Gallstone ileus is an uncommon type of mechanical intestinal obstruction caused by an intraluminal gallstone, and preoperative diagnosis is difficult in the Emergency department. This study is a retrospective analysis of the clinical presentation of five patients with gallstone ileus treated between 2000 and 2012. Clinical features, diagnostic testing, and surgical treatment were analyzed. Five patients were included: two cases showed bowel obstruction; two patients presented a recurrent gallstone ileus with prior surgical intervention; and one patient presented acute peritonitis due to perforation of an ileal diverticula. In all cases CT confirmed the preoperative diagnosis. In our experience, gallstone ileus may present with clinical features other than intestinal obstruction. In suspicious cases CT may be useful to decrease diagnostic delay, which is associated with more complications.
El íleo biliar es una causa poco frecuente de obstrucción intestinal mecánica causada por el paso del cálculo a través de la luz intestinal de difícil diagnóstico preoperatorio en el Servicio de Urgencias. Presentamos un estudio retrospectivo de cinco casos tratados de íleo biliar entre 2000 y 2012. Se analizaron las características clínicas, las pruebas diagnósticas y el tratamiento quirúrgico realizado. Se incluyeron cinco pacientes, dos debutaron con una obstrucción intestinal típica, otros dos presentaron un ileo biliar recurrente previamente intervenido y el último presentó una peritonitis secundaria a la perforación de un divertículo ileal. En todos los casos el TAC permitió el diagnóstico preoperatorio. En nuestra experiencia el íleo biliar puede aparecer con clínica diferente a la obstrucción intestinal. En lo casos de sospecha un TAC puede ser útil para disminuir el retraso diagnóstico relacionado con mayor número de complicaciones.
Gallstone ileus is defined as a mechanical intestinal obstruction secondary to the presence of a gallstone in the intestinal lumen.1 The most common cause is the impaction of the calculus in the ileum after passing through a biliary-enteric fistula, which is usually cholecysto-duodenal.
It is a rare and potentially serious complication of cholelithiasis2 and represents between 1% and 3% of cases of mechanical obstruction of the small intestine. It is more common in patients over the age of 65, representing up to 25% of small bowel obstructions,3 and it is predominant in females, with a ratio of 3.5–6.0:1.4 Morbi-mortality is high, mainly due to its difficult and often delayed diagnosis. Although the classic presentation is that of intermittent incomplete obstructive symptoms caused by the movement of the calculus along the intestine, other rarer presentations have been described, that can delay diagnosis and deteriorate outcomes.
The aim of this study is to evaluate the clinical characteristics of patients diagnosed with gallstone ileus that could aid in proper preoperative diagnosis in the Emergency Department. Despite the limited number of series published in Spain (this is the second), it has been shown that when the diagnosis is made intraoperatively, the rate of immediate complications is higher than when the diagnosis is done preoperatively.5
Material and MethodsWe present a retrospective review of patients diagnosed with gallstone ileus at our center over a period of time between 2001 and 2010. In the five diagnosed during this period, we analyzed age, sex, associated comorbidities (hypertension, diabetes mellitus, heart disease, chronic obstructive pulmonary disease), the index of the American Society of Anesthesiologists (ASA index), symptoms at onset, delay in diagnosis and, therefore, in surgical treatment, physical examination, diagnostic testing and analytical data of interest. The small number of patients only allowed us to carry out a descriptive statistical analysis. Statistical calculations were performed with SPSS© for Windows, version 15.0.
ResultsOut of a total of 456 small intestine obstructions, 5 cases of gallstone ileus were diagnosed, which is 1.09% of all intestinal obstructions treated at our Emergency Department. They were one male and four females aged between 67 and 86, with a mean age of 76±7.8 years. All patients except one had been previously diagnosed with cholelithiasis (80%).
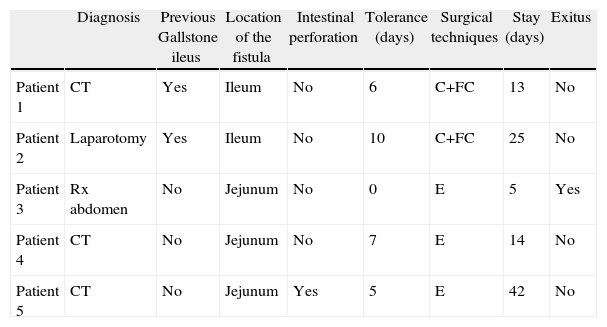
The most common associated diseases (comorbidities) of the affected patients were hypertension (60%), heart disease (60%) and diabetes (25%). When we classified these patients with ASA criteria, four patients (80%) had an ASA 3 risk and the fifth patient had an ASA 2 risk. These data are summarized in Table 1.
Clinical Data.
