Duodenal perforations after endoscopic retrograde cholangiopancreatography (ERCP) are an uncommon complication. The management of this kind of perforation is controversial. The aim of this study was to analyze the results of the management of a series of 15 patients who were diagnosed with this complication.
MethodsRetrospective study of duodenal perforations after ERCP diagnosed at a tertiary level hospital, between 2001 and 2011. The variables age, sex, ERCP indication, type of perforation, time of diagnosis, clinical presentation, radiographic findings, management, surgical technique, length of stay and intrahospital mortality were recorded and analyzed.
ResultsOut of a total of 1923 ERCP performed, 15 duodenal perforations were detected (0.78%). Perforation site was the duodenal wall (3 cases) and periampullary (12 cases). Eleven perforations were suspected during the procedure. Patients with duodenal wall perforations underwent immediate surgery. Seven of 12 periampullary perforations were managed conservatively with a favourable outcome in 5 of them. Subsequent scheduled surgery was performed in 4 cases. The mean length of hospital stay was 21.2 days (range: 3–49) and intrahospital mortality was 20%.
ConclusionsPerforations after ERCP have high mortality rates, and require a complicated therapeutic approach that needs to be individualized. Selective conservative management is a valid and safe option in selected patients.
La perforación duodenal tras colangiopancreatografía retrógrada endoscópica (CPRE) constituye un cuadro infrecuente. Su manejo es controvertido. El objetivo de este estudio fue analizar los resultados obtenidos en función de su manejo en una serie de 15 pacientes en los que se diagnosticó esta complicación.
MétodosEstudio descriptivo retrospectivo de las perforaciones duodenales tras CPRE, diagnosticadas en un hospital de tercer nivel entre el 2001 y el 2011. Se analizaron las siguientes variables: edad; sexo; motivo de la CPRE; tipo de perforación; momento del diagnóstico; clínica; prueba de imagen; manejo inicial; técnica quirúrgica; estancia global y mortalidad.
ResultadosDe un total de 1.923 CPRE realizadas se identificaron 15 perforaciones duodenales tras el procedimiento (0,78%). La localización de la perforación fue en la pared duodenal, lejos de la papila (3 casos) y periampulares (12 casos). En 11 pacientes el diagnóstico se sospechó durante el procedimiento. Las perforaciones de pared duodenal se trataron con cirugía urgente. En 7 de las 12 perforaciones periampulares se realizó manejo conservador inicial con evolución favourable en 5 de ellas. En 4 pacientes se realizó cirugía programada posterior. La estancia media hospitalaria fue de 21,2 días (rango: 3–49) y la mortalidad global del 20%.
ConclusionesLas perforaciones tras CPRE constituyen un cuadro de elevada mortalidad, difícil diagnóstico y complicado abordaje terapéutico que precisa ser individualizado. El manejo conservador selectivo constituye una opción válida y segura.
The perforation of the digestive tract after endoscopic retrograde cholangiopancreatography (ERCP) is a rare complication; however, it is associated with a high mortality rate that fluctuates from 8% to 23%, related to a late diagnosis and treatment.1 Its low incidence varies from 0.3% to 2.1%.1–3 Therefore, the treatment is based on studies with a low level of evidence. Even though the therapeutic management has been traditionally surgical, there have been publications of some series that support the utilization of conservatory measures in selected patients. Thus, several authors have suggested classifications based on its location and injury mechanism4,5 that, together with clinical and radiological findings, can contribute to a correct selection of these patients. This study describes the results obtained according to its management in a series of patients diagnosed with this complication.
Materials and MethodsA descriptive, retrospective and uni-centre study was conducted on duodenal perforations after ERCP that took place in a reference hospital during the period between January 2001 and December 2011. This hospital takes care of a population of 333572 inhabitants and has 702 beds. Seventeen patients were identified with a perforation in the digestive tract as a complication during the endoscopic procedure. These patients were registered in the databases of the General Surgery Service and the Digestive Service. Two cases were excluded. One with an oesophageal perforation and the other one with a jejunal perforation and history of Billroth II gastrectomy. Finally, the study included 15 patients who suffered a duodenal perforation as a complication of ERCP. The study was approved by the Ethics Committee of the institution (code 130067).
