Morbid obesity is a serious health problem whose prevalence is increasing. Expensive co-morbidities are associated to these patients, as well as a reduction in the survival. Bariatric surgery resolves the co-morbidities (type 2 diabetes mellitus, 86.6%; cardiovascular risk, 79.0%; obstructive sleep apnea syndrome, 83.6%; hypertension, 61.7%), reduces the mortality rate (among 31%–40%), and increases the morbid obese patients survival over a 10-years period. It provides significant savings for the National Health System. The obese patients consume a 20% plus of health resources and 68% plus of drugs than general population. Bariatric surgery requires an initial investment (diagnosis-related group cost: 7468€), but it is recovered in a cost-effectiveness ratio of 2.5 years. Significant savings are obtained from the third year. To the direct economic benefits associated with reduced health expenditures an increase in tax collection should be added (sick leave and unemployment reduction are estimated in 18%, with a productivity increase of 57% for self-employed people). Bariatric surgery is one of the most cost-effective procedures in the healthcare system.
La obesidad mórbida es un problema grave de salud de prevalencia creciente que asocia costosas comorbilidades y reduce la supervivencia. La cirugía bariátrica (CB) además de resolver las comorbilidades (86,6% diabetes tipo 2; 79% riesgo cardiovascular; 83,6% apnea del sueño; 61,7% hipertensión arterial), reducir la mortalidad entre un 31–40% y aumentar la supervivencia de los obesos mórbidos 10 años, supone un importante ahorro al Sistema Nacional de Salud. Los obesos consumen un 20% más de recursos sanitarios y un 68% más de fármacos. La CB requiere una inversión inicial (grupos relacionados por diagnóstico: 7.468 €) que se recupera en un ratio coste-efectividad de 2,5 años y se consigue un ahorro significativo a partir del 3.er año. A la reducción directa de costes sanitarios se debería sumar el aumento en la recaudación de impuestos por reducción del 18% de paro y bajas y el aumento del 57% de la productividad de autónomos. La CB es una de las intervenciones más rentables del Sistema Nacional de Salud.
In a time of budget limitations and scarce resources, it is imperative to establish which health interventions are necessary and profitable in terms of the health of the population and financial costs. The association between obesity and multiple and costly diseases such as type 2 diabetes mellitus (DM2), hypertension (HTN), obstructive sleep apnoea (OSA), arthropathies, cancer, and others1,2 has made the care of obese patients problematic for the health care system. It is estimated that these patients consume 7% of the total healthcare cost in Spain, and after updating these costs to the year 2011, these patients account for approximately 2880 million Euros (€) per year.3 This cost could be decreased through health interventions promoting weight loss and a decrease in the prevalence of associated diseases.4,5
The prevalence of obesity has been progressively increasing in our country, with prevalence rates increasing from 9.1% to 15% (1993–2009), according to the Spanish National Health Survey (NHS). In fact, Spain is one of the countries with the greatest prevalence of obesity in the European Union.6–8 The prevalence of morbid obesity has increased by 200%, and 5%–8% of patients were found to have a body mass index (BMI) >35 and 1% with a BMI >40 in the ENRICA 2010 study.9,10 The most worrisome aspect is the increase in childhood obesity, which has risen from 5% to 19.1% during the last 10 years, with 26.1% of children classified as overweight.6 Without a doubt, prevention should be a priority of the health care system in order to slow this trend.11 However, for obesity cases where the BMI >40kg/m2, no prevention or treatment measure has achieved a long-term efficacy greater than 10%, with the exception of bariatric surgery (BS), which is associated with the remission of comorbidities and an increase in the life expectancy of operated obese individuals.12–14 The present study conducted a systematic review of the literature to evaluate the results of BS cost-benefits.
