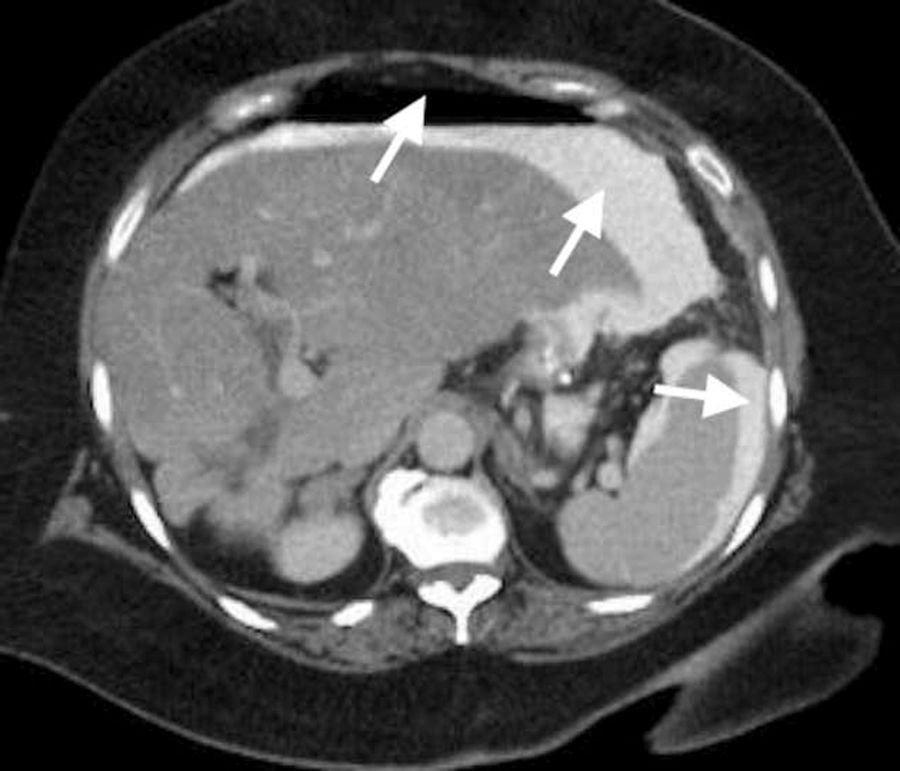
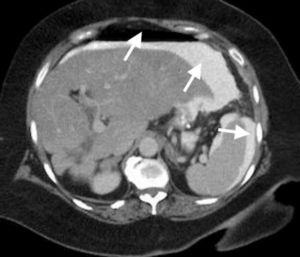
Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) was introduced by Sanchez-Pernaute et al. in 2007 for super-obese patients (BMI>50kg/m2).1 This procedure reduces complications and surgical time, but if an anastomotic leak (AL) occurs, it can be difficult to diagnose and treatment ranges from conservative measures to re-operation.2,3 There are very few published cases of AL after SADI-S.2,4 We present a technical option of how to surgically resolve an AL after this procedure. The patient is a 60-year-old woman with a BMI of 55kg/m2, personal history of type 2 diabetes and obstructive sleep apnea syndrome. Four days earlier, she had undergone a laparoscopic SADI-S procedure at another hospital, with no complications during the hospital stay. Upon arrival at our emergency room, she presented hypertension, tachypnea, malaise and progressive abdominal pain. She reported no fever, nausea or vomiting. Laboratory tests were normal, except for C-reactive protein: 90mg/L (reference values: 0–8.0mg/L). Computed tomography (CT) scan with oral contrast demonstrated pneumoperitoneum and peri-hepatic and peri-splenic free fluid (Fig. 1). We decided to perform urgent laparoscopy, finding diffuse peritonitis. The AL site was identified on the posterior side of the duodeno-ileal anastomosis. The defect was closed with absorbable sutures; the abdominal cavity was washed abundantly, and aspiration drain tubes were put in place.