The following data were registered: age, gender, comorbidity, indication of endoscopic procedure, time of diagnosis and imaging tests used, time of symptoms appearance and period elapsed until surgery, symptomatology, findings during surgery and type of surgical procedure performed. The perforations were classified retrospectively as: (a) duodenal wall, far from papilla; (b) periampullary, related to the sphincterotomy; and (c) of the bile duct, due to the equipment, according to the proposal made by Howard et al.5 and Stapfer et al.4 Furthermore, it was also considered whether risk factors of perforation existed, such as juxta-diverticular papilla, precut6 or papilla stenosis. Finally, stay in the Reanimation/Intensive care Unit was evaluated, and also overall length of hospital stay and mortality.
In case of suspected post-ERCP perforation, the patient was studied by the General Surgery on-call team. The initial procedure, urgent surgery or conservative treatment, was based on findings during ERCP, symptomatology, clinical severity of the patient, performed diagnostic tests and judgement of the team on call. Conservative-managed patients were treated with serum therapy, nasogastric tube, intravenous wide-spectrum antibiotic therapy and nil by mouth.
The results obtained were studied by means of the SPSS statistical package for Mac OS, v. 20.0 (SPSS Inc., Chicago, IL, USA). The quantitative variables were described through the mean, standard deviation, and range. Qualitative variables were described using frequency and percentages.
ResultsDuring the assessment period, 1923 ERCP were performed in our institution. Fifteen patients suffered duodenal perforation (0.78%), 3 males and 12 females, with mean age 68.5±22.5 years (range: 21–91).
There were 3 duodenal wall perforations and 12 periampullary perforations. ERCP indications were mostly due to benign disease of bile duct. Eight patients had choledocholithiasis, 4 of them with cholangitis; 4 patients had cholestasis, 2 of them related to cholecystitis; 2 patients had malignant obstructive jaundice, one of them also had associated cholangitis; finally, a patient presented a papillary haemorrhage after a previous sphincterotomy.
In 12 patients, some risk factor of perforation was observed during the procedure, while 3 of them presented 2 risk factors. Precut and peridiverticular papilla were the most frequent risk factors, and they were present in 8 and 4 patients respectively. In addition, 2 patients suffered papilla stenosis and, in one of them, an extension of a previous sphincterotomy was performed.
In 11 patients, diagnosis of perforation was made during the procedure, in 3 patients between 12 and 48h and, in another patient, 4 days after ERCP. The clinical presentation was variable. Six patients presented abdominal pain, 3 of them with peritoneal irritation, 2 with thoracic pain, and one of them with pain radiating to the shoulder. Four patients presented sepsis signs, 3 patients presented subcutaneous emphysema, with respiratory failure, and 2 of them required immediate intubation. Neutrophilia was the most frequent finding in blood tests (8 patients), followed by leukocytosis (4 patients), metabolic acidosis (one patient), and anaemia with 5g/dl haemoglobin in the patient with papillary haemorrhage.
