Papillary thyroid carcinoma (PTC) is the most common malignancy of the thyroid gland. Currently, in addition to the classic PTC variant, 14 other histopathological variants can be distinguished.1
The Warthin-like variant of papillary thyroid carcinoma (PTC-WL) is rare (1.9%),2 as only 164 cases have been described,3 and there are no specific recommendations regarding its prognosis and treatment.
We present a case of the PTC-WL variant and comment on the most relevant aspects of this type of tumor given its rarity.
A 59-year-old woman with no medical history consulted for a nodule in the left thyroid lobe that was well defined, non-adherent, measured 2cm, with no palpable lymphadenopathies. Analytically, the patient was euthyroid with elevated anti-TPO antibodies (1500IU/mL).
Ultrasound revealed a solid, hypoechoic nodule measuring 17mm×21mm×16mm with no halo, scarce intranodular vascularization and a poorly defined surface (TIRADS 4C). FNA was performed on 2 occasions, reported as Bethesda II.
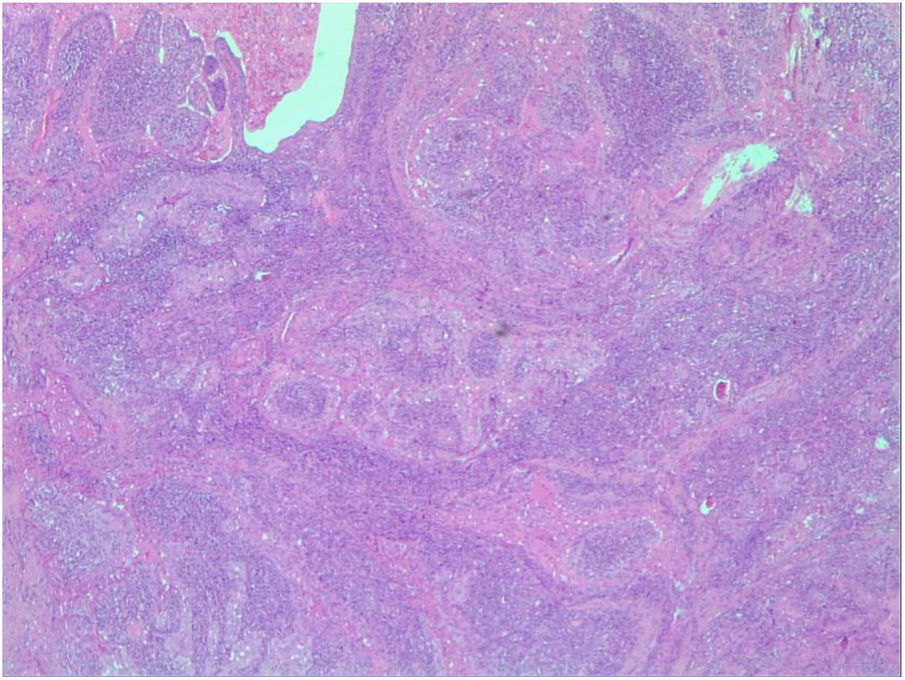
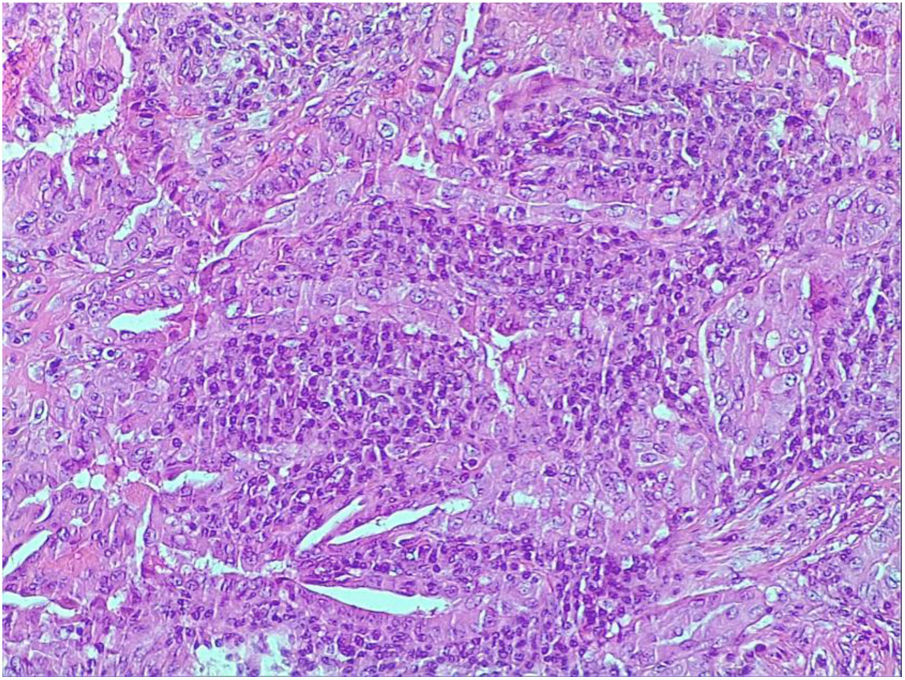
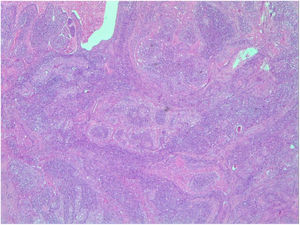
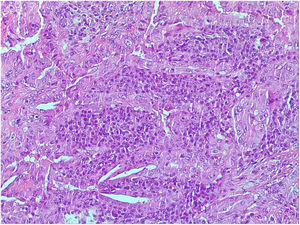
Left hemithyroidectomy was indicated. The pathology study reported a PTC-WL variant measuring 2cm, no capsular infiltration, mutated BRAF V600E biomarker and associated thyroiditis (Figs. 1 and 2).
