal Lesions.
| Absolute Contraindication, No. (%) | Relative Contraindication, No. (%) | No Contraindication, No. (%) | |
| Previous upper abdominal surgery | 2 (5) | 21 (58) | 13 (36) |
| Lesion size | 13 (36) | 18 (50) | 5 (14) |
| Suspected primary malignant adrenal tumour | 21 (58) | 8 (22) | 7 (19) |
| Suspected adrenal metastasis | 3 (8) | 3 (8) | 30 (83) |
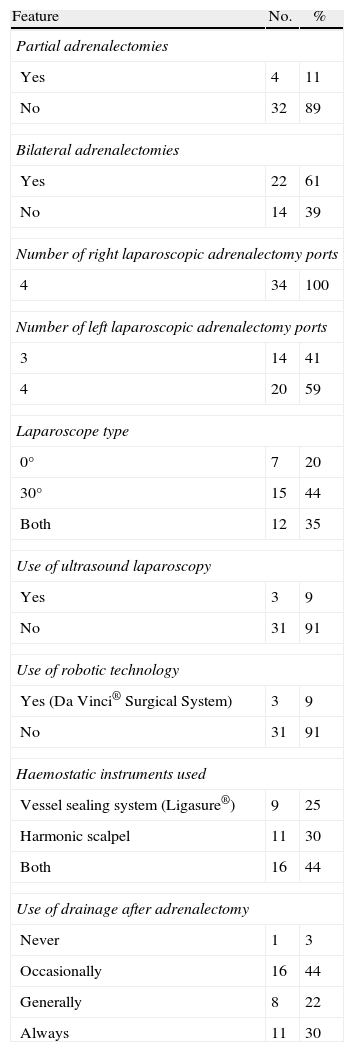
Table 5 shows some technical details of the procedures. The indications collected by the various units for partial adrenalectomy included bilateral pheochromocytoma, adrenal cysts and hyperaldosteronism or Cushing syndrome adenomas. Indications for bilateral adrenalectomy were hypophyseal Cushing's disease, bilateral adrenal hyperplasia, pheochromocytoma and bilateral metastases.
Technical Details of Surgical Procedures.
| Feature | No. | % |
| Partial adrenalectomies | ||
| Yes | 4 | 11 |
| No | 32 | 89 |
| Bilateral adrenalectomies | ||
| Yes | 22 | 61 |
| No | 14 | 39 |
| Number of right laparoscopic adrenalectomy ports | ||
| 4 | 34 | 100 |
| Number of left laparoscopic adrenalectomy ports | ||
| 3 | 14 | 41 |
| 4 | 20 | 59 |
| Laparoscope type | ||
| 0° | 7 | 20 |
| 30° | 15 | 44 |
| Both | 12 | 35 |
| Use of ultrasound laparoscopy | ||
| Yes | 3 | 9 |
| No | 31 | 91 |
| Use of robotic technology | ||
| Yes (Da Vinci® Surgical System) | 3 | 9 |
| No | 31 | 91 |
| Haemostatic instruments used | ||
| Vessel sealing system (Ligasure®) | 9 | 25 |
| Harmonic scalpel | 11 | 30 |
| Both | 16 | 44 |
| Use of drainage after adrenalectomy | ||
| Never | 1 | 3 |
| Occasionally | 16 | 44 |
| Generally | 8 | 22 |
| Always | 11 | 30 |
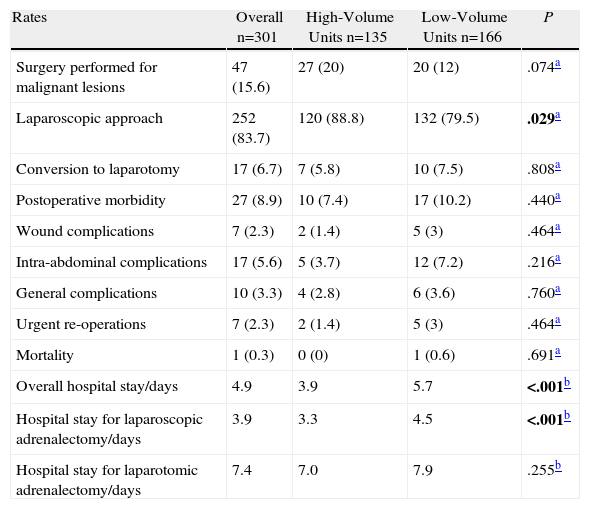
Table 6 shows the results based on the volume of activity of surgical units. It can be seen that the percentage of patients operated upon laparoscopically was significantly higher in units with a high number of cases. There were 17 patients in the series (6.7%) that required conversion to laparotomy: 8 cases of pheochromocytoma, 2 of primary aldosteronism, 2 of bilateral adrenal hyperplasia, 2 myelolipomas, 1 adenoma, 1 metastases and 1 adrenal carcinoma. The causes were haemorrhage in 8 patients, difficulty in identifying the structures in 4 cases, anaesthetic problems in 2, size of the lesion in 2, and invasion of adjacent structures (adrenal carcinoma with inferior vena cava invasion) in the last patient.
