Bilateral cerebral calcifications that affect the basal ganglia are detected in 0.68%–0.93% of cranial computed tomography (CT) scans.1,2 They have been reported in asymptomatic patients and in a variety of neurological conditions. Cerebral calcifications are classified into 3 groups: physiological, idiopathic (including Fahr disease) and secondary to calcium metabolism alterations.3 The most common causes of these calcifications with a striatum-pallidus-dentate distribution are the calcium–phosphorus metabolism disorders: hypoparathyroidism, pseudohypoparathyroidism, pseudo-pseudohypoparathyroidism and hyperparathyroidism. However, all chronic hypocalcaemia states, such as renal failure (the most frequent), vitamin D deficiency, hypomagnesaemia, pancreatitis and hypoparathyroidism, can be associated with intracranial calcifications.4 The association of basal ganglia calcifications and primary hyperparathyroidism is exceptional. We present a recent case and review data from the literature.
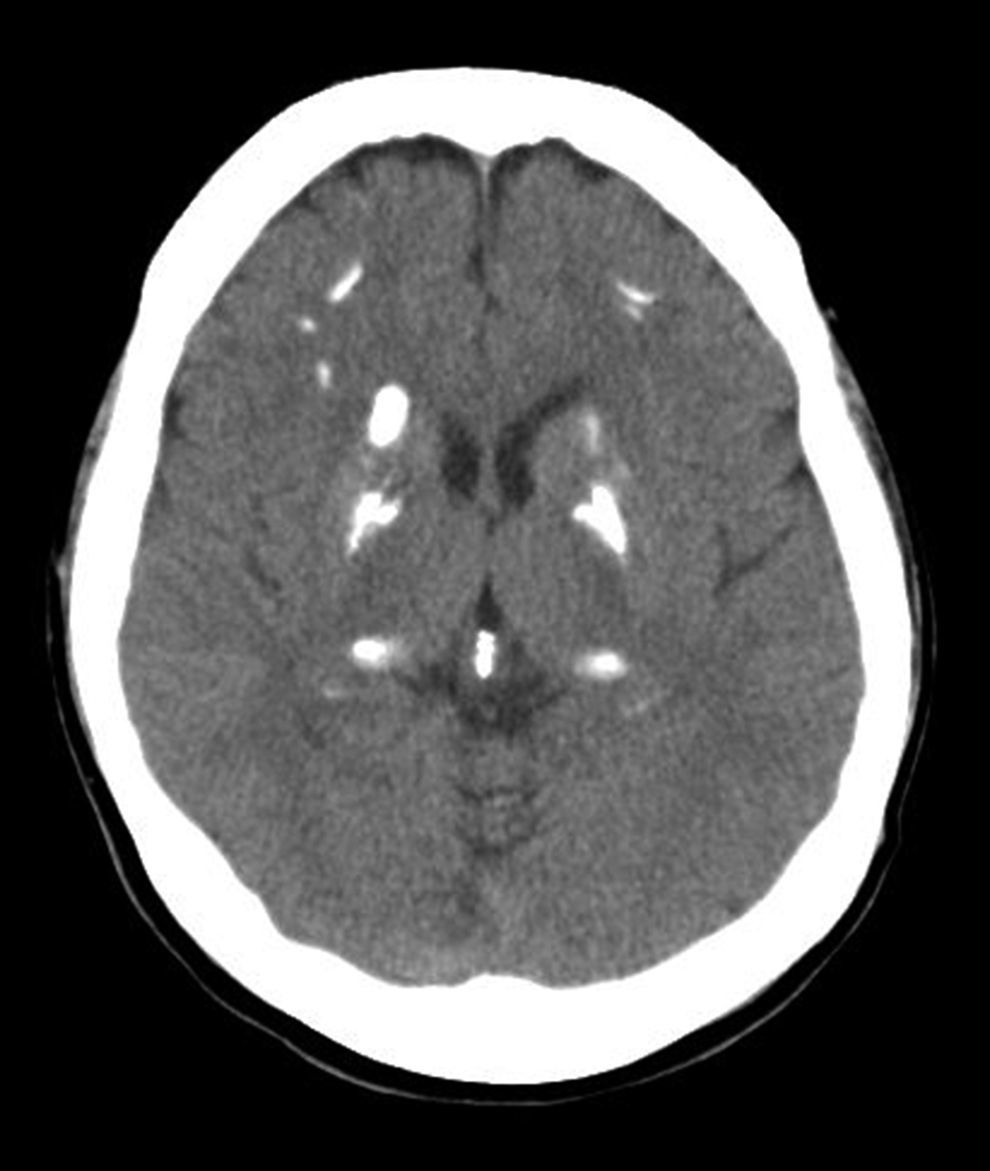
The patient is a 49-year-old woman who had been admitted due to an episode of partial left visual impairment and affected sensorimotor function of the left arm, of undetermined aetiology, which completely resolved spontaneously. She reported no medical history of interest, no family history of Fahr disease or Fahr syndrome, and no calcium–phosphorus metabolism diseases. She had had no previous fractures. Cranial CT study observed coarse calcifications in the basal and periventricular ganglia, as well as the bilateral frontal lobe and convexity (Fig. 1). The study was completed with a magnetic resonance imaging (MRI) scan of the brain, which revealed symmetrical calcifications in the basal ganglia, dentate nucleus of the cerebellum and in the union of the grey and white matter, which corresponded with the calcifications seen on CT scan.
The lab work showed: calcium 10.0mg/dL, phosphorus 2.8mg/dL, calcium×phosphorus product 28.0, total protein 65.4g/L, 24h calciuria 365mg/vol (normal: 110–250), PTH 172.7pg/mL (normal: 11–67), and calcifediol 11ng/mL. Other inflammatory, infectious and metabolic conditions were ruled out.
