Rectal duplication cyst (RDC) is a rare anomaly of intestinal tract representing 3%–8% of alimentary tract duplications1. Neoplasm arising into RDC is very rare situation being difficult to suspect.
We report a case of adenocarcinoma occurring in a true RDC that was initially confused as a fistulized pilonidal disease and successfully treated with radical surgery and adjuvant radiation therapy.
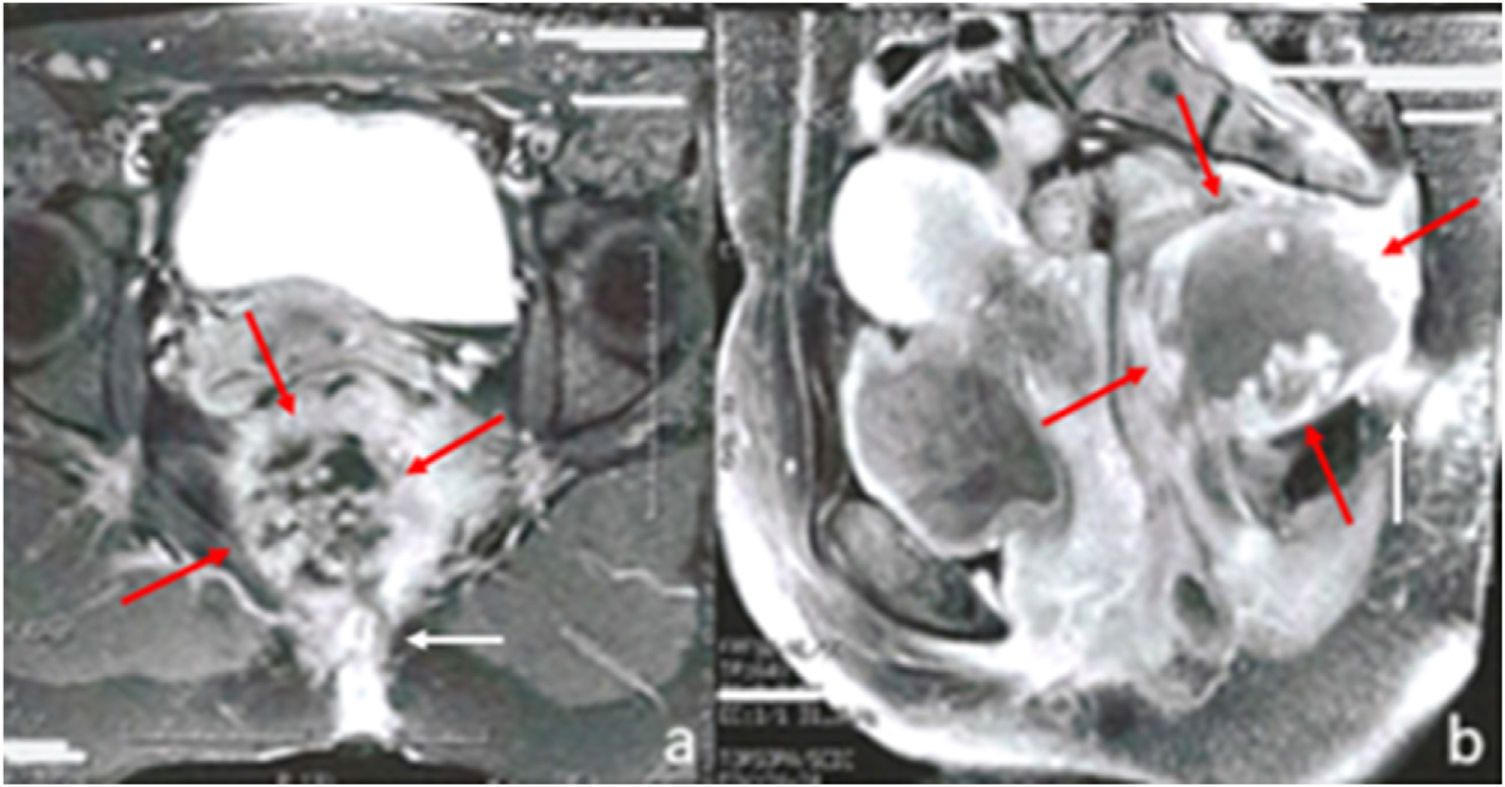
A 42-year-old woman, was referred because of persistence of purulent drainage from sacro-coccygeal wound, five months later excisional surgery of a pilonidal cyst; no malignant cells were found at histological study. Recto-sigmoidoscopy showed a partially ulcerated lesion at 8−9 cm from the anal verge, draining purulent liquid: biopsy described inflammatory tissue without malignancy. Pelvic magnetic resonance imaging (MRI) described a 64 × 35 mm solid-cystic mass in retrorectal space with fistulous tract opened in sacro-coccygeal wound without rectal wall involvement (Fig. 1a and b).