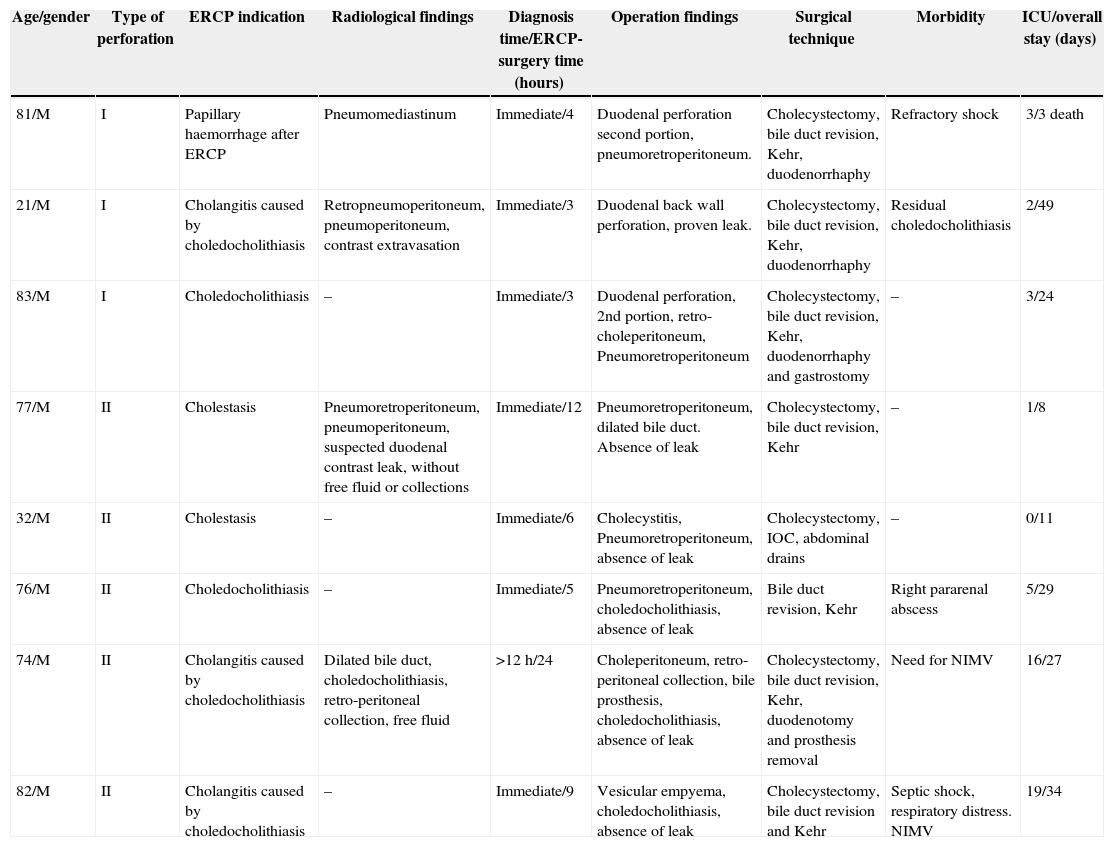
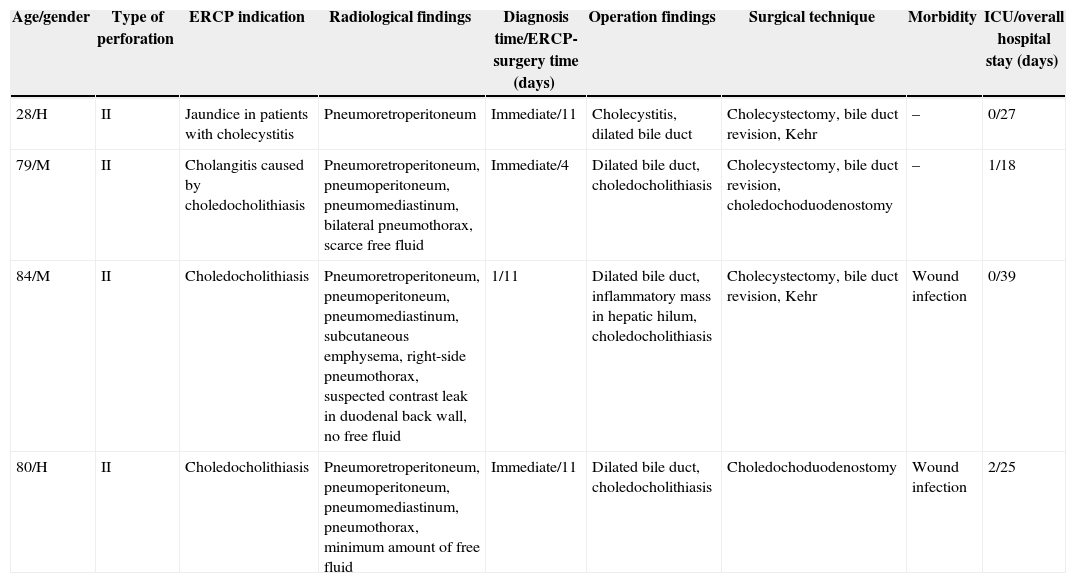
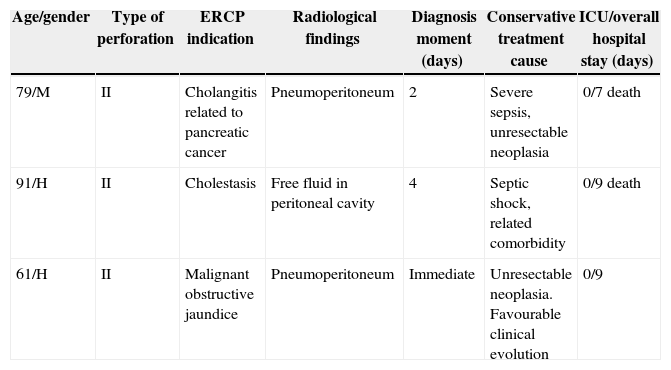
The diagnosis was confirmed during the complementary imaging test in 11 patients. In the remaining patients, the diagnosis was based on ERCP findings. Abdominal CT scan was the most frequently requested test (7 cases). In 3 patients, standing chest X-ray was conclusive. Abdominal ultrasound scan was requested in a single occasion, in which free intra-abdominal fluid was observed. Patients’ characteristics are listed in Tables 1–3.
Characteristics of Patients With Initial Surgical Treatment.
| Age/gender | Type of perforation | ERCP indication | Radiological findings | Diagnosis time/ERCP-surgery time (hours) | Operation findings | Surgical technique | Morbidity | ICU/overall stay (days) |
|---|---|---|---|---|---|---|---|---|
| 81/M | I | Papillary haemorrhage after ERCP | Pneumomediastinum | Immediate/4 | Duodenal perforation second portion, pneumoretroperitoneum. | Cholecystectomy, bile duct revision, Kehr, duodenorrhaphy | Refractory shock | 3/3 death |
| 21/M | I | Cholangitis caused by choledocholithiasis | Retropneumoperitoneum, pneumoperitoneum, contrast extravasation | Immediate/3 | Duodenal back wall perforation, proven leak. | Cholecystectomy, bile duct revision, Kehr, duodenorrhaphy | Residual choledocholithiasis | 2/49 |