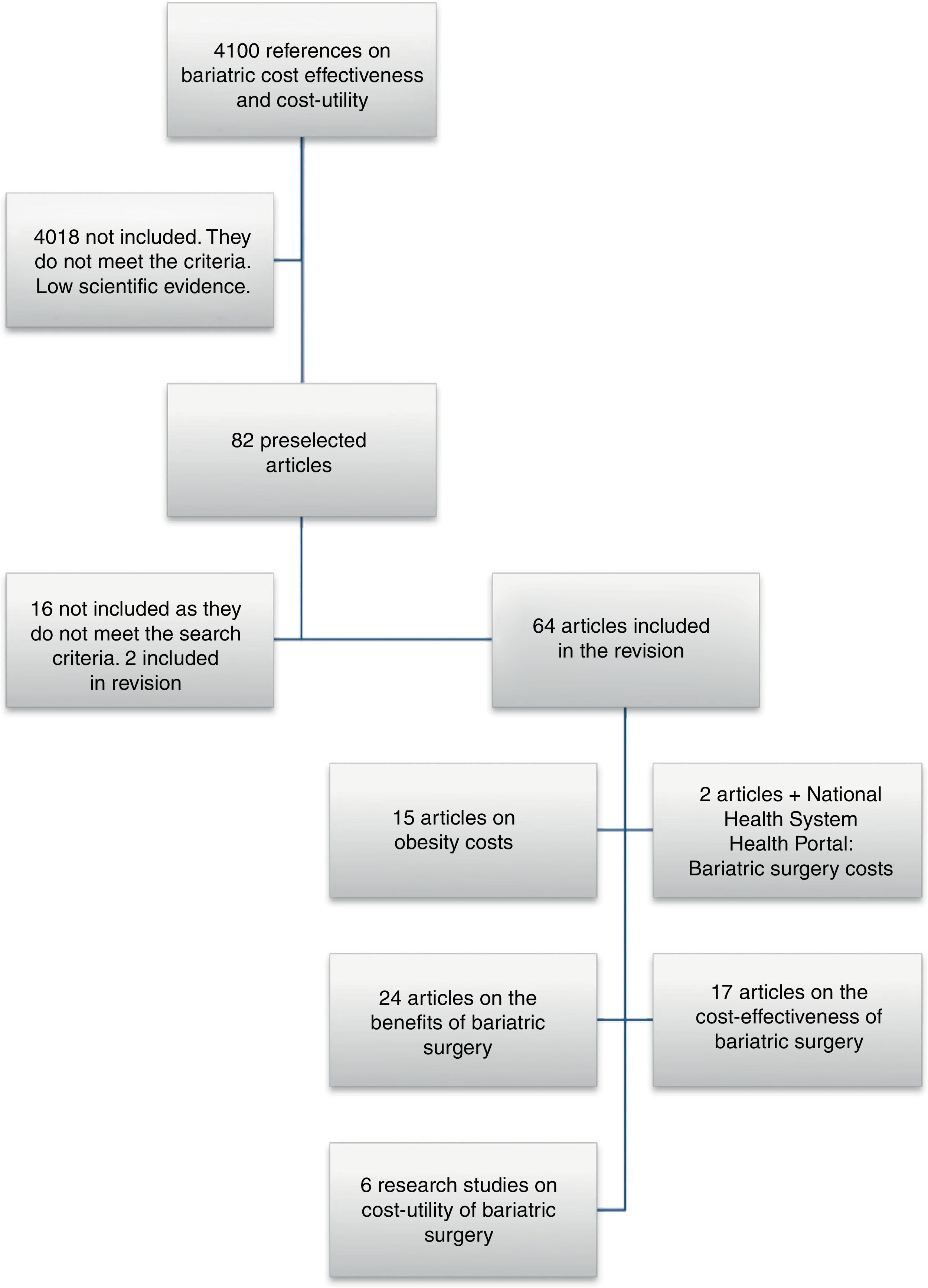
Materials and MethodsA meta-search was conducted in the following 9 databases using the terms “bariatric surgery cost-effectiveness” and “bariatric surgery cost-utility”: Pubmed, Scopus, Web of Science, Amazon Books, Google Scholar, Google Books, Pubget, Eric, and Spacenet. Articles in English and Spanish were selected that described concrete data related to the effectiveness of BS and provided cost-effectiveness, cost-benefit, or cost-utility ratios. Two experts then decided on the inclusion or exclusion of these articles for the present study. Articles that did not provide concrete numerical data with respect to the morbidity associated with obesity, mortality associated with obesity, obesity costs for the health care system, BS-associated morbidity, BS-associated mortality, and BS-associated costs were excluded.