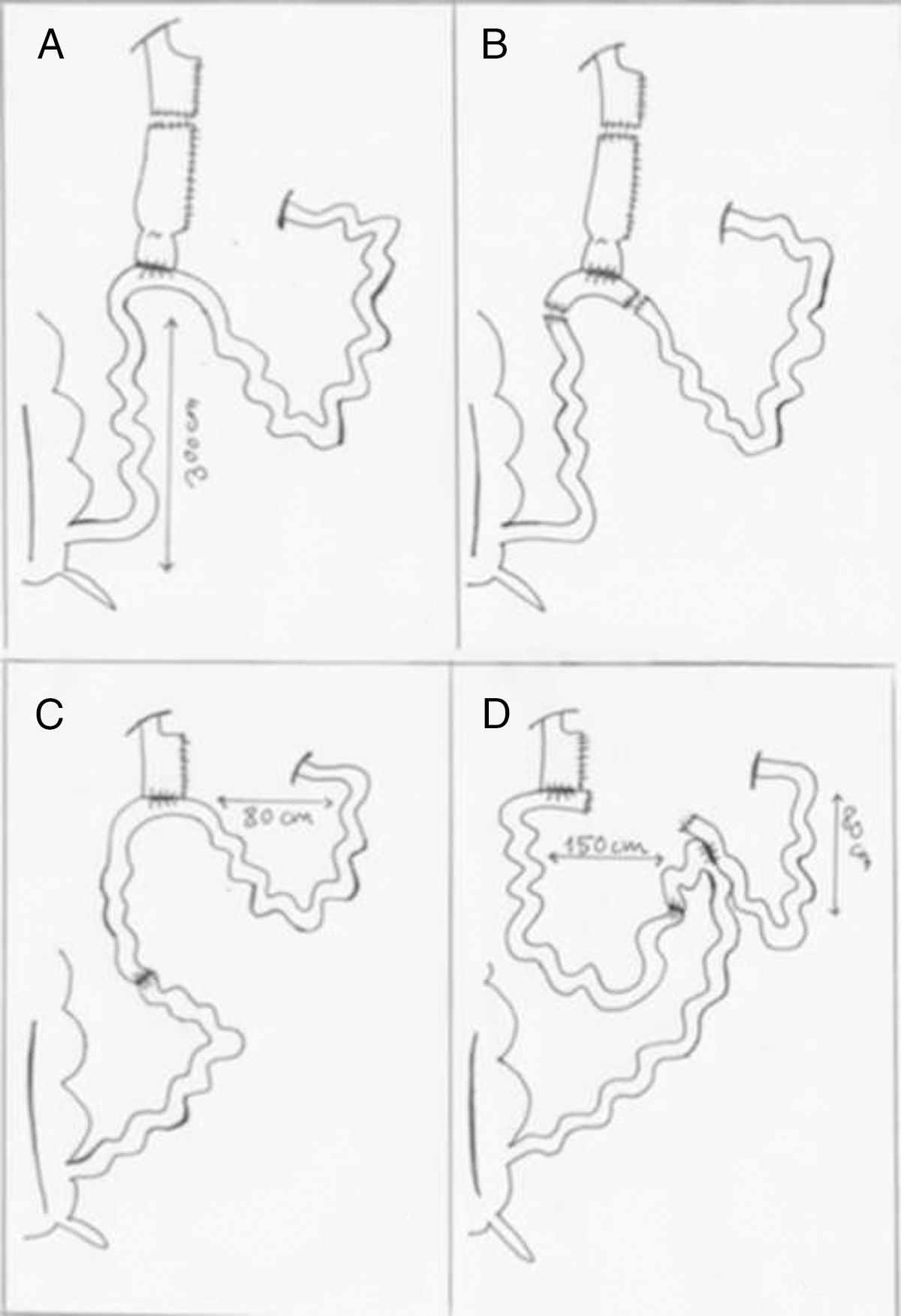
24h later, the patient presented clinical deterioration and bilious discharge through the abdominal drain tube, so emergency laparotomy was performed. We observed that the duodenal-ileal anastomosis was again dehiscent. Instead of another repair, drain placement and the impossibility of performing a feeding jejunostomy without modifying the configuration of the loops, we decided to create a Roux-en-Y gastric bypass (RYGB). A 60cm3 gastric pouch was created by dividing the sleeve gastrectomy with linear staplers. The gastric remnant was resected in an inverted Y with the duodeno-ileal anastomosis, including the leak point, in the piece. The ileum was then reconstructed with a side-to-side mechanical anastomosis, and a RYGB was performed with linear staplers (Fig. 2). Finally, two 19-French suction drains were inserted. Total parenteral nutrition was started on day 1 of the postoperative period and intravenous piperacillin–tazobactam was administered for 10 days. On the 8th postoperative day, the anastomoses were tested with oral methylene blue, and the patient began to drink liquids. On the 10th postoperative day, a radiological study was done with Gastrografin®, which confirmed that there was no leakage. On the 17th postoperative day, the patient presented a peri-splenic abscess requiring percutaneous drainage under radiological control. The hospital stay was 26 days. The SADI-S is a technique that reduces the number of intestinal anastomoses, which offers a series of advantages: lower probability of postoperative AL or stenosis of the anastomosis, favorable rate of weight loss results and resolution of comorbidities, with an incidence of postoperative complications and nutritional deficiencies comparable to those obtained with biliopancreatic diversion or the duodenal switch. The overall rate of complications in SADI-S is 4.8%.2,5
(A) Creation of a 60cm3 gastric pouch with a linear stapler; (B) inverted Y resection of the gastric remnant and ileum, including the anastomosis with the leak; (C) creation of mechanical ileo-ileal and gastrojejunal anastomoses, with a biliopancreatic loop measuring 80cm in length; (D) creation of a 150cm intestinal loop and finally division of the communication between the biliopancreatic loop with the gastrojejunal anastomosis.