| 83/M | I | Choledocholithiasis | – | Immediate/3 | Duodenal perforation, 2nd portion, retro-choleperitoneum, Pneumoretroperitoneum | Cholecystectomy, bile duct revision, Kehr, duodenorrhaphy and gastrostomy | – | 3/24 |
| 77/M | II | Cholestasis | Pneumoretroperitoneum, pneumoperitoneum, suspected duodenal contrast leak, without free fluid or collections | Immediate/12 | Pneumoretroperitoneum, dilated bile duct. Absence of leak | Cholecystectomy, bile duct revision, Kehr | – | 1/8 |
| 32/M | II | Cholestasis | – | Immediate/6 | Cholecystitis, Pneumoretroperitoneum, absence of leak | Cholecystectomy, IOC, abdominal drains | – | 0/11 |
| 76/M | II | Choledocholithiasis | – | Immediate/5 | Pneumoretroperitoneum, choledocholithiasis, absence of leak | Bile duct revision, Kehr | Right pararenal abscess | 5/29 |
| 74/M | II | Cholangitis caused by choledocholithiasis | Dilated bile duct, choledocholithiasis, retro-peritoneal collection, free fluid | >12h/24 | Choleperitoneum, retro-peritoneal collection, bile prosthesis, choledocholithiasis, absence of leak | Cholecystectomy, bile duct revision, Kehr, duodenotomy and prosthesis removal | Need for NIMV | 16/27 |
| 82/M | II | Cholangitis caused by choledocholithiasis | – | Immediate/9 | Vesicular empyema, choledocholithiasis, absence of leak | Cholecystectomy, bile duct revision and Kehr | Septic shock, respiratory distress. NIMV | 19/34 |
IOC: intraoperative cholangiogram; NIMV: non-invasive mechanic ventilation.