The Spanish National Health System (SNHS) statistical portal was consulted to obtain data regarding BS in Spain (costs by Diagnosis Related Groups (DRGs), length of stay, comorbidities, and SNHS data).
ResultsMeta-searchA total of 4100 references were identified that included the words “cost” and “obesity”. Eighty-two articles or book chapters were selected that made reference to the effectiveness, cost-effectiveness, cost-benefit, or cost-utility of BS. In the final review, 66 publications were included that provided specific numerical data (Fig. 1). These studies were grouped by topic for posterior analysis, and the complete texts were reviewed. The publication dates ranged between 1999 and 2012.
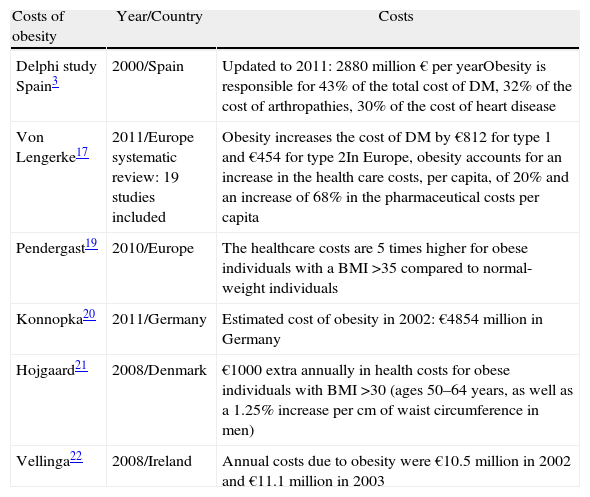
Costs Derived From ObesityThe evaluation of obesity management strategies requires prior analysis of the costs imposed on the healthcare system.15,16 A review published in 2011 provided data from 19 European studies that evaluated the impact of obesity on the cost of different diseases.17 For patients with diabetes, obesity increases the health costs by €812 per year for type 1 diabetes and by €454 for DM2; a 78% higher cost per capita has also been reported when obesity and diabetes are associated.17,18 In Spain, obesity is responsible for 43% of the total costs related to DM2, more than 32% of the costs related to arthropathies, and more than 30% of the costs related to cardiac diseases.23 In European countries, obesity contributes to a per capita increase of 20% in health care costs, and this increase in pharmaceutical expenses is 68% higher compared to normal weight patients.17,19 Numerous studies have reported the estimated annual cost of obesity for European countries. In 2002, in Germany, this cost was €4854 million, to which an estimated indirect cost of €5019 million was added.20 In Ireland, the annual hospital cost derived from obesity (without taking into account health care centres or drugs) was €11.1 million in 2003.22 In Spain, the costs associated with obesity account for 7% of the total health care cost; after updating these costs to 2011, this amount was approximately €2880 million/year23 (Table 1). In Denmark, the estimated total cost has not been published, but an extra yearly health cost of 1000$/person has been calculated for patients between 50 and 64 years of age with a BMI >30. Obesity is also responsible for increasing costs and worsening results following multiple surgical procedures, ranging from simple appendicitis or the placement of an orthopaedic prosthesis to organ transplant.24–27
Costs Associated With Obesity in the European Union.