The images from the parathyroid scintigraphy and ultrasound were compatible with the presence of a left upper parathyroid adenoma. Bone densitometry showed the spinal column T-score of +0.46 and left hip T-score of −0.19. The diagnosis of primary hyperparathyroidism probably secondary to left upper adenoma was established. Even though it did not meet criteria of parathyroidectomy established in the Third and more recently the Fourth International Workshop on the Management of Asymptomatic Primary Hyperthyroidism,9,10 but given the possibility of progression of the cerebral calcium deposit, we opted for surgical intervention.
Nineteen months after the neurological episode, the patient underwent major ambulatory surgery involving minimally invasive parathyroidectomy with intraoperative monitoring, meeting the criteria for a biochemical cure. The pathology result was a 0.52g parathyroid adenoma. During follow-up, 4 months after the intervention, the patient has had no new neurological alterations, and the follow-up lab work showed calcium 9.0mg/dL, phosphorus 3.3mg/dL, calcium×phosphorus product 29.7, total protein 65.7g/L, albumin 38.7g/L, 24h calciuria 266mg/vol, PTH 28.9pg/mL and calcifediol 40ng/mL. The cerebral CT showed no changes compared to the original scan.
To determine the frequency of the association of primary hyperparathyroidism and cerebral calcifications, we performed a PubMed search without limits, last updated on 1 May 2015, and the following strategy: ([Cerebral Calcifications] OR [Brain Calcification] OR [Basal Ganglia Calcifications] OR [Central Nervous System Calcifications] OR [Intracranial Calcifications] AND [Hyperparathyroidism]). The search obtained 35 results. The articles and related bibliographic references were reviewed.
The possible causes of cerebral calcifications are metastatic deposits secondary to a local alteration of the blood–brain barrier or a neuronal calcium metabolism disorder.