Characteristics of Patients Treated by Conservative Methods and Subsequently Operated on.
| Age/gender | Type of perforation | ERCP indication | Radiological findings | Diagnosis time/ERCP-surgery time (days) | Operation findings | Surgical technique | Morbidity | ICU/overall hospital stay (days) |
|---|---|---|---|---|---|---|---|---|
| 28/H | II | Jaundice in patients with cholecystitis | Pneumoretroperitoneum | Immediate/11 | Cholecystitis, dilated bile duct | Cholecystectomy, bile duct revision, Kehr | – | 0/27 |
| 79/M | II | Cholangitis caused by choledocholithiasis | Pneumoretroperitoneum, pneumoperitoneum, pneumomediastinum, bilateral pneumothorax, scarce free fluid | Immediate/4 | Dilated bile duct, choledocholithiasis | Cholecystectomy, bile duct revision, choledochoduodenostomy | – | 1/18 |
| 84/M | II | Choledocholithiasis | Pneumoretroperitoneum, pneumoperitoneum, pneumomediastinum, subcutaneous emphysema, right-side pneumothorax, suspected contrast leak in duodenal back wall, no free fluid | 1/11 | Dilated bile duct, inflammatory mass in hepatic hilum, choledocholithiasis | Cholecystectomy, bile duct revision, Kehr | Wound infection | 0/39 |
| 80/H | II | Choledocholithiasis | Pneumoretroperitoneum, pneumoperitoneum, pneumomediastinum, pneumothorax, minimum amount of free fluid | Immediate/11 | Dilated bile duct, choledocholithiasis | Choledochoduodenostomy | Wound infection | 2/25 |
Characteristics of Patients Treated by conservative Methods and Without Intervention.
| Age/gender | Type of perforation | ERCP indication | Radiological findings | Diagnosis moment (days) | Conservative treatment cause | ICU/overall hospital stay (days) |
|---|---|---|---|---|---|---|
| 79/M | II | Cholangitis related to pancreatic cancer | Pneumoperitoneum | 2 | Severe sepsis, unresectable neoplasia | 0/7 death |
| 91/H | II | Cholestasis | Free fluid in peritoneal cavity | 4 | Septic shock, related comorbidity | 0/9 death |
| 61/H | II | Malignant obstructive jaundice | Pneumoperitoneum | Immediate | Unresectable neoplasia. Favourable clinical evolution | 0/9 |
The average hospitalization time was 21.3±13.4 days (range: 3–49) and mortality rate was 20% (3 patients).
The treatment was initially surgical in 8 patients and conservative in the remaining 7.
Initial Surgical ManagementEight out of 15 patients were operated on (Table 1). All the patients underwent a cholecystectomy (except one of them, who had already undergone cholecystectomy) and intraoperative cholangiogram. In the event of evidenced choledocholithiasis, we proceeded with a choledochotomy, calculus removal and a Kehr drain placement. Three patients with type I perforation underwent a duodenorrhaphy in monoplane with interrupted sutures. In 5 patients with type II perforations, the perforation area was not found. A systematic drain was used. The postoperative period was slow but favourable in most of the patients. Two of them required prolonged orotracheal intubation due to respiratory distress, with subsequent need for non-invasive mechanical ventilation (NIMV); one patient developed a right pararenal abscess treated with percutaneous drain, while another patient presented residual choledocholithiasis. The patient with papillary haemorrhage after previous ERCP passed away 3 days after surgery due to refractory shock and multiple organ failure. The average stay in the Intensive Care Unit was 7 days (range: 1–19) and the overall stay was 23±15 days (range: 3–49). The mortality rate was 12.5% (one case).
Initial Conservative ManagementSeven patients were initially treated in a conservative manner. In 4 patients, imaging tests did not show extravasation of significant contrast, with good clinical evolution and scheduled intervention for cholecystectomy and in order to treat non-resolved choledocholithiasis (Table 2). Two patients had a choledochoduodenostomy. The other 2 patients underwent bile duct revision with choledochotomy, calculus removal and Kehr drain. There were 2 surgical wound infections.
A patient diagnosed during the procedure with unresectable neoplasia presented a favourable evolution with conservative treatment and discharge. Two patients had a late diagnosis of sepsis, and a conservative attitude was adopted due to unresectable neoplasia or old age with relevant comorbidity. Both of them passed away due to septic shock and multiple organ failure (Table 3).
