A trimodal prehabilitation protocol was designed with the aim to evaluate whether it contributes to reducing postoperative morbidity, to evaluate the effect of prehabilitation on overall hospital stay, and to analyze the evolution of functional capacity before and after surgery.
MethodsA single-center observational study of patients with colorectal cancer who underwent surgery with curative intent after a trimodal prehabilitation protocol. We collected data for postoperative morbidity according to the Comprehensive Complication Index and hospital stay, which were compared with a historical matrix. Functional capacity data were also collected before and after the application of the prehabilitation protocol.
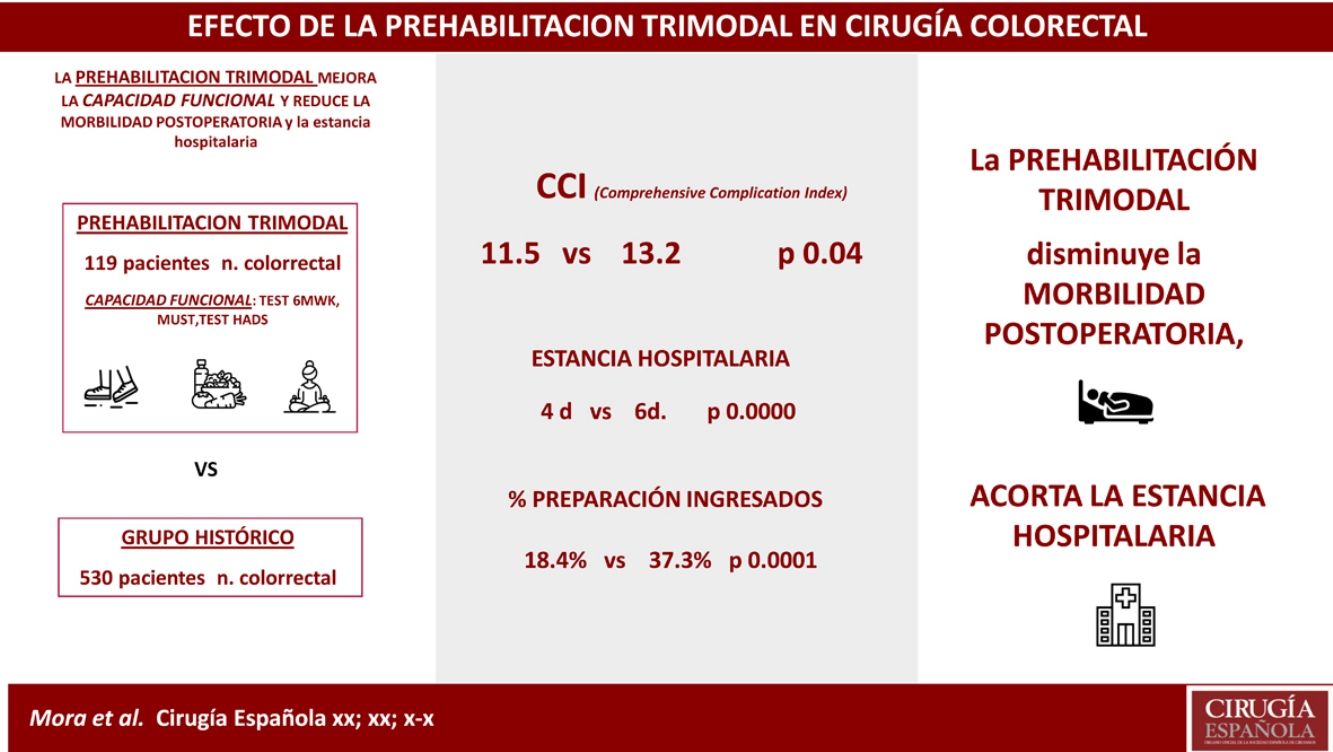
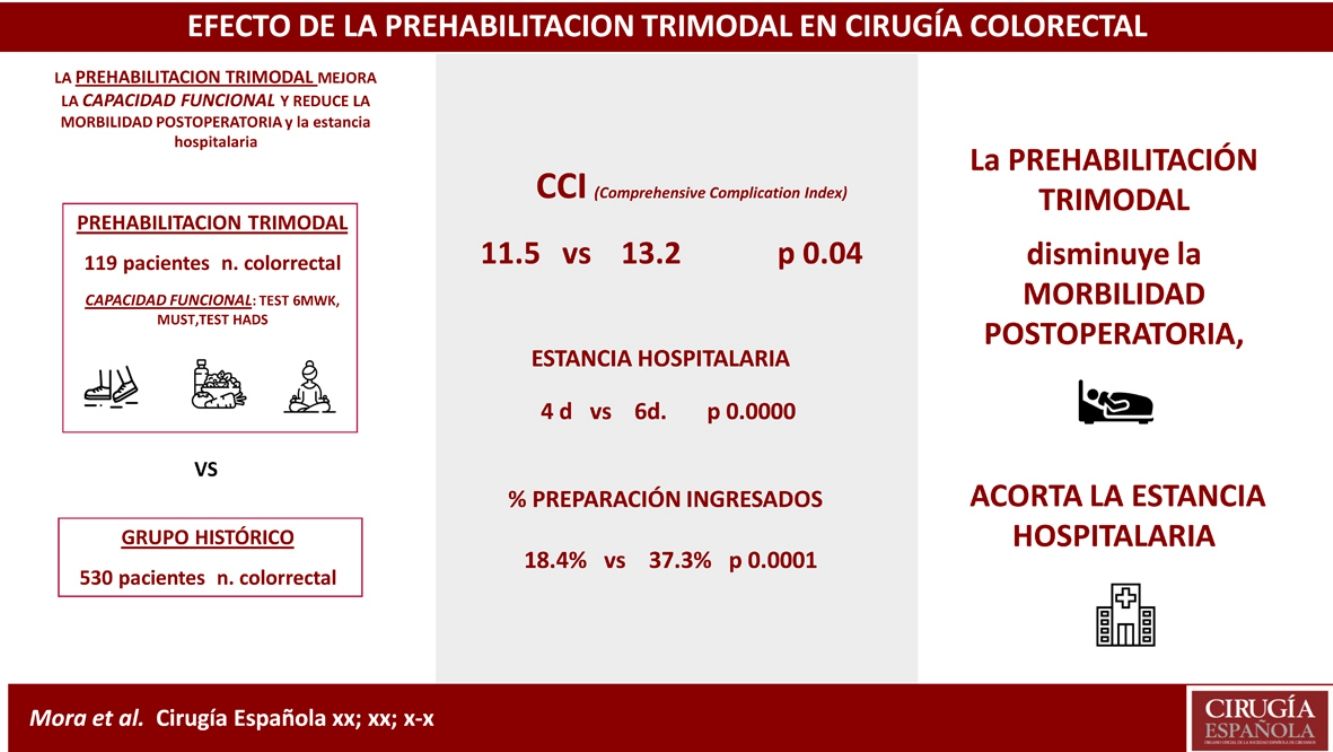
ResultsCompared to the historical population, the overall Comprehensive Complication Index was reduced from 13.2 to 11.5, which was statistically significant. Analyzed by morbidity type, all decreased in percentage, although without achieving significance (surgical site infection from 11.7% to 8.4%, nosocomial infection 15.8 to 10% and medical morbidity 8.6% to 4.2%). The overall hospital stay went from 6 to 4 days, and the decrease in the percentage of patients who prepared at home was statistically significant in both cases.
ConclusionsTrimodal prehabilitation can contribute to lowering the postoperative morbidity and overall hospital stay of patients undergoing colorectal cancer surgery.
Se ha diseñado un protocolo de prehabilitación trimodal con el objetivo de valorar si contribuye a disminuir la morbilidad postoperatoria, valorar el efecto de la prehabilitación en la estancia hospitalaria global y analizar la evolución de la capacidad funcional antes y después de cirugía.
MétodosEstudio observacional unicéntrico con pacientes con cáncer colorrectal intervenidos quirúrgicamente con intención curativa después de un protocolo de prehabilitación trimodal. Se recoge morbilidad postoperatoria según el Comprehensive Complication Index y estancia hospitalaria, y se compara con una matriz histórica. También se recoge capacidad funcional antes y después de la aplicación del protocolo de prehabilitación.
