Oesophageal cavernous hemangiomas are rare benign tumours, with less than 100 cases reported in the literature, that can simulate malignant tumours.
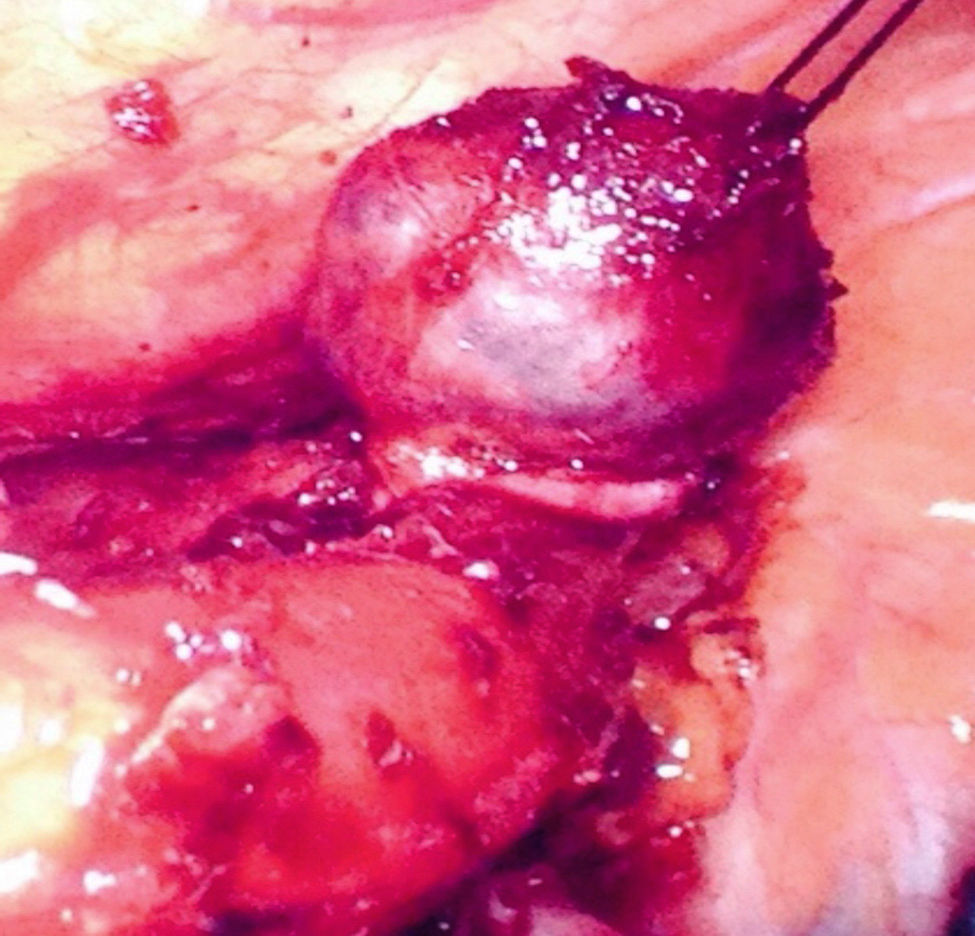
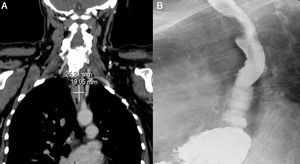
The patient is a 63-year-old woman with a history of right breast lumpectomy due to lobular carcinoma (stage T1N0) and selective biopsy of the sentinel lymph node in 2013. She came to our consultation because of grade I dysphagia to solid food that had been progressing over the past 24 months; in the last 2 months, she had also experienced grade III dysphagia to liquids associated with dysphonia for the previous 6 months. A computed tomography (CT) scan revealed a nodular image in the wall of the thoracic oesophagus measuring approximately 2.5×1.9cm (Fig. 1A). An upper gastrointestinal (GI) test identified a smooth repletion defect, compatible with a submucosal mass (Fig. 1B). The study was completed with endoscopic ultrasound, which demonstrated a tumour measuring 22×13mm that was 25cm from the dental arch, with heterogeneous echogenicity, cystic areas and perilesional lymphadenopathies measuring 7mm. The material obtained from the fine-needle aspiration (FNA) was bloody. Given the uncertainty of the exact nature of the lesion and its posterior evolution, we decided to perform surgery. Selective intubation was used of the left main bronchus and a right video-assisted thoracoscopic approach was used, with the patient in prone decubitus. Prior to selective lung collapse, 4 trocars were inserted in the right hemithorax: 2 12-mm and 2 5-mm subscapular trocars. Intraoperative endoscopy confirmed the location of the tumour 2cm proximal to the azygos vein, which was divided with a 30mm vascular stapler. The mediastinal pleura was opened longitudinally over the area of the tumour using an electrocautery hook, and the muscle layer of the oesophagus was likewise opened in the same direction. Afterwards, we carefully dissected the submucosal tumour that was adhered to the plane of the mucosa (probably due to fibrosis secondary to previous FNA), causing no perforation of the mucosa; finally, enucleation was completed (Fig. 2). The surgical specimen was inserted into a specimen bag and the myotomy was sutured to prevent mucosal prolapse. The trocars were closed and 2 20F chest tubes were inserted. Postoperative evolution was favourable, except for a hypertensive crisis that was difficult to control and fever that subsided after the withdrawal of the central catheter; these factors prolonged hospitalisation. A follow-up barium swallow revealed no fistula or stenosis, and the patient initiated tolerance to oral intake. She was discharged on the tenth day post-op. The pathology study with immunohistochemistry established the diagnosis of cavernous hemangioma (2.1cm) located in the submucosa that was circumscribed and pseudoencapsulated, integrating predominantly venous vascular elements and areas of capillary structures.