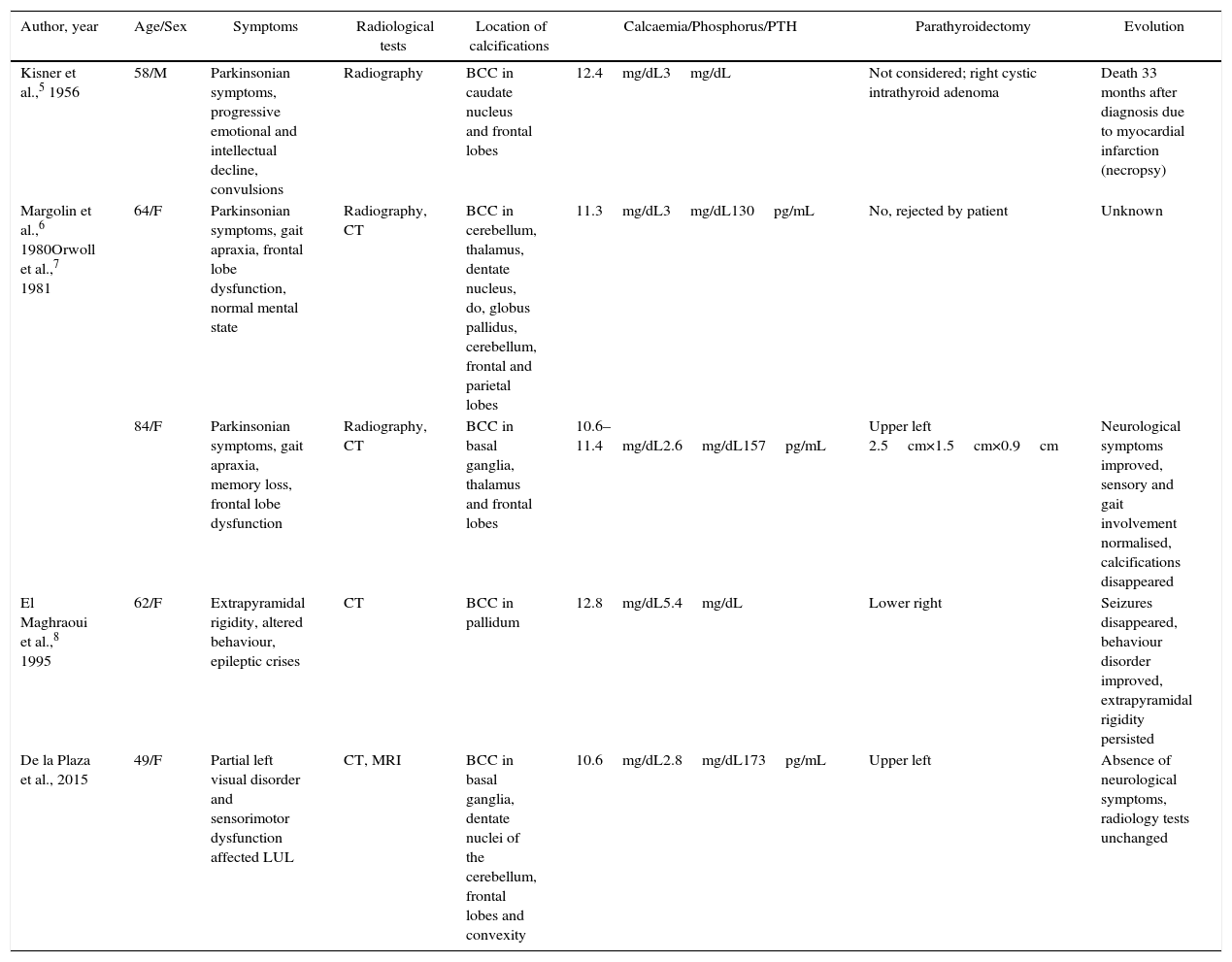
In the review of the literature, only 4 patients have been reported,5–8 2 of which were simultaneously included in 2 articles,6,7 who presented primary hyperparathyroidism and cerebral calcifications. The characteristics of the 4 patients described in the literature are summarised in Table 1.