ResultadosEn comparación con la población histórica se consigue disminuir el Comprehensive Complication Index global de forma estadísticamente significativa de 13,2 a 11,5. Desglosando por tipo de morbilidad, todas disminuyen en porcentaje sin conseguir significación (infección espacio quirúrgico del 11,7 al 8,4%; infección nosocomial del 15,8 al 10%, y morbilidad médica del 8,6 al 4,2%). La estancia hospitalaria global pasa de 6 a 4 días y el porcentaje de pacientes que se preparan en casa disminuye de forma estadísticamente significativa en ambos casos.
ConclusionesLa prehabilitación trimodal puede contribuir a disminuir la morbilidad postoperatoria y la estancia hospitalaria global de los pacientes intervenidos de neoplasia colorrectal.
Despite advances in surgical and anesthetic techniques in colorectal surgery, the morbidity of these procedures continues to be significant.1 Enhanced Recovery After Surgery (ERAS)2 programs use intraoperative and postoperative measures to reduce postoperative complications, which also reduces hospital stay.3 Thus, efforts for improvement are being focused on the preparation phase of patients before surgery.
The term ‘functional capacity’ refers to the nutritional, physical and emotional state of a patient to face a stressful situation, such as a surgical procedure.4 It is believed that improved preoperative functional capacity can reduce postoperative morbidity and also improve patient recovery.
Trimodal programs appear to prepare patients to face their pathology on 3 levels: nutritional, emotional and physical. These programs are defined as prehabilitation and their positive effect has been demonstrated in other medical centers and pathologies.4–7
Our objective was to assess the effect of a trimodal prehabilitation program on overall hospital stay and to analyze the evolution of functional capacity before and after surgery in patients diagnosed with colorectal cancer who were scheduled for surgery at our hospital. As it improves functional capacity (physical, nutritional and emotional), we believe that a prehabilitation protocol can reduce postoperative morbidity while also reducing the hospital stay of patients undergoing surgery for colorectal cancer.
MethodsThe study included all patients diagnosed with colorectal cancer who were candidates for curative surgery, as determined by the Colorectal Cancer Committee.