Results Related to the Volume of Activity in the Unit.
| Rates | Overall n=301 | High-Volume Units n=135 | Low-Volume Units n=166 | P |
| Surgery performed for malignant lesions | 47 (15.6) | 27 (20) | 20 (12) | .074a |
| Laparoscopic approach | 252 (83.7) | 120 (88.8) | 132 (79.5) | .029a |
| Conversion to laparotomy | 17 (6.7) | 7 (5.8) | 10 (7.5) | .808a |
| Postoperative morbidity | 27 (8.9) | 10 (7.4) | 17 (10.2) | .440a |
| Wound complications | 7 (2.3) | 2 (1.4) | 5 (3) | .464a |
| Intra-abdominal complications | 17 (5.6) | 5 (3.7) | 12 (7.2) | .216a |
| General complications | 10 (3.3) | 4 (2.8) | 6 (3.6) | .760a |
| Urgent re-operations | 7 (2.3) | 2 (1.4) | 5 (3) | .464a |
| Mortality | 1 (0.3) | 0 (0) | 1 (0.6) | .691a |
| Overall hospital stay/days | 4.9 | 3.9 | 5.7 | <.001b |
| Hospital stay for laparoscopic adrenalectomy/days | 3.9 | 3.3 | 4.5 | <.001b |
| Hospital stay for laparotomic adrenalectomy/days | 7.4 | 7.0 | 7.9 | .255b |
There were no statistically significant differences in the activity volume for hospital morbidity. After classifying them into general, intra-abdominal and lesion complications, there was no statistically significant difference either after comparing units according to their volume. General complications affected 10 patients (3.3%): with 4 cases of pneumonia, 2 decompensation of previous heart conditions, 2 urinary tract infections, 1 deep vein thrombosis and 1 multiple organ dysfunction syndrome after colorectal anastomosis dehiscence which led to the patient's death on the 15th postoperative day.
Wound complications included 4 cases of infection, 2 hernias and 1 evisceration. The most common intra-abdominal complication was haematoma in the resection bed (7 cases). There were 2 cases of sigmoid ischaemia and persistent lymphatic leakage, and one case of postoperative ileus, intra-abdominal abscess, duodenal perforation, pancreatic fistula, splenic laceration requiring splenectomy and, finally, a dehiscence of colonic anastomosis performed after segmental resection of splenic flexure, which was needed for the complete removal of an adrenal carcinoma. The latter patient and 6 others (2.3% of the total) required re-operation: there were 3 intra-abdominal haematomas, 1 ischaemia of the sigmoid colon and the cases of duodenal perforation and evisceration. As shown in Table 6, the overall average hospital stay for laparoscopic adrenalectomy was significantly lower in high-volume centres.