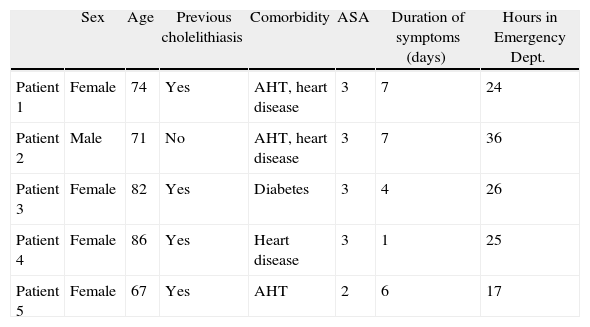
| Diagnosis | Previous Gallstone ileus | Location of the fistula | Intestinal perforation | Tolerance (days) | Surgical techniques | Stay (days) | Exitus | |
| Patient 1 | CT | Yes | Ileum | No | 6 | C+FC | 13 | No |
| Patient 2 | Laparotomy | Yes | Ileum | No | 10 | C+FC | 25 | No |
| Patient 3 | Rx abdomen | No | Jejunum | No | 0 | E | 5 | Yes |
| Patient 4 | CT | No | Jejunum | No | 7 | E | 14 | No |
| Patient 5 | CT | No | Jejunum | Yes | 5 | E | 42 | No |
C+FC: cholecystectomy plus biliary-enteric fistula closure; E: enterotomy; Rx. abdomen: abdominal radiography; CT: computed tomography.
The clinical symptoms when the patients came to the ER were different amongst the 5. Three presented with symptoms of pain and abdominal distension along with vomiting, indicative of bowel obstruction. The fourth patient reported a vague history of recurrent abdominal pain and intermittent abdominal distention and, lastly, the fifth patient showed symptoms of intense abdominal pain, peritoneal irritation and silent abdomen with an onset of just a few hours after having experienced vague and intermittent abdominal pain some days prior.
On physical examination, the most common findings were mucocutaneous dehydration and abdominal distension, which were present in all cases.
The average time transpired from the onset of symptoms until arrival at the Emergency Department and indication for surgery was 5±2.5 days (Table 1). On the other hand, the time elapsed from the patients’ arrival to the ER and the start of laparotomy was 19.6±6.6h.
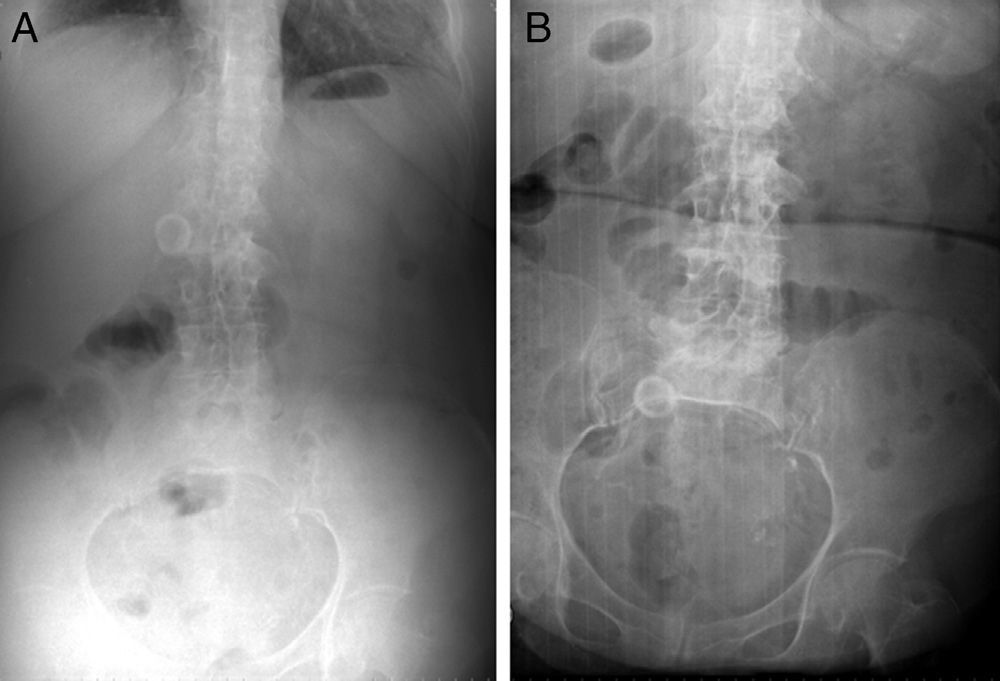
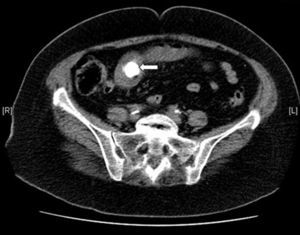
All patients underwent abdominal radiography. In only one patient did we observe the Rigler triad (dilated small bowel loops, ectopic biliary lithiasis and pneumobilia). In the remainder, important dilatation was observed in the bowel loops with air-fluid levels (Fig. 1A and B). Three of these four cases underwent abdominal computed tomography (CT) (patients 1, 4 and 5). In all the cases, CT scans showed pneumobilia and a calculus that was causing the intestinal obstruction (Fig. 2) and confirmed the diagnosis. In all three cases, coronal CT reconstruction demonstrated a cholecysto-duodenal fistula (Fig. 3). In patient number 5, a large pneumoperitoneum was also observed. In the remaining patients, no radiological abnormalities were evident and they were operated on with no clear preoperative cause due to acute abdominal symptoms. Hence, preoperative diagnosis was possible in 80% of cases (Table 2).