Inclusion and exclusion criteriaInclusion criteria:
- -
Colorectal neoplasia
- -
Curative intent
- -
Scheduled surgery
- -
Informed consent
Exclusion criteria:
- -
Refusal to be included in the study
- -
Palliative intent
- -
Urgent surgery
- -
Baseline pathology that made it impossible to carry out the protocol
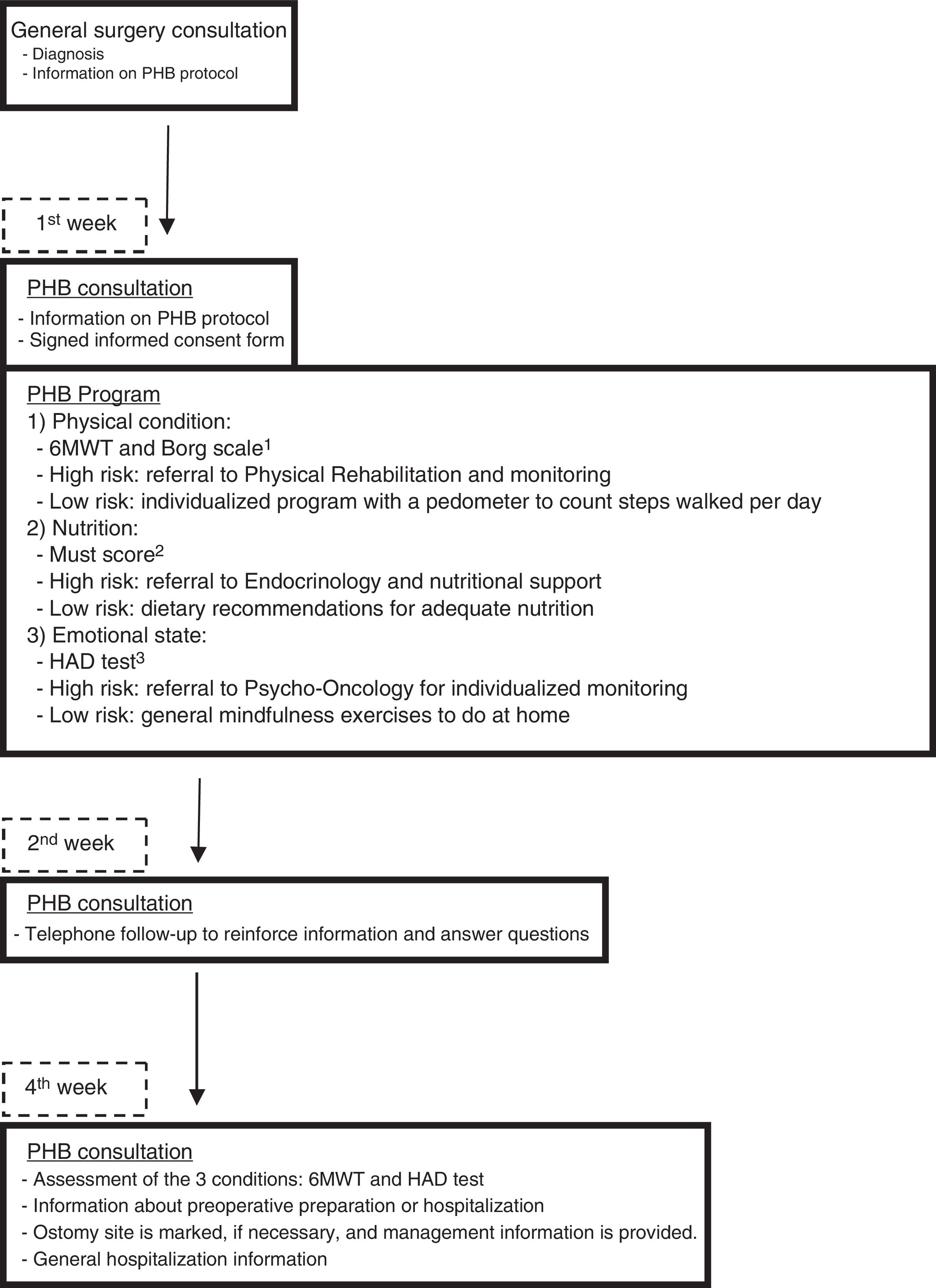
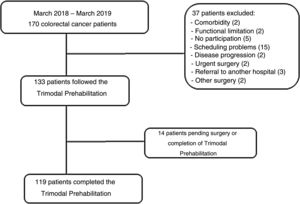
The study began in the general surgeon’s office, where the patient was informed of the diagnosis and the need for surgical intervention. The prehabilitation protocol was discussed, and a specific appointment was scheduled for the prehabilitation consultation. In this consultation, the study protocol was explained again and, once the informed consent form was signed, the patient was included in the study (Fig. 1).
The protocol began with an initial office visit for a basic preoperative assessment, and the Malnutrition Universal Screening Tool (MUST) test was administered to assess nutritional status, the HADS test was used to assess the degree of depression and anxiety of the patient, and the 6-minute walk test (6MWT) was done, after which the oxygen consumption formula was applied to determine the number of steps that the patient should walk each day (10,000 steps; between 10,000 and 7000 steps; and 7000 steps) and the patient was given a pedometer. A book was also provided with tips for high-protein shakes, exercises that could be done at home, and a link to a mindfulness resource. At the end of the book, there was space for the patient to write down the daily number of steps, daily meals, and any concerns.
The following week, a telephone consultation reinforced the explanation of the initial office visit, and any questions were answered.
One week before the intervention, the patient was seen again in the consultation, and the Hospital Anxiety and Depression Scale (HADS) test and the 6MWT were performed again to check whether there were any changes compared to the former results. Preoperative preparation was also explained, ostomy sites marked, and any questions answered about the surgical technique and hospital stay.
After at least 4 weeks of trimodal prehabilitation, the patient underwent surgery. The postoperative course followed the enhanced recovery standards of the ERAS program, which is included in the intrahospital control guidelines that have been used at our hospital since 2014.