With diagnosis of retro-rectal cystic hamartoma fistulized to intergluteal cleft, the patient underwent surgery, performing a kraske posterior approach. In-bloc resection was performed including affected skin, fistula tract, coccys, part of left levator ani muscle, tumor and part of posterior wall of de low rectum, firmly attached to the lesion. Rectal defect was sutured and protected by loop ileostomy. No complication occurred in early and late postoperative course.
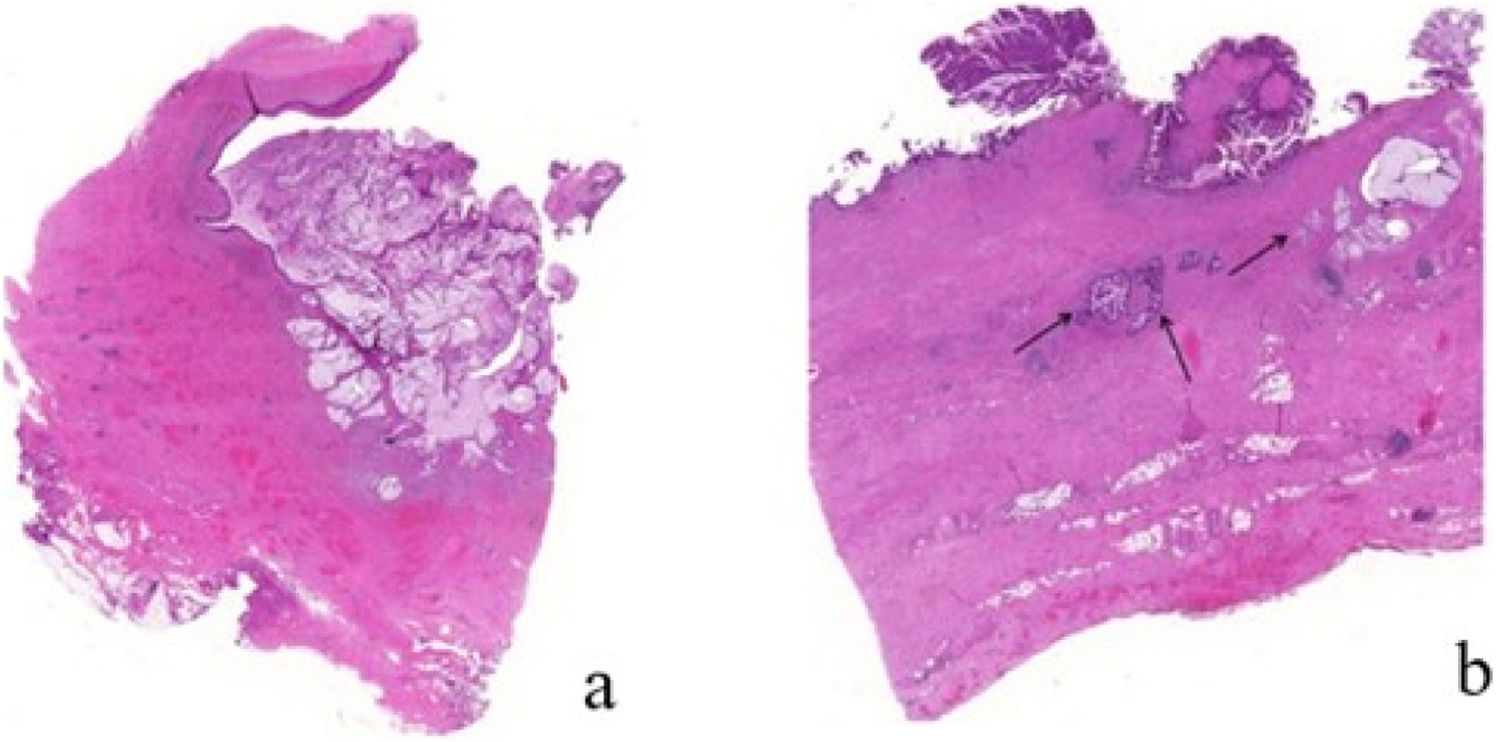
Histological diagnosis was “invasive adenocarcinoma of intestinal type with more than 50% of mucin and focus of squamous and transitional epithelium over smooth muscle within a rectal duplication cyst” (Fig. 2a and b) with resection margins free from neoplasm.
