Takayasu arteritis (TA) is a granulomatous vasculitis that affects large arteries, primarily the aorta and supra-aortic trunks, although medium-sized arteries may also be involved.1