Characteristics of the Patients With Bilateral Cerebral Calcifications and Primary Hyperparathyroidism.
| Author, year | Age/Sex | Symptoms | Radiological tests | Location of calcifications | Calcaemia/Phosphorus/PTH | Parathyroidectomy | Evolution |
|---|---|---|---|---|---|---|---|
| Kisner et al.,5 1956 | 58/M | Parkinsonian symptoms, progressive emotional and intellectual decline, convulsions | Radiography | BCC in caudate nucleus and frontal lobes | 12.4mg/dL3mg/dL | Not considered; right cystic intrathyroid adenoma | Death 33 months after diagnosis due to myocardial infarction (necropsy) |
| Margolin et al.,6 1980Orwoll et al.,7 1981 | 64/F | Parkinsonian symptoms, gait apraxia, frontal lobe dysfunction, normal mental state | Radiography, CT | BCC in cerebellum, thalamus, dentate nucleus, do, globus pallidus, cerebellum, frontal and parietal lobes | 11.3mg/dL3mg/dL130pg/mL | No, rejected by patient | Unknown |
| 84/F | Parkinsonian symptoms, gait apraxia, memory loss, frontal lobe dysfunction | Radiography, CT | BCC in basal ganglia, thalamus and frontal lobes | 10.6–11.4mg/dL2.6mg/dL157pg/mL | Upper left 2.5cm×1.5cm×0.9cm | Neurological symptoms improved, sensory and gait involvement normalised, calcifications disappeared | |
| El Maghraoui et al.,8 1995 | 62/F | Extrapyramidal rigidity, altered behaviour, epileptic crises | CT | BCC in pallidum | 12.8mg/dL5.4mg/dL | Lower right | Seizures disappeared, behaviour disorder improved, extrapyramidal rigidity persisted |
| De la Plaza et al., 2015 | 49/F | Partial left visual disorder and sensorimotor dysfunction affected LUL | CT, MRI | BCC in basal ganglia, dentate nuclei of the cerebellum, frontal lobes and convexity | 10.6mg/dL2.8mg/dL173pg/mL | Upper left | Absence of neurological symptoms, radiology tests unchanged |
BCC: bilateral cerebral calcifications; CT: computed tomography; F: female; LUL: left upper limb; PTH: parathyroid hormone; M: male; MRI: magnetic resonance imaging.
All the patients presented Parkinsonian symptoms and 2 of them had convulsive crises. It should be mentioned that 2 patients were not operated on. In the first case,5 surgery was not proposed to the patient, and the diagnosis of adenoma was established during necropsy. There was a progressive neurological decline until the patient died of a myocardial infarction 33 months after diagnosis. The evolution of the second patient, who rejected the procedure, is unknown.6
The other 2 patients who underwent parathyroidectomy experienced improved neurological syndrome, including the disappearance of seizures, the behaviour alteration in one of them,8 and sensory and gait alterations in the other. Calcifications practically disappeared from their CT scans.7 It should also be mentioned that the patient described in the article by El Maghraoui et al.8 with the diagnosis of parathyroid adenoma presented phosphates of 5.4mg/dL, which is hardly compatible with primary hyperparathyroidism.
The patient that we report in this article is the fifth case in the literature with associated bilateral basal ganglia calcifications and primary hyperparathyroidism. Although the coincidence of the different 2 entities cannot be ruled out, in the 2 previous cases published that had undergone resection of the adenoma, improvements were seen in the neurological symptoms in one and, in the other, the calcifications virtually disappeared. In our patient, 46 months after parathyroidectomy and 65 after the neurological symptoms and CT diagnosis, the basal ganglia calcifications have not progressed, nor have there been any further neurological symptoms. We do not know if the patient would have developed a more severe neurological condition if we had not performed parathyroidectomy, as was the case in the other 4 patients mentioned in our review. We therefore believe that parathyroidectomy is indicated in this association.
Please cite this article as: de la Plaza Llamas R, Ramia Ángel JM, Arteaga Peralta V, Hernández Cristóbal J, López Marcano AJ. Calcificaciones cerebrales e hiperparatiroidismo primario. Cir Esp. 2016;94:e5–e7.