Epidemiological and Clinical Data.
| Sex | Age | Previous cholelithiasis | Comorbidity | ASA | Duration of symptoms (days) | Hours in Emergency Dept. | |
| Patient 1 | Female | 74 | Yes | AHT, heart disease | 3 | 7 | 24 |
| Patient 2 | Male | 71 | No | AHT, heart disease | 3 | 7 | 36 |
| Patient 3 | Female | 82 | Yes | Diabetes | 3 | 4 | 26 |
| Patient 4 | Female | 86 | Yes | Heart disease | 3 | 1 | 25 |
| Patient 5 | Female | 67 | Yes | AHT | 2 | 6 | 17 |
ASA: American Society Anesthesiology; AHT: arterial hypertension.
Two patients had previous histories of gallstone ileus and had undergone enterolithotomy and removal of the calculus (Table 2). The recurrence of gallstone ileus occurred within 3 months of the initial symptoms in one patient and within 6 months in the other. In one case (patient #4), laparotomy showed biliary peritonitis secondary to jejunal diverticular perforation existing in a section of dilated small intestine prior to impaction of the calculus (Table 2).
The most common biochemical abnormalities were hypokalemia (60% of cases), hyponatremia (40%) and metabolic alkalosis (40%).
The surgical technique used was cholecystectomy with closure of the biliary-enteric fistula in the two cases of recurrent gallstone ileus (40%), opting for enterotomy and stone removal in the three remaining cases (60%). The days required for postoperative tolerance to oral intake was 5.6±3.6 and mean hospital stay was 19.8±14.3 days. Postoperative mortality was 20% (one case), secondary to the development of acute pulmonary edema with acute renal failure. As there was just one single case, we cannot establish variables that could predict a poor prognosis.
DiscussionGallstone ileus is a rare complication of cholelithiasis in senior patients. In our study, it was seen in 1.09%, which is within the range of other series.3 This low incidence means that in our country there has only been one published series of 40 cases; the rest of the publications are case-control studies. Therefore, the retrospective study shown here is the second series published in Spain and, despite the limitations resulting from its size, it shows a high incidence of atypical presentations, which makes it undeniably interesting to emergency surgeons. In our group, the most frequently associated diseases were heart disease and hypertension, which appeared in 40% of patients. Due to these characteristics, mortality in patients with gallstone ileus ranges between 7.1% and 18%.6,7 In our series of gallstone ileus, mortality was 20%. This single case cannot establish a predictive relationship between clinical or therapeutic characteristics and death, although it does illustrate the high mortality of these patients.
The results of sex and age are similar to those published by other authors.8,9 The youngest of our patients was 67 years old. The earliest published case of gallstone ileus was seen in a 13-year-old patient.10 Most patients were previously diagnosed with cholelithiasis. In all cases, the diagnosis had been made by their Primary Care physician in the context of an abdominal pain study. In no case had the patients previously gone to the emergency room for cholelithiasis complications.
All patients reported a history of vague symptoms of abdominal pain during the days (mean 5.5 days) prior to arrival to the emergency room, probably due to the movement of the calculus along the intestine until the obstruction was complete. Once in the Emergency Department, the time elapsed from admittance until laparotomy was 19.6h, which demonstrates the difficult diagnosis given the symptoms, although it is possible that this time may include a delay in the start of laparotomy caused by the availability of an emergency operating room, which is an aspect that could not be assessed.