| Costs of obesity | Year/Country | Costs |
| Delphi study Spain3 | 2000/Spain | Updated to 2011: 2880 million € per yearObesity is responsible for 43% of the total cost of DM, 32% of the cost of arthropathies, 30% of the cost of heart disease |
| Von Lengerke17 | 2011/Europe systematic review: 19 studies included | Obesity increases the cost of DM by €812 for type 1 and €454 for type 2In Europe, obesity accounts for an increase in the health care costs, per capita, of 20% and an increase of 68% in the pharmaceutical costs per capita |
| Pendergast19 | 2010/Europe | The healthcare costs are 5 times higher for obese individuals with a BMI >35 compared to normal-weight individuals |
| Konnopka20 | 2011/Germany | Estimated cost of obesity in 2002: €4854 million in Germany |
| Hojgaard21 | 2008/Denmark | €1000 extra annually in health costs for obese individuals with BMI >30 (ages 50–64 years, as well as a 1.25% increase per cm of waist circumference in men) |
| Vellinga22 | 2008/Ireland | Annual costs due to obesity were €10.5 million in 2002 and €11.1 million in 2003 |
No data related to the indirect costs of BS in Spain or other countries were found (with respect to the cost of sick leave, follow-up, examinations, etc.). Only data with respect to direct costs have been reported.
In the case of BS, the SNHS has defined a DRG that includes the surgical treatment of obesity with an average cost of €7468. According to data from the statistical portal of the SNHS, 2830 yearly cases were treated in hospitals of the public health care network between the years 2005 and 2010, with an average length of stay of 6.8 days. The estimated cost of this surgery in other countries is higher. For example, in the US, the average cost per BS procedure performed through Medicare between 2004 and 2008 was $19746.28 In Finland, the average cost per procedure in 2011 was approximately €14600.29
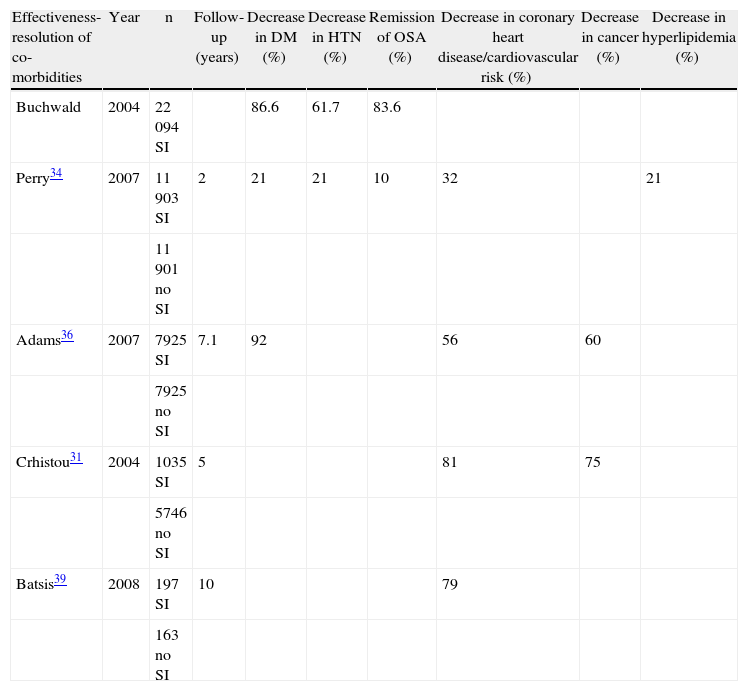
Benefits of Bariatric SurgeryAn increase in the survival of morbidly obese operated patients vs non-operated patients has been shown in studies with 5–10 years of follow-up data (Table 2). In particular, the mortality rate of patients who underwent BS was shown to decrease between 31% and 89% in studies that analysed between 2000 and 66100 patients who were followed for 5–10 years. BS has also been associated with a decrease in the incidence and mortality related to cardiovascular diseases and cancer.30–33 With respect to the evolution of several comorbidities, several studies and meta-analyses have been published with sample sizes between 3000 and 12000 surgically intervened (SI) patients; in these studies, remission of DM2 in 86.6% of patients,33 improvement or resolution of hyperlipidemia in 70% of patients, remission of HTN in 61.7% of patients, and remission of OSA in 83.6% of patients were reported.14 Likewise, a reduction between 32 and 56% of coronary diseases and a 60% reduction in the incidence of cancer have been observed.34–36 In addition, a 10-year increase in the life expectancy of operated morbidly obese patients vs non-operated patients has been estimated.30,37
Improvement in Comorbidities After BS.