The patient was reoperated with right hemithyroidectomy and prophylactic left lymph node dissection, with definitive histology of thyroiditis and no lymph node involvement.
Radioiodine (100mCi) was administered, and after 18 months of follow-up the patient is disease-free with thyroglobulin 0.1ng/mL and anti-thyroglobulin antibodies 0.1IU/mL.
The PTC-WL variant mainly affects women (W:M=8:1) in the fifth decade of life.3 Its name is due to the histological similarity with salivary gland tumors4 and its behavior is similar to the classic PTC variant,1 which is currently considered different from the oncocytic variant due to histological and prognostic differences.
The size is variable (0.5–6.0cm), presentation is usually unifocal (88%) and lymph node involvement is seen in up to 45% of cases, similar to the classic variant.2,3 On ultrasound, they are usually seen as solid-cystic nodules.5 Diagnosis by FNA biopsy is complicated because it is difficult to differentiate the lesion from the classic variant or other lesions such as thyroiditis, and the definitive diagnosis is sometimes established with the surgical specimen.6
In the case described, the cytology result was Bethesda II on 2 occasions, with no diagnosis of thyroiditis or carcinoma. This established the surgical indication together with the high suspicion of malignancy on ultrasound, and the definitive diagnosis was reached based on the surgical specimen.
The histological diagnosis stands out because of a papillary structure with fibrovascular stalks infiltrated by lymphatic tissue and covered by tumor cells with oncocytic change and nuclear characteristics of papillary carcinoma. Oncocytic or Hürthle cells may be seen interspersed in the lymphatic infiltrate. The healthy parenchyma is also usually accompanied by lymphatic infiltrate.7
Proper diagnosis is important since the prognosis and treatment may be different for each histological variant. The differential diagnosis will be mainly with Hürthle cell carcinoma, as well as the tall cell and oncocytic variants of papillary carcinoma.7
The PTC-WL variant is associated with Hashimoto's thyroiditis in 80% of cases.2 Some authors consider this a good prognostic factor since the tumor is less aggressive and survival is higher when this association exists.8 In the case described, this association was found in the surgical specimen, but not in the preoperative cytological study.
The BRAF (proto-oncogene B-raf) V600E mutation presented by the patient has been implicated in the pathogenesis of papillary thyroid carcinoma,8 being detected in more than 80% of patients with the classic PTC variant2 and up to 65% of patients with the PTC-WL variant.2
Since there are few published cases, the prognosis and treatment are not clear. Based on the bibliography consulted, it appears to be a carcinoma with a good prognosis similar to the classic PTC variant, so the prognosis and treatment of the PTC-WL variant are currently considered the same. However, published studies include few cases, with short follow-up times and poorly documented histopathological and clinical characteristics.9
Regarding tumor behavior, the study by Yeo et al.2 is the only article that compares the PTC-WL and classic variants, finding that the former is associated more with Hashimoto's thyroiditis and less with the BRAF V600E mutation, with similar demographic, clinical and pathological characteristics, especially when associated with Hashimoto's thyroiditis.2
The BRAF V600E mutation has been associated with a worse prognosis, associated with more extensive disease and a higher recurrence rate.10 Therefore, we decided to use prophylactic central homolateral node dissection in the case described. However, Yeo et al. did not find a correlation between the BRAF mutation and the clinical–pathological characteristics among patients with the PTC-WL variant.2
The medical literature has reported lymphatic involvement in up to 45% of cases,2 3 cases of recurrence (1.8%)3,9 and 2 cases (1.2%) associated with undifferentiated areas, one of which progressed to anaplastic disease, distant metastasis and death within 18 months of surgery.3
The patient described presented an association with Hashimoto's thyroiditis and BRAF V600E mutation. After excellent response to treatment, she is currently disease-free.
Please cite this article as: Villalba Ferrer F, García Coret MJ, Ríos Agudo A, Alcalá García del Río G, Villalba Segarra A. Warthin-like, una variante infrecuente del carcinoma papilar de tiroides. Cir Esp. 2020;98:637–638.