The radiographic diagnostic criteria for gallstone ileus described in 1941 that are still currently valid are: signs of complete/partial small bowel obstruction, pneumobilia, visualization of the gallstone (if calcified), changes in the stone's position and two adjacent air-fluid levels, located in the right upper quadrant. At least two of the first three radiographic signs described appear in 50% of the cases; pneumobilia, for instance, is evidenced in 30%–60% of cases. However, with these criteria the preoperative diagnosis is only made in 31%–48% of patients.7,11 The results of our series show that abdominal radiography is not useful for the diagnosis of gallstone ileus as it was only diagnostic in one case. However, in the three patients who underwent CT scan, the test was diagnostic in 100% of the cases. Moreover, coronal CT reconstruction showed in 100% of cases the presence of a cholecysto-duodenal fistula, which was the origin of the gallstone ileus.12 The presence of the pneumoperitoneum in patient 5 was an added complication to obstruction. While recognizing the limited size of this series, what we draw from this experience is that it would be prudent to recommend a CT scan in cases of small bowel obstructions of uncertain causes in order to clarify the origin.
Recurrent gallstone ileus occurs in 5% of cases,13 and 57% of them occur in the first 6 months after the first intervention, which is usually enterotomy and calculus extraction without cholecystectomy.13 In our series, recurrence occurred in 40% of cases, one during the first 3 months and another within the first 6 months after the first intervention, which had been enterotomy with stone extraction in both cases. This high incidence of recurrence in our series means that, in a patient with a bowel obstruction and a history of prior gallstone ileus, gallstone ileus should be considered.
Jejunal perforation is a rare complication of gallstone ileus, and only 10 cases have been described in the literature. The perforation can occur at or prior to the point of impaction of the gallstone. It typically appears on the antimesenteric border and is secondary to the hyper pressure that causes the obstruction with necrosis and perforation of the jejunal wall.14 Recently, Browning et al. described for the first time in the literature a perforation in the mesenteric border, produced by the perforation of a preexisting jejunal diverticulum.14 In our case number 5, the mesenteric location of the perforation, the presence of food remains and the presence of two jejunal diverticula in the proximity of the perforation support the fact that intestinal obstruction secondary to gallstone ileus would cause intraluminal hyper pressure in the proximal jejunum and, consequently the preexisting jejunal diverticular perforation. This would be the second case described in the literature.15
Treatment of gallstone ileus is primarily surgical, entailing the extraction of the calculus by enterotomy. After removing the calculus that is causing the obstruction, there is controversy about the surgical technique to subsequently perform. A single-phase technique, indicated in patients with low surgical risk, would also include cholecystectomy and biliary-enteric fistula repair (definitive repair).7,16,17 The two-phase technique would be conducted by first treating the obstruction by enterotomy, indicated for patients with high surgical risk,18,19 and subsequently evaluating the need for a bile duct procedure.
While single-phase surgical treatment presents greater mortality (16.9%) than the two-phase treatment (11.7%),13 the latter is not without complications, including recurrent gallstone ileus. In a review of 1001 cases,13 Reisner and Cohen showed a recurrence of gallstone ileus of 5% (57% of recurrences were within 6 months after the first surgery). The authors demonstrated that, in most cases (80%–90%), the gallstones were passed spontaneously and without clinical repercussions.13 Therefore, they concluded that enterotomy and extraction alone is the procedure of choice for patients with significant comorbidity. This view is supported by other authors, such as Muthukumarasamy20 and Rodriguez-Sanjuan.7 In our series, the two patients with recurrence were treated with single-phase surgery with complete resolution of the fistula. In the remainder, we chose to perform enterotomy and extraction of the calculus alone. So far, after a mean follow up of 35 months, there have been no complications.
ConclusionGallstone ileus is an important although uncommon cause of mechanical obstruction. It is essential for surgeons on emergency call to understand this entity in order to make the diagnosis as early as possible. Although it typically presents intermittent obstruction symptoms caused by the migration of a gallstone along the intestine, patients often present vague symptoms several days prior to emergency care, and there may be rarer presentations. For example, the presence of peritonitis in the abdomen due to intestinal perforation secondary to intestinal hyper pressure, which causes the obstruction and leads to primary perforation, or a preexisting diverticulum, as occurred in our patient number 5. It should also be noted that a history of a previous episode of gallstone ileus does not preclude a new occurrence. While in the literature the recurrence rate is very low (about 5%), in our series it was 40% (2 patients), so we should not rule out the diagnosis of gallstone ileus in patients with previous history. In uncertain cases of intestinal obstruction, CT can be very useful for diagnosis, since it not only diagnoses gallstone ileus, but it is also able to find the biliary-enteric fistula that causes it. The ability to preoperatively diagnose the symptoms has a direct influence on reducing complications, so its treatment in the Emergency Department is extremely important.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Martín-Pérez J, Delgado-Plasencia L, Bravo-Gutiérrez A, Burillo-Putze G, Martínez-Riera A, Alarcó-Hernández A, et al. El íleo biliar como causa de abdomen agudo. Importancia del diagnóstico precoz para el tratamiento quirúrgico. Cir Esp. 2013;91:485–489.