| Effectiveness-resolution of co-morbidities | Year | n | Follow-up (years) | Decrease in DM (%) | Decrease in HTN (%) | Remission of OSA (%) | Decrease in coronary heart disease/cardiovascular risk (%) | Decrease in cancer (%) | Decrease in hyperlipidemia (%) |
| Buchwald | 2004 | 22094 SI | 86.6 | 61.7 | 83.6 | ||||
| Perry34 | 2007 | 11903 SI | 2 | 21 | 21 | 10 | 32 | 21 | |
| 11901 no SI | |||||||||
| Adams36 | 2007 | 7925 SI | 7.1 | 92 | 56 | 60 | |||
| 7925 no SI | |||||||||
| Crhistou31 | 2004 | 1035 SI | 5 | 81 | 75 | ||||
| 5746 no SI | |||||||||
| Batsis39 | 2008 | 197 SI | 10 | 79 | |||||
| 163 no SI |
To evaluate the direct tangible benefits related to BS, the following aspects were considered: (1) the savings in medications for the treatment of resolved comorbidities; (2) the savings in health benefits (including CPAP, glucometers, specialist consults, orthopaedic prostheses, etc.); and (3) the resolution of work-related disabilities.
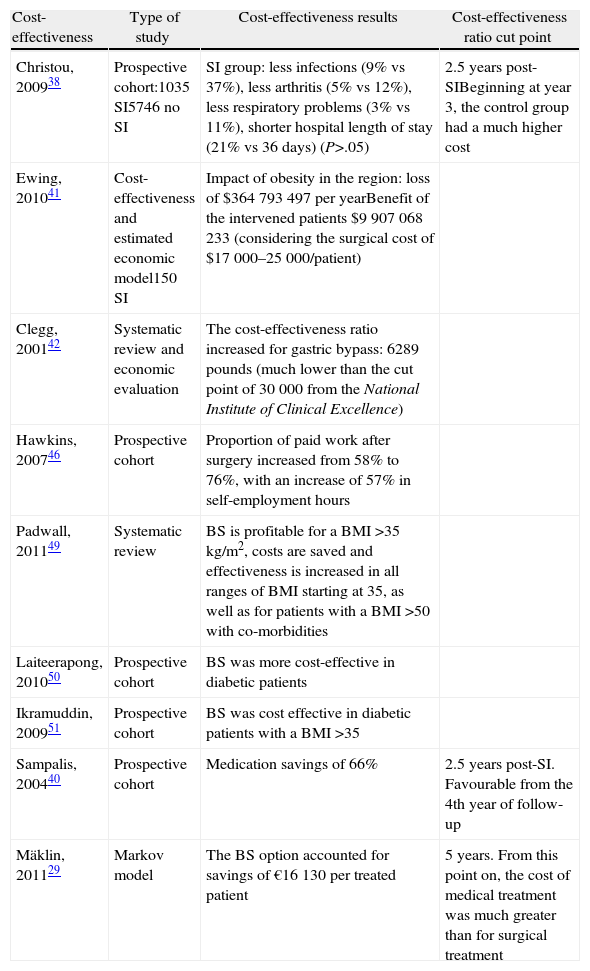
These benefits were highlighted in Canada following the study of Christou et al.,31,38 where operated patients demonstrated significantly lower rates of diagnosis of cancer (2% vs 8%), cardiac problems (5% vs 27%), infections (9% vs 37%), arthritis (5% vs 12%), and respiratory problems (3% vs 11%). Moreover, the health costs of the group that did not receive the SI far exceeded those of the operated patients after 3 years of follow-up. The cardiovascular risk (measured by the Framingham method) also decreased by 79% after BS, according to a study conducted by the Mayo Clinic, which compared 197 gastric bypass surgery patients with 163 non-operated morbidly obese patients.39 With respect to the savings from unnecessary medicines, the mean cost of treatments per patient decreased by 66%, where the cut-off point for the cost-effectiveness ratio was observed at 2.5 years after surgery; in addition, this favourable result for the group of operated patients remained at the fourth year of follow-up40 (Table 3).