DiscussionIn recent years, several studies have shown an increase in the frequency of adrenalectomies performed. This is probably due to the increased detection of asymptomatic adrenal masses in imaging studies performed for other reasons, and to the widespread use of laparoscopy, which is a low morbidity approach accepted by physicians and patients.1–4 These studies conclude that the volume of activity in the surgical unit is an important factor in their results, as in other procedures and conditions.7–14
Given that only retrospective series of individual units were published in Spain, the endocrine surgery section of the AEC designed a questionnaire to determine the current state of adrenal surgery in Spain. The objective was to find out which centres, departments and surgeons performed this technique and to analyse details related to diagnosis, preoperative treatment, the surgical procedure and its results. Moreover, these data could be used as a basis for a Spanish adrenal surgery registry, similar to those developed by the Association for the laparoscopic surgery of the liver, pancreas, stomach and oesophagus, as well as for single-port laparoscopic surgery.18,19
It was distributed electronically through a secure Internet site, and the low response rate may have been influenced by not using the conventional post. Other digestive surgery surveys published recently had higher response rates: 55% in the Canadian national survey for laparoscopic colorectal surgery,20 61% in the US survey on the multimodal treatment of colorectal cancer,14 and 92% in a Saudi Arabia survey on the laparoscopic treatment of acute cholecystitis.21 Another reason for the low response rate may have been the low incidence of adrenal surgery, which is usually performed in specialised endocrine surgery or advanced laparoscopy units. In addition, many surgeons may have not received the survey due to not belonging to the AEC or due to not updating their email address. Finally, the survey was not sent to the specialist urology departments, which also routinely perform this technique. They perform up to 28% of such procedures in North America, according to the Park et al. study.3
In our study, adrenal surgery in Spain is usually performed by a small number of surgeons in endocrine surgery units in large hospitals. Due to the low incidence of these processes, only 50% of patients were operated in units that perform 10 or more procedures per year, which is similar to data from North American and European records.1–3,15 The results for the preoperative location techniques used and types of pathology intervened were also similar to these series. The pattern is fairly uniform in the responses for the preoperative preparation of pheochromocytoma. The alpha-blocker used is usually phenoxybenzamine, although doxazosin is beginning to be used in Spain, possibly due to its greater availability. Furthermore, this allows preoperative preparation to be done at home and leads to less hypotension in the postoperative period.
The laparoscopic approach was the norm, with usage figures (84%) higher than in previous studies, although some hospitals have not yet implemented the procedure. Spanish surgeons do not consider this approach to be contraindicated by previous upper abdominal surgery or a diagnosis of adrenal metastasis. However, half of them would contraindicate it for large lesions and a diagnosis of adrenal carcinoma. The nil use of the posterior or lateral retroperitoneal endoscopic approach is noteworthy, with good results in the Essen University series published by Walz et al.22 This is probably influenced by the speciality of the surgeons surveyed, who were not accustomed to this approach.
Our results show low rates for the following: conversion to laparotomy (6.7%), overall morbidity (8.9%), urgent re-operation (2.3%) and mortality (0.3%), as well as a hospital stay of 4.9 days, which is similar to data published in North American and European studies.1,15 As with other surgical fields7,14 and previous multicentre studies that describe the results of adrenal surgery,1–3,15 the influence of the volume of activity of the centre can be observed. Thus, the laparoscopic approach is used with greater frequency and shorter hospital stay in units with a higher number of cases.
The low response rate is a major limitation of our study; and indeed may have led to a response bias, with surgeons working in specialist units most likely to perform minimally invasive surgery responding more readily. However, we believe the findings are consistent with those obtained from similar studies,1–3 with the data coming from a representative sample of the Spanish surgical community giving value to the results. Moreover, this is the first European approach to this problem, apart from a Danish study.15 We believe that this initiative needs to be increasingly communicated to Spanish surgical groups, and to be used as a basis for the implementation of a national adrenal surgery registry, under the AEC.
In conclusion, our data show that adrenal surgery is performed in Spain in hospitals of varying complexity. The laparoscopic approach is standard, with good results for morbidity and hospital stay. As in previous studies, the volume of activity in the unit is a factor impacting on the results. High volume centres have carried out laparoscopic adrenalectomy more frequently and with shorter hospital stays.
Conflicts of InterestThe authors have no conflicts of interest to declare.