(A) Thoracic CT with i.v. contrast: submucosal stenosing oesophageal lesion measuring 2.5×1.9cm in craniocaudal length and 3.4cm cross-wise from the carina at its lower edge. (B) Barium oesophagogastric transit study: in the thoracic oesophagus, a smooth repletion defect is observed, compatible with submucosal mass.
Oesophageal cavernous hemangiomas originate in the oesophageal submucosa and protrude into the lumen, causing pseudopolyps. Their incidence is unknown, with few cases described in the literature. The most frequent symptoms are dysphagia and haemorrhage. Endoscopy can be diagnostic by detecting a blue-grey mass that is easily compressible, which should provide a suspected diagnosis of hemangioma and avoid biopsy, which is formally contraindicated. Endoscopic ultrasound provides visualisation of the lesion, determines its location, and can specify the vascular nature of the formation. CT with contrast also shows evidence of the lesion. Despite its benign nature, treatment is very important because fatal complications can develop, including severe haemorrhage.1 Endoscopy can be useful in small tumours; however, surgery is indicated in most cases.2
The first video-assisted thoracoscopic enucleations were published in 1992.3,4 Nonetheless, indications have not been established to suggest that oesophageal leiomyomas from 1 to 5cm in diameter would be the best candidates for thoracoscopy, with associated shorter hospital stays.5 In lesions of the lower third of the oesophagus, laparoscopic enucleation can be a valid option.6
The prone decubitus position improves continuous oxygenation for at least 12h after the intervention,7 as well as functional respiratory capacity and lung distensibility. Other advantages are the improved recovery of patients with acute respiratory failure, better diaphragm movement, and the prevention of pneumonia and dependent atelectasis in the left lung, which frequently occurs in the left decubitus position.8
The minimally invasive approach is a safe alternative to the open technique that presents less blood loss, shorter hospital stay, reduced total morbidity,9 less surgical trauma and a faster return to normal daily activities.10
With the case that we describe, we would like to highlight the feasibility of video-assisted thoracoscopic oesophageal extramucosal enucleation in prone decubitus.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Motos Micó JJ, Vidaña Márquez E, Belda Lozano R, Ferrer Márquez M, Rosado Cobián R. Exéresis toracoscópica en posición decúbito prono de un hemangioma esofágico. Cir Esp. 2016;94:e9–e11.