Studies of BS Cost-effectiveness.
| Cost-effectiveness | Type of study | Cost-effectiveness results | Cost-effectiveness ratio cut point |
| Christou, 200938 | Prospective cohort:1035 SI5746 no SI | SI group: less infections (9% vs 37%), less arthritis (5% vs 12%), less respiratory problems (3% vs 11%), shorter hospital length of stay (21% vs 36 days) (P>.05) | 2.5 years post-SIBeginning at year 3, the control group had a much higher cost |
| Ewing, 201041 | Cost-effectiveness and estimated economic model150 SI | Impact of obesity in the region: loss of $364793497 per yearBenefit of the intervened patients $9907068233 (considering the surgical cost of $17000–25000/patient) | |
| Clegg, 200142 | Systematic review and economic evaluation | The cost-effectiveness ratio increased for gastric bypass: 6289 pounds (much lower than the cut point of 30000 from the National Institute of Clinical Excellence) | |
| Hawkins, 200746 | Prospective cohort | Proportion of paid work after surgery increased from 58% to 76%, with an increase of 57% in self-employment hours | |
| Padwall, 201149 | Systematic review | BS is profitable for a BMI >35kg/m2, costs are saved and effectiveness is increased in all ranges of BMI starting at 35, as well as for patients with a BMI >50 with co-morbidities | |
| Laiteerapong, 201050 | Prospective cohort | BS was more cost-effective in diabetic patients | |
| Ikramuddin, 200951 | Prospective cohort | BS was cost effective in diabetic patients with a BMI >35 | |
| Sampalis, 200440 | Prospective cohort | Medication savings of 66% | 2.5 years post-SI. Favourable from the 4th year of follow-up |
| Mäklin, 201129 | Markov model | The BS option accounted for savings of €16130 per treated patient | 5 years. From this point on, the cost of medical treatment was much greater than for surgical treatment |
The following are considered indirect, tangible benefits of BS: (1) re-entry into the job market and a decrease in unemployment rates; (2) reduction in sick leave; and (3) decrease of early deaths in the active population. The decreased rates of mortality among morbidly obese individuals after BS and the 10-year increase in life expectancy translate into an increase in working life, which is associated with income and tax payments.
A study conducted in the Plains region of southern Texas revealed the financial impact of BS in this area; in particular, this study looked at sick leave, job loss, and tax payments in a group of 150 morbidly obese individuals before and after BS. Comparing these results to the employment data of the regional database, morbidly obese individuals demonstrated a productivity equivalent of 87.8% that of a non-obese worker. The calculated impact of morbid obesity in this region involved a financial loss of US$ 364793497 per year, the loss of 1977 jobs, and an indirect tax loss of $13209196. In the case of the SI patients, considering a 3% yearly discount rate, the net benefit was US$ 9907068233 (considering the cost of BS to be between US$ 17000 and US$ 25000 per patient).41
Moreover, in the report of health technology produced by the National Institute of Clinical Excellence Guidelines for Bariatric Surgery, it was estimated that the incremental cost-effectiveness ratio for gastric bypass is 6289 pounds, which is well below the cut-off point of 30000 pounds considered by the National Institute of Clinical Excellence to be cost effective. This places BS among the most profitable interventions.42
Intangible BenefitsWith respect to the intangible benefits of BS, we considered the following: (1) the improvement in quality of life; (2) the improvement in well-being; (3) the increase in the possibilities of higher professional education; and (4) the possibility of higher job training.