For the analysis of the results, the following variables were collected in an ACCESS database:
- a)
Main variable: Comprehensive Complication Index (CCI). Formula that collects, with different specific weight, all the morbidity of the patient during hospital admission.8 Morbidity is collected according to the Dindo-Clavien classification.9
- b)
Secondary variables:
- 1
Demographic: age, sex, American Society of Anesthesiology (ASA) score
- 2
Measurement of functional capacity: Six-Minute Walk Test (6MWT, physiological reserve),10,11 MUST test (need for nutritional supplements)12 and the HADS test (degree of anxiety and depression).13 Need for follow-up with: physical therapist, nutritionist, psycho-oncologist.
- 3
Surgical: procedure, preoperative hospital stay, postoperative hospital stay, morbidity
- 1
The control group was a group of patients who underwent surgery for colorectal neoplasia at our center from 2014 onwards. Their data were obtained from the database that has been routinely used at our hospital since 2005.14 We define the years 2014–2017 as a control group because they are the dates during which laparoscopic techniques were considered established in 80%–90% of patients, and the ERAS guidelines2 were also being followed.
The patient is her/his own control to assess the effect of the trimodal prehabilitation protocol.
Sample sizeTo demonstrate the effectiveness of the patient population, we used the CCI with values from 0 to 100. In our population of patients treated for colorectal neoplasia since 2014, the mean CCI was 22 and the standard deviation was 18.
We proposed a 30% reduction in postoperative complications with a minimum detectable effect size of 8, an alpha error of 0.05 and a beta error of 0.002. This required 79 patients to detect clinical differences.
Statistical analysisThis was done using the SPSS program, version 21.
Descriptive analysisThe quantitative variables are described by means and standard deviation when the distribution was considered normal; otherwise, median, interquartile range and range are used.
Categorical variables are reported with absolute numbers and percentages.