Average hospital stay in the ICU was 1.5±0.7 days (range: 1–2), overall hospital stay was 19.2±12 days (range: 7–39) and mortality was of 28.5% (2 cases).
DiscussionERCP combined with endoscopic sphincterotomy is currently a relevant tool for biliopancreatic disease management.1 Even though it is considered a safe technique, ERCP has become a mere therapeutic technique due to its invasive nature, together with the introduction of cholangiography or echoendoscopy.
The most frequent post-ERCP complications are pancreatitis, perforation, haemorrhage and cholangitis,3 and others have already been mentioned but are less frequent, such as subcapsular liver haematoma7 or intestinal obstruction.8 In the multicentre studies published by Freeman et al.3 and Williams et al.,9 these complications were presented in 9.8% and 5% of the patients, respectively. In our series, post-ERCP duodenal perforations, the subject of our study, were present in 0.78% of the patients, with a mortality rate of 20%. These data are similar to the ones referred by Machado1 in his review.
Several authors4,5 have classified post-ERCP perforations by their location, injury mechanism and severity. Type I perforations, of the duodenal wall, far from papilla, are caused by the endoscopy passage and are usually diagnosed during the procedure. Type II perforations, periampullary, are usually related to the procedure difficulty, and they take place at the moment of the precut or sphincterotomy. Type III perforations, in the bile duct, tend to be caused by guideline manipulation, Dormia basket or during stent placement. In our series, as other authors describe,5,10–12 periampullary perforations are more frequent. They took place in 80% of the patients; however, there was no evidence of any perforation at the bile duct level. Nevertheless, authors like Howard et al.5 and Wu et al.12 refer to 23% and 35% of bile duct perforations, respectively.
The suspicion of perforation during the procedure is a relevant factor to achieve an early diagnosis and decide which patients will benefit from a conservative treatment. It allows treatment to begin as early as possible and it is related to the better morbidity and mortality results,1,5,12,13 contrary to late diagnosis. Four of our patients had a late diagnosis and 3 of them presented a worse clinical course. Two patients were diagnosed with sepsis 2 and 4 days after the procedure, and passed away after 7 and 9 days, respectively. One patient, diagnosed after 12h and urgently operated on, presented a retroperitoneal collection and choleperitoneum. Therefore, she required an admission in the ICU. Patients with retroperitoneal collections seem to have a worse prognosis and should require urgent surgical intervention.4,12 Such a feature was present in the aforementioned patient.