Sánchez-Pernaute et al. achieved a low rate of AL and re-operation in their first 100 cases, observing only one AL treated conservatively with success. Other studies, such as Nelson et al., obtained similar results, with a single AL in the duodeno-ileal anastomosis in a total of 69 patients, treated successfully with conversion to a mini gastric bypass.6,7 Bariatric surgery has been proven a very effective method to treat morbid obesity, but AL are very dangerous complications, associated with prolonged hospital stays and severe morbidity and mortality. The incidence of AL published in bariatric surgery ranges from 0% to 5.6% with a mean of 2.4%.8 Early diagnosis and proper management are the keys to therapeutic success.3 The etiology of AL is multifactorial, and “acute” leaks are those appearing within the first 7 postoperative days. These are usually secondary to technical surgical problems or ischemic mechanisms and usually require early re-operation.3 The surgical treatment of AL is most widely accepted in cases of severe sepsis and no response to rigorous resuscitative measures. This approach is essential in cases of high-discharge jejunal–jejunal or jejuno-ileal AL, as it leads to rapid deterioration.9 The laparoscopic approach is the best option.4
In our case, given the viability of the tissue because it was an acute yet small AL, our initial decision was to repair the AL, which did not succeed. In such cases, drainage and washing is the best treatment option, and primary repair should be deferred. In the second intervention, the option of reconstructing the anastomosis and converting to duodenal switch would have been a valid alternative, but with the lack of experience in this technique, we decided to convert to RYGB. We have only found one series in which an AL required conversion of the SADI-S to a mini gastric bypass.7 There is no algorithm for managing AL associated with the SADI-S technique, but we believe that urgent conversion to RYGB can be a safe option that provides a definitive solution to the leak. Informed consent was obtained from all the individual participants included in the study.
Please cite this article as: Morante Castaño J, Carlin Gatica JH, Veguillas Redondo P, de la Plaza Llamas R, Ramia Angel JM. Derivación gástrica en Y de Roux como procedimiento de urgencia para resolver la fuga en un SADI-S. Cir Esp. 2018;96:663–664.