(a) Haematoxylin–Eosin 40×, showing neoplastic degeneration of the cyst wall with intestinal epithelium. Note pools of extracellular mucin; (b) atypical glands with abundant extracellular mucin; low power view of the cyst wall with a smooth-muscle coat in two layers. The inner lining mucosa shows intestinal type epithelium with high-grade dysplasia and invasive adenocarcinoma (arrows).
Metastatic disease was ruled out after surgery and the patient received adjuvant pelvic radiotherapy. After nine years of follow-up, the patient remains disease-free; unfortunately, at the eighth postoperative year, she developed a radio-induced sarcoma of the left iliac bone of the pelvis and needed surgery of internal left hemipelvectomy.
It is widely accepted that RDC occurs during embryological development, due to abnormal splitting of the notochord, consisting of a persistent connection between endoderm and dorsal ectoderm2. It is most frequent in female patient, often associated with other congenital defects, mostly genitourinary and vertebral anomalies. Neoplasm arising within RDC is very uncommon; few cases have been reported in literature and the real incidence is not well-known, estimated around 12% in adults with RDC3,4. Also, to our knowledge, only one case have been previously described with presentation similar to pilonidal disease4.
Diagnosis of rectal duplication is based on the Ladd’s criteria: contiguity with the intestinal tract with a smooth muscle coat and a mucosal lining of intestinal cells5. In our case, histologic study described a malignant disease within a true case of rectal duplication, since all Ladd’s criteria were present.
RDC is frequently asymptomatic; potential symptoms are anal bleeding, tenesmus and anal suppuration: in 20%–45% of cases, a fistula tract is present due to ulceration or infection4,6. In our patient, the malignant RDC fistulized to the sacrococcygeal area and was confused with a pilonidal sinus.
Recto-sigmoidoscopy should be performed to rule out invasion of the rectal wall. MRI is the diagnostic method of choice, useful to studying relationship between tumor and surrounding structures in order to plan the most appropriate operative approach7.
Preoperative biopsy is a controversial issue: the access to retrorectal space is limited due to the sacrum, with risk of bleeding, sepsis, seeding of malignant cells, nerve injury and possibility of inconclusive histology6. When the tumour is resectable, surgical resection should be performed without histological confirmation, taking care to remove in-bloc suspicious tissue and invaded anatomical structures. Only for inoperable patients, unresectable lesion or metastatic disease, malignancy should be confirmed to indicate oncospecific chemo-radiotherapy.
Different surgical approaches have been proposed to achieve curative excision of presacral tumours, depending on size and location with respect to the rectum, sacrum bone and adjacent structures7,8. In our patient, the lesion was situated below the third sacral vertebra so we performed a posterior para-sacrococcygeal approach (Kraske procedure).
There are poor data concerning malignant recurrence. Before the present case, just 4 of 13 papers on this topic provided information about oncological outcome3,4,9,10 but only Parvaiz et al. report a long term follow-up results without recurrence4: similarly to that, our patient was successfully treated with surgery, with no postoperative complications and no evidence of disease relapse (local or metastatic) nine years after surgery. Nevertheless, two aspects of our case should be emphasised. First, RDC presented a clear communication with rectal lumen and the neoplasm invaded the posterior wall of the rectum: these findings are important since morbidity could have been higher and disease-free survival could have been worse than we observed; second, our patient received postoperative adjuvant radiotherapy, so we cannot know how it was relevant in local recurrence control. Actually, there are no data that supports the use of postoperative chemo-radiotherapy in the treatment of adenocarcinoma arising in duplication cyst of the rectum. Due to lack of experience in oncological multidisciplinary treatment of this type of rectal neoplasm, together with the fact that the tumour fistulised towards surrounding structures, Colorectal Cancer Committee of our institution achieved the consensus to give postoperative adjuvant radiation, according to the current indication for common rectal cancer.
Conflict of interestThe authors declare that they have no conflict of interest.
We wish to thank our patient for the consent to report her clinical experience.