Bivariate analysisThe analysis of the quantitative variables, for paired groups, was performed using the Student’s t test for paired data if they met the conditions for its application. If not, the nonparametric Wilcoxon test was used.
The variables of the HADS test were considered categorical variables. They were analyzed according to the McNemar test.
For the unpaired quantitative variables, the chi-square test was used.
A P value of <.05 was considered statistically significant.
The protocol was approved by the Ethics Committee of our hospital and was enrolled in the ClinicalTrials.gov database (ID: NCT: 03543514). All patients signed an informed consent form before entering the study.
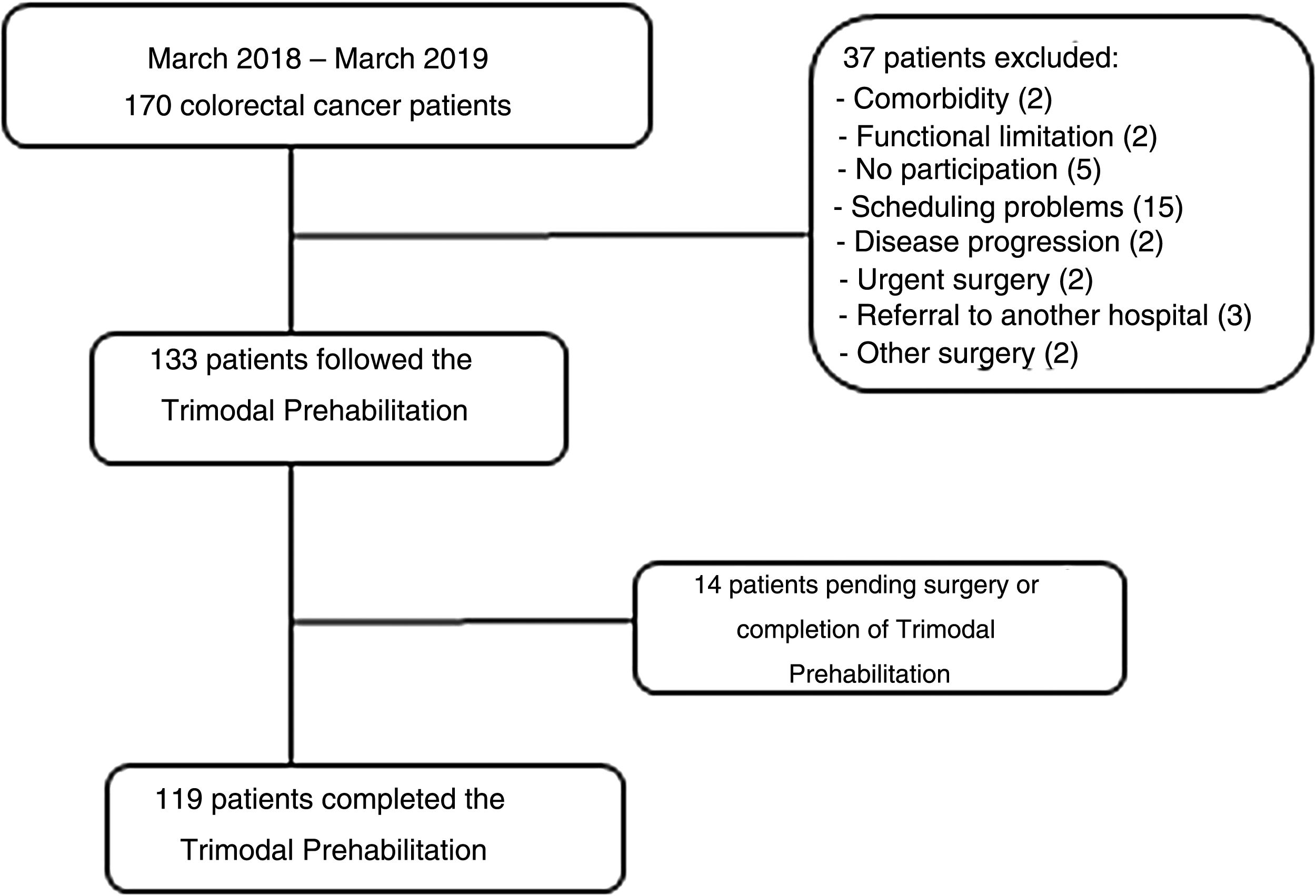
ResultsFrom March 2018 to March 2019, 170 patients were diagnosed with colorectal cancer and were candidates for surgery. One hundred and thirty-three have followed the prehabilitation program. At the time of the analysis, 14 patients were awaiting intervention and we included only 119 patients in the analysis. The reasons for exclusion can be seen in the flow chart (Fig. 2).
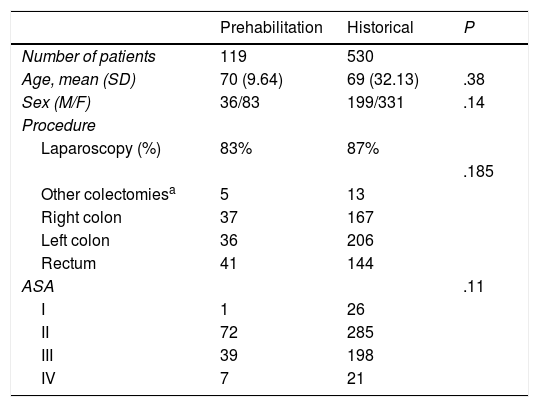
Before starting the analysis, a comparison was made between the historical population and the study population (Table 1).
Prehabilitated population characteristics and comparison with the historical population.
| Prehabilitation | Historical | P | |
|---|---|---|---|
| Number of patients | 119 | 530 | |
| Age, mean (SD) | 70 (9.64) | 69 (32.13) | .38 |
| Sex (M/F) | 36/83 | 199/331 | .14 |
| Procedure | |||
| Laparoscopy (%) | 83% | 87% | |
| .185 | |||
| Other colectomiesa | 5 | 13 | |
| Right colon | 37 | 167 | |
| Left colon | 36 | 206 | |
| Rectum | 41 | 144 | |
| ASA | .11 | ||
| I | 1 | 26 | |
| II | 72 | 285 | |
| III | 39 | 198 | |
| IV | 7 | 21 |
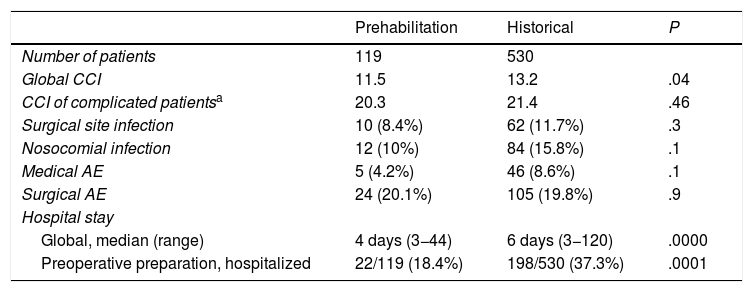
The global CCI in the prehabilitation group (11.5) was lower than that of the historical group (13.2), with statistically significant differences (P=.04). The CCI of complicated patients was lower among the prehabilitation group (20.3) compared to the historical one (21.4) with no statistically significant differences.