To all surgeons, units and departments that completed and sent the survey questionnaire to the endocrine surgery section of the AEC: Norberto Casinello Fernández (Servicio de Cirugía General, Hospital Clínico Universitario, Valencia), Elisabeth Bollo Arocena (Servicio de Cirugía General, Hospital de Donostia, San Sebastián), César Pablo Ramírez Plaza (Servicio de Cirugía General, Hospital Universitario Carlos Haya, Malaga), Nuria Muñoz Pérez (Servicio de Cirugía General, Hospital Universitario Virgen de las Nieves, Granada), Francisco Rodríguez González (Servicio de Cirugía General, Hospital Costa del Sol, Marbella, Malaga), Eduardo Domínguez-Adame Lanuza (Servicio de Cirugía General, Hospital Universitario Virgen Macarena, Sevilla), Adolfo Basáñez Amuchástegui (Servicio de Cirugía General, Hospital de Galdácano, Bilbao), Juan Sancho Inserser (Servicio de Cirugía General, Hospital del Mar, Barcelona), José Miguel del Pino Monzón (Servicio de Cirugía General, Hospital Universitario Nuestra Señora de Candelaria, Tenerife), Alejandro Flor Costa (Quirúrgica Cirujanos, Barcelona), Carmen González Sánchez (Servicio de Cirugía General, Hospital Universitario de Salamanca), José Manuel Couselo Villanueva (Servicio de Cirugía General, Hospital Xeral Calde, Lugo), Ana Carrión Tomás (Servicio de Cirugía General, Hospital General Universitario, Alicante), Mario Serradilla Martín (Servicio de Cirugía General, Complejo Hospitalario de Jaén), David Martínez Ramos (Servicio de Cirugía General, Hospital General de Castellón), Marifé Candel Arenas (Servicio de Cirugía General, Hospital Universitario Reina Sofía, Murcia), Nieves Cáceres Alvarado (Servicio de Cirugía General, Hospital Xeral Cíes, Vigo), José María Octavio de Toledo Ubieto (Servicio de Cirugía General, Hospital de Ourense), Joaquín Gómez Ramírez (Servicio de Cirugía General, Hospital Universitario de la Princesa, Madrid), Francisco Mateo Vallejo (Servicio de Cirugía General, Hospital de Jerez, Cádiz), Gonzalo Gutiérrez Fernández (Servicio de Cirugía General, Hospital Universitario Marqués de Valdecilla, Santander), Lourdes Galán Raposo (Servicio de Cirugía General, Hospital Meixoeiro, Vigo), Pedro Cascales Sánchez (Servicio de Cirugía General, Complejo Hospitalario de Albacete), José Manuel Ramia Ángel (Servicio de Cirugía General, Hospital Universitario de Guadalajara), Susana Ros López (Servicio de Cirugía General, Hospital Universitario Arnau de Vilanova, Lleida), Javier Aguiló Lucia (Servicio de Cirugía General, Hospital Lluís Alcanyís, Xátiva, Valencia), Francisco Herrera Fernández (Servicio de Cirugía General, Hospital de Santa Ana, Motril, Granada), Tomás Balsa Marín (Servicio de Cirugía General, Hospital Nuestra Señora del Prado, Talavera de la Reina, Toledo), Teresa Alves Conceiçao (Servicio de Cirugía General. Hospital Torrecárdenas, Almería).
Please, cite this article as: Villar del Moral JM, et al. Cirugía suprarrenal en España: resultados finales de una encuesta nacional. Cir Esp. 2011; 89:663–9.
Some of the information in the article was presented at the 4th Congress of the European Society of Endocrine Surgeons (ESES) held in Vienna, Austria, 13–15 May 2010, and at the 28th Congreso Nacional de Cirugía (national surgery congress) held in Madrid, Spain, 9–11 November, 2010. A preliminary analysis of the results from a small number of hospitals was published in the official ESES publication (Villar JM, Moreno P, Ortega J, Bollo E, Ramírez CP, Muñoz N, et al. Results of adrenal surgery. Data from a Spanish National Survey. Langenbecks Arch Surg. 2010;395:837–43).