80% of the patients suffered some risk factor of perforation during the procedure. The identification may alert the physician in order to attempt to reduce the risk.14 The following have been considered as risk factors of perforation: alteration of biliodigestive anatomy, sphincterotomy length, periampullary diverticula, precut, stenosis or dilated bile duct, papillary stenosis, sphincter of Oddi dysfunction and difficulty and longer duration of the procedure.3,9 With the aim to reduce perforation risk, new precut techniques are being introduced, such as transpancreatic precut sphincterotomy or balloon dilation of the papilla.14–16
Some studies consider sphincter of Oddi dysfunction as the most frequent indication related to digestive perforation.5,17 However, choledocholithiasis was the most frequent indication (53%) in our patients. Such data are also similar to other studies.4,11,12,18,19
Abdominal CT scan is considered the most useful diagnostic method for this complication.1 Furthermore, it is considered essential for all those patients that may be eligible for a conservative management,18 just as it was performed with our patients. All of our cases presented retropneumoperitoneum, though Genszlinger et al.20 state that a radiological retropneumoperitoneum can be observed without clinical impact even in 29% of the asymptomatic patients treated with ERCP. The presence of massive subcutaneous emphysema, pneumomediastinum or pneumothorax has been defined as a predictive sign of probable bad evolution with conservative treatment.4 However, 2 patients with these characteristics and conservative management in our series had a good subsequent evolution, as well as the results obtained by Fujii et al.21
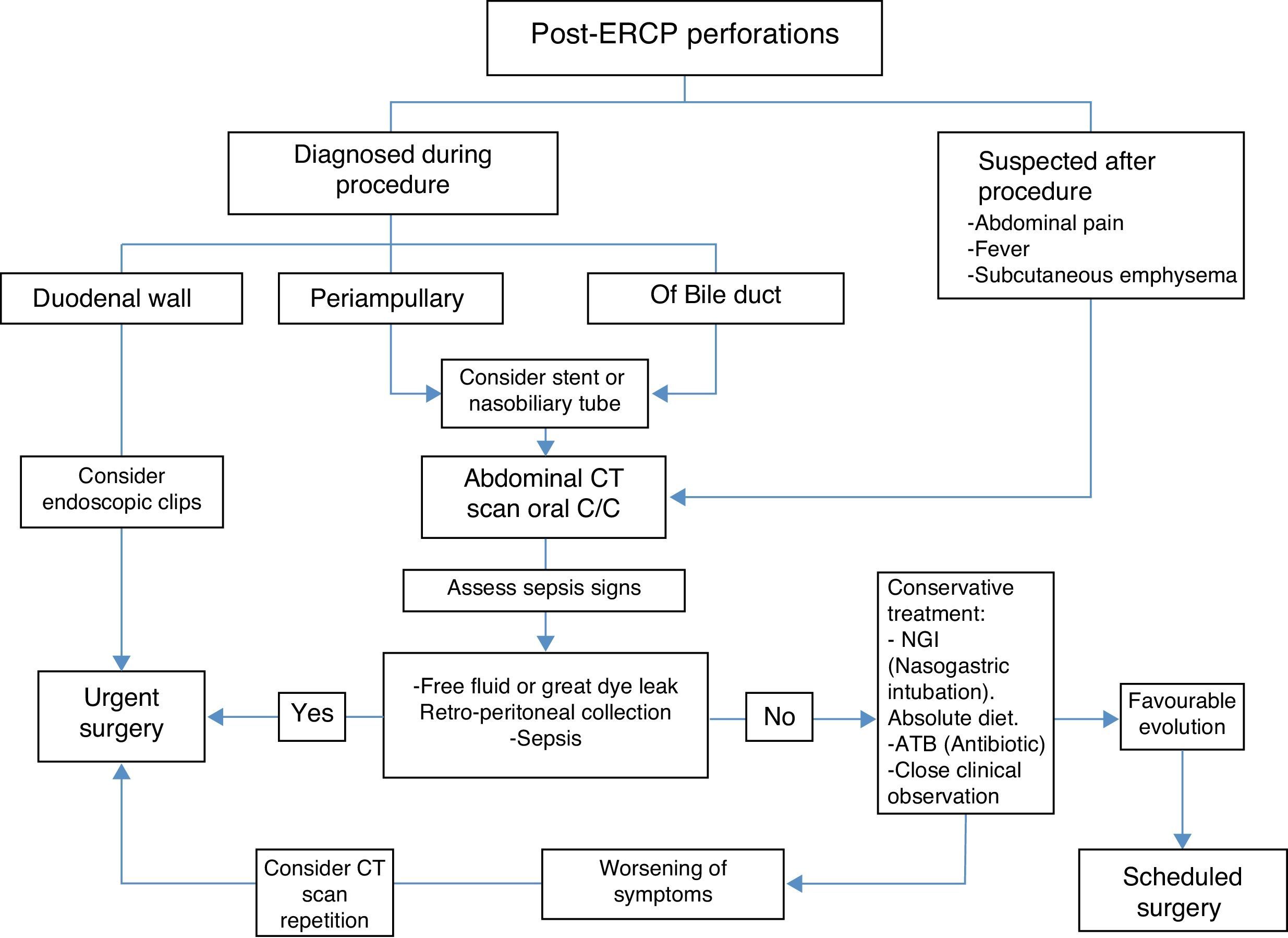
The management of post-ERCP perforation is controversial. Some authors support an early surgical management.6,22 However, an increasing number of authors prefer a selective conservative management1,4,5,10,17,18 considering the perforation type and location, as well as overall condition of the patient. In our environment, the decision to adopt a conservative treatment or a surgical treatment was based on findings observed during ERCP, the symptoms of patients and complementary tests.