Morbidity analysisSurgical adverse effects (AE) did not vary when the 2 groups were compared. In the remaining morbidities, a decrease was observed in the prehabilitation group, without being statistically significant (Table 2).
Morbidity results of the prehabilitation group and comparison with the historical population.
| Prehabilitation | Historical | P | |
|---|---|---|---|
| Number of patients | 119 | 530 | |
| Global CCI | 11.5 | 13.2 | .04 |
| CCI of complicated patientsa | 20.3 | 21.4 | .46 |
| Surgical site infection | 10 (8.4%) | 62 (11.7%) | .3 |
| Nosocomial infection | 12 (10%) | 84 (15.8%) | .1 |
| Medical AE | 5 (4.2%) | 46 (8.6%) | .1 |
| Surgical AE | 24 (20.1%) | 105 (19.8%) | .9 |
| Hospital stay | |||
| Global, median (range) | 4 days (3−44) | 6 days (3−120) | .0000 |
| Preoperative preparation, hospitalized | 22/119 (18.4%) | 198/530 (37.3%) | .0001 |
AE: adverse effect.
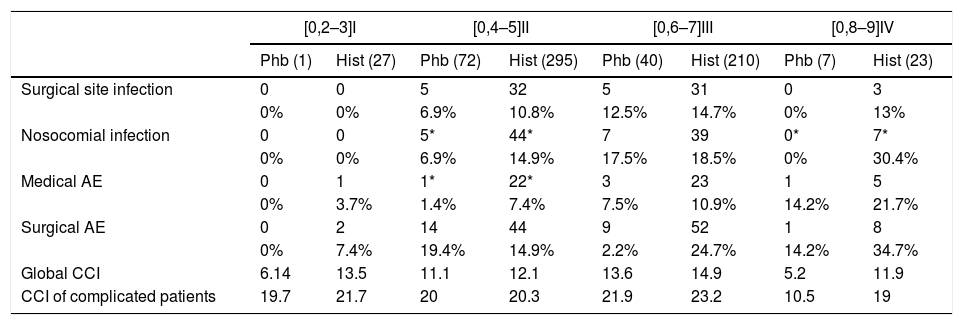
We separated the groups according to the ASA (Table 3). In all, there were differences between the historical and prehabilitation groups, in favor of the latter. These differences were only statistically significant in the ASA II group in the nosocomial AE and medical AE, and in ASA IV in the nosocomial AE.
Analysis of the morbidity results according to ASA group.
| [0,2–3]I | [0,4–5]II | [0,6–7]III | [0,8–9]IV | |||||
|---|---|---|---|---|---|---|---|---|
| Phb (1) | Hist (27) | Phb (72) | Hist (295) | Phb (40) | Hist (210) | Phb (7) | Hist (23) | |
| Surgical site infection | 0 | 0 | 5 | 32 | 5 | 31 | 0 | 3 |
| 0% | 0% | 6.9% | 10.8% | 12.5% | 14.7% | 0% | 13% | |
| Nosocomial infection | 0 | 0 | 5* | 44* | 7 | 39 | 0* | 7* |
| 0% | 0% | 6.9% | 14.9% | 17.5% | 18.5% | 0% | 30.4% | |
| Medical AE | 0 | 1 | 1* | 22* | 3 | 23 | 1 | 5 |
| 0% | 3.7% | 1.4% | 7.4% | 7.5% | 10.9% | 14.2% | 21.7% | |
| Surgical AE | 0 | 2 | 14 | 44 | 9 | 52 | 1 | 8 |
| 0% | 7.4% | 19.4% | 14.9% | 2.2% | 24.7% | 14.2% | 34.7% | |
| Global CCI | 6.14 | 13.5 | 11.1 | 12.1 | 13.6 | 14.9 | 5.2 | 11.9 |
| CCI of complicated patients | 19.7 | 21.7 | 20 | 20.3 | 21.9 | 23.2 | 10.5 | 19 |
* P>.005.