The monetary value attributable to the indirect, tangible, and intangible benefits is complex. In a study conducted in the UK with a group of morbidly obese individuals who underwent gastric bypass, the rate of paid employment after BS increased from 58% to 76%. Moreover, self-employed workers increased their total work time from 1023 to 1611h, representing a 57% increase.46
Multiple studies have shown an improvement in the quality of life of patients after receiving BS.43–45 With respect to the cost-utility analysis used to quantify and evaluate the costs according to the unit of earned consequence of 2 or more health intervention alternatives, a health intervention tends to be considered as profitable in terms of cost-utility if it costs less than US$ 50000 per quality-adjusted life-year (QALY).47 In 2004, the American Society for Metabolic and Bariatric Surgery (ASMBS) published a cost-utility study comparing the results of diet and exercise vs gastric bypass in young women with a BMI >40. Gastric bypass was shown to be a more effective alternative with a cost-utility ratio of US$ 7126/QALY (in the branch of medical treatment, no gain was observed in years adjusted by quality of life).48 In Finland, a cost-utility study at 10 years estimated the medical treatment cost of morbid obesity to be around €50000 and that of BS to be around €33870, with an advantage in favour of BS of 7.63 QALY vs 7.05 QALY of medical treatment. Moreover, the cost of medical treatment is much higher than surgical treatment after 5 years of follow-up.29
Cost-benefit in Sub-groupsIs the cost-effectiveness of BS the same for all morbidly obese patients? A recent meta-analysis evaluated BS in relation to various sub-types of the population. For this, the sample included studies published since 2003 with a minimum of 1B degree of evidence. The obese population with a BMI ≥35kg/m2 was stratified according to the presence or absence of comorbidities (HTN, DM2, coronary heart disease, dyslipidemia, and cerebral disease), 3 categories of BMI, and the application of SI or no-SI. The mean age was 39.7 years, with no differences reported between groups. The global result of this study suggested that BS is profitable for patients with a BMI >35kg/m2, with an increasing benefit as the BMI value increases. Costs are also saved and the efficacy is improved for patients with severe obesity, with a BMI >50kg/m2, and with at least 1 comorbidity. In contrast, for individuals without co-morbidities and a BMI >50kg/m2, BS continues to cost $1904 per earned QALY. In any case, this procedure continues to be more profitable for such patients in comparison to those with lower BMIs and those without comorbidities (US$ 3872 for patients with a BMI between 35 and 40kg/m2 and US$ 3770 for a BMI between 40 and 50kg/m2). Moreover, the life expectancy for individuals without surgical treatment was reduced by approximately 6.5 years.49 Some studies have also pointed towards a greater cost-effectiveness of BS in the sub-group of patients with DM2.50–53
Treatment AccessibilityThe impact of a given health intervention on the health of the population depends, to a large extent, on accessibility, given that patients who cannot gain access to treatment cannot obtain the calculated benefit. In Canada, the US, and the UK, less than 1% of possible candidates receive BS, and the waitlists are very long (with an average of 5 years in Canada).54,55 In Spain, according to data regarding the prevalence of morbid obesity and the yearly interventions registered by the Spanish Ministry of Health and taking into account the annual survey conducted by the Spanish Society of Obesity Surgery (SECO, for its initials in Spanish), in the last 5 years, 5.24% of possible candidates have received SIs. Among the causes for this low accessibility, the following factors should be considered: deficits in the services offered by the SNHS due to the scarcity of specialised multidisciplinary teams; deficits in the health education of candidates who do not understand the consequences of their obesity and the available therapeutic options; deficits in the training of health care personnel regarding the therapeutic options available for patients with morbid obesity; and the socioeconomic discrimination that morbidly obese patients frequently experience. Indeed, society often blames morbidly obese individuals for their situation and makes access to treatment difficult, even at primary health care centres, which jeopardises the equality of the health care system.56
DiscussionObesity is a serious health problem for the Spanish population and a challenge for the funding of the public health system, as it entails an increase in the global yearly costs and an increase in the costs of other diseases including DM2, HTN, arthropathies, etc. Therefore, health interventions that can successfully reduce the percentage of obese individuals in the Spanish population, as well as the associated diseases, will lead to important savings in population health costs. The studies included in this review show that BS is a cost-effective health intervention in which the economical investment made is recovered within 2.5 years and savings to the health system are achieved within 3 years of surgery.