It is worldwide accepted that the patients with intraperitoneal duodenal perforations must undergo surgery immediately. The surgical technique shall depend on the size of perforation, duodenal condition and clinical situation of the patient. The 3 patients with type I duodenal perforations were early diagnosed and operated on, which allowed a simple closure of the duodenal defect. Other surgical alternatives are duodenostomy, pyloric exclusion with gastrojejunostomy or feeding jejunostomy.4,10,12 Some authors have suggested the usage of endoscopic clips or endoloops11,14,23,24 with suitable resources and enough experience.
The management of periampullary perforations is a matter of discussion. Seven out of 12 periampullary perforations were treated conservatively. Nevertheless, Howard et al.5 and Li et al.11 registered conservative management rates close to 100%. Some supportive arguments are the scarce findings during the surgical intervention, without identification of perforation in most of the cases.13,16 Five patients evolved favourably and, conservative treatment failed in 2 patients. However, in the latter, the decision was based on old age or the existence of an inoperable neoplasia. In other series, the conservative management rate exceeds 60%, with a success rate over 90%.1
From the 5 patients with periampullary perforations urgently operated on, the place of perforation was not found in any of them, not even after methylene blue instillation. Perhaps, some of these patients could have been eligible for the conservative treatment of the perforation. However, this statement should be cautiously made due to the retrospective character of the study. Miller et al.25 consider that periampullary perforations would take advantage of early surgery, with pyloric exclusion with gastrojejunostomy and bile drainage as the most adequate technique. Other authors5,14,17 suggest the use of self-expandable stents or nasobiliary tubes for the treatment of periampullary perforations diagnosed during the procedure.
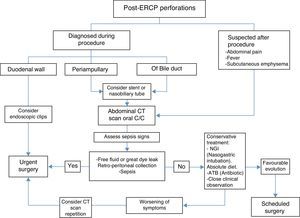
Over the years, there has been a change in the treatment of post-ERCP perforations, with selective conservative treatment as the current trend. Considering our experience as well as other authors experience,1 we could conclude that, as a general rule, patients with type I duodenal perforation will require immediate surgery, with variations in the surgical technique at the moment of diagnosis, duodenal condition and the symptoms of the patient. Patients with periampullary or bile duct perforation can be considered for a selective conservative treatment. The following are supportive factors: early diagnosis, absence of sepsis and collections, free intra-abdominal fluid or great leak of oral dye in abdominal CT scan. Besides, patients that undergo a conservative management may benefit from subsequent elective surgery with lower morbidity and mortality rates. The use of endoscopic techniques is currently soaring (Fig. 1).
Authors’ ContributionMaría Desirée Armas Ojeda and Joaquín Marchena Gómez designed the study and analysed and interpreted the results along with Vanesa Ojeda Marrero, José Carlos Cabrera Marrero, María del Pino Mathías Gutiérrez, and Daniel Ceballos Santos, who also helped María Desirée Armas Ojeda with the acquisition and gathering of data. The article was drafted by María Desirée Armas Ojeda, Vanesa Ojeda Marrero and Cristina Roque Castellano, while María Desirée Armas Ojeda, Cristina Roque Castellano and Joaquín Marchena Gómez critically reviewed the article and were responsible for the final version approval.
Conflict of InterestThe authors declare that there are no conflicts of interest.
Please cite this article as: Armas Ojeda MD, Ojeda Marrero V, Roque Castellano C, Cabrera Marrero JC, Mathías Gutierrez MP, Ceballos Santos D, et al. Perforaciones duodenales tras colangiopancreatografía retrógrada endoscópica. Cir Esp. 2015;93:403–410.
Please cite this article as: Armas Ojeda MD, Ojeda Marrero V, Roque Castellano C, Cabrera Marrero JC, Mathías Gutierrez MP, Ceballos Santos D, et al. Perforaciones duodenales tras colangiopancreatografía retrógrada endoscópica. Cir Esp. 2015. This manuscript was presented as a communication at the XVIII Reunión Nacional de Cirugía, on 9–11 November, 2011, in Pamplona, Spain.