Functional capacity:
- -
Physiological status: 20 patients had an indication for referral to physical therapy. We found differences with improvement in the second test compared to the first (P= .96).
- -
Nutritional status: the MUST test showed that most patients were well nourished. Only 2 of the 119 patients need nutrition monitoring.
- -
Psychological state: according to the HADS test, the degree of anxiety and depression decreased compared to the initial test (anxiety: P= .14; depression: P= .73). The psychology resource was not started until 5 months before the end of the study, and only 4 of the 19 patients who needed were referred.
The overall hospital stay was reduced (P=.000) with a median of 6 days to 4 days in favor of the prehabilitation group.
The group of patients who performed preoperative preparation at home increased (P=.0001) in the prehabilitation group.
DiscussionPrehabilitation is a set of care measures that begins once cancer is diagnosed. It includes physical and psychological evaluations that determine a functional baseline, identify deficiencies, and provide interventions that improve physical and psychological health to reduce the incidence or severity of future deterioration.15 These processes imply a change for medical professionals, who must care for the patient once the pathology has been diagnosed and attempt to improve their comorbidities as well as their functional capacity. As for patients, it means they become an active part of the process of preparing for the treatment of their disease.
These protocols involve creation of multidisciplinary circuits where professionals from different services collaborate. These professionals must understand the purpose of their contribution and must be well coordinated. On the other hand, the collaboration of hospital administrators is also necessary, as certain resources need to be approved. As we see in our case, there are parts of the protocol that have not been able to be applied in their entirety.
Despite the deficiencies, we have achieved encouraging results that allow us to continue with the protocol and defend its improvement and implementation in other pathologies. The global CCI has been reduced in a statistically significant manner in the group undergoing prehabilitation. The percentages of nosocomial, surgical site and medical AE also decreased in the prehabilitation group, although without achieving statistically significant differences. We always talk about statistically significant differences, but if we give a clinical sense to the results, we can observe that all-type morbidity is lower in the prehabilitation group.
According to the studies evaluated, prehabilitation presents better results in ASA III patients.11 In our group, we found statistically significant differences in medical AE and nosocomial infection in ASA II patients, and in nosocomial infection AE in ASA IV. For the ASA II, this may be due to the type of prehabilitation performed or because the group of ASA IV patients was very small.
Where statistically significant differences are achieved is in the reduction of the hospital stay, both pre- and postoperative, of prehabilitation patients. The median postoperative stay was 6 days in the historical group, which dropped to 4 days in the prehabilitation group. In addition, fewer patients were admitted to prepare for surgery. This may be due to the fact that the patients are seen more times and, therefore, are better informed and more confident to carry out the preparation at home. This decrease in hospital stay represents a significant cost reduction.
Study limitations: this is a pilot study. We compared the study population with a historical group. When these comparisons are made, there is a recognized limitation in the results obtained. Therefore, we have tried to reduce it as much as possible by analyzing patient demographic characteristics and surgical procedures; also, the percentage of laparoscopy and the in-hospital control protocol were the same in the 2 groups. We have not been able to perform a complete protocol. In spite of everything, we have shown that patients do not decrease their physical capacity during the period from the diagnosis of the disease to the surgery; and that the rate of complications through CCI is lower and statistically significant in prehabilitation patients. All this manages to reduce the overall hospital stay of patients following the prehabilitation protocol, with the savings that this entails.
In conclusion, trimodal prehabilitation is able to contribute towards reducing postoperative morbidity and overall hospital stay in patients undergoing colorectal cancer surgery. It involves a change in the preoperative preparation of patients. Future studies will show that prehabilitation has a beneficial effect on not only preoperative management, but on any patient treatment.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Mora López L, Pallisera Llovera A, Serra-Aracil X, Serra Pla S, Lucas Guerrero V, Rebasa P, et al. Estudio observacional prospectivo unicéntrico sobre el efecto de la prehabilitación trimodal en cirugía colorrectal. Cir Esp. 2020;98:605–611.