The greatest limitation of studies published to date regarding the cost-effectiveness of BS is the short follow-up duration, as the majority of studies have been limited to 5 years. This leads to bias in the long-term predictive models that could overestimate or underestimate the long-term impact of BS. However, the sensitivity analyses were consistent between studies, and the range of inter-study variability was small. Another bias we observed in the studies included in this review was that the majority of the models considered that the weight of the patients from both groups (medical and surgical treatment) would remain stable over time, and few studies considered the percentage of expected regained weight. However, when the cost-effectiveness ratio was analysed, it strongly favoured BS.48 Moreover, a majority of the models tended to only consider the direct costs and benefits of BS and did not include an analysis of the monetary value of the indirect benefits (increases in tax collection due to an increase in the percentage of paid work, reductions in sick leave, increases in productivity, etc.); in addition, indirect costs associated with BS were also not included (sick leave, examinations, regained weight, etc.).
The comparison between the costs of obesity and BS among different countries is complex, given that the funding from the different European or North American health systems is radically different, and there are also great differences in salaries, administrative expenses, prices of healthcare products, etc. Spain stands out due to the low calculated cost for many procedures, among which BS is included.
Another possible bias of the studies examined is the variability in the results between surgeons and centres based on the experience and annual volume of SIs. The inexperience or lack of training of the surgeon is frequently associated with an increase in post-operative morbidity and mortality, which may therefore reduce the benefit of surgery.48,57 This potential variability in results was not taken into account in the majority of the cost-effectiveness analyses included in the review, although these ratios appeared higher for the centres with the greatest experience and largest patient volume.58
Given the numerous benefits to health, quality of life, and finances resulting from BS, as well as the limited treatment accessibility of the affected population, significant attention should focus on rethinking health policies to favour strategies that can increase the number of BS procedures performed annually in our country, following the criteria for quality, safety, and efficiency that this type of surgery requires.59 To achieve these objectives, international scientific societies, including the International Federation for Obesity Surgery and the American Association of Bariatric Surgeons60–62 among others, recommend building multidisciplinary teams to address specific areas of obesity treatment. In addition, professionals should receive specific training for the treatment of morbid obesity, including general practitioners and general and gastrointestinal surgery specialists, endocrinologists, dieticians and nutritionists, anaesthesiologists, physiotherapists, psychiatrists, radiologists, etc. The SECO and the Obesity Chapter of the Spanish Association of Surgeons have made special efforts to establish appropriate competencies as well as theoretical and practical capacities for bariatric surgeons and have facilitated specific training in BS for surgeons who requested it.57 However, global health policies at the national level are also required to approach the problem of providing specific areas of training in our country. It is true that to increase the accessibility of BS for patients, it may be necessary to divert resources to the management of this area.63 However, studies have shown a recovery of the initial investment and a decrease in expenses over the course of 4–5 years, which may make BS a short-term profitable investment.31,40 Moreover, health expenses could be between 22 and 55% less with a reduction in the prevalence of obesity, according to a study conducted in the United States.16 Therefore, obesity control may be a very effective measure for the control of health costs, especially during times of financial crisis. Obesity prevention in the general population, particularly in children, and the treatment of obesity in its initial stages through diet and exercise programmes should be a priority for the Spanish health authorities, as in other countries such as the United States64,65 or Australia.66 In this context, BS should be included within the general strategic programme for the prevention and treatment of obesity, considering it as a highly profitable health intervention.
Conflict of InterestThe authors declare no conflict of interest.
Please cite this article as: Sánchez-Santos R, Sabench Pereferrer F, Estévez Fernandez S, del Castillo Dejardin D, Vilarrasa N, Frutos Bernal D, et al. ¿Es rentable operar a los obesos mórbidos en tiempos de crisis? Análisis coste-beneficio de la cirugía bariátrica. Cir Esp. 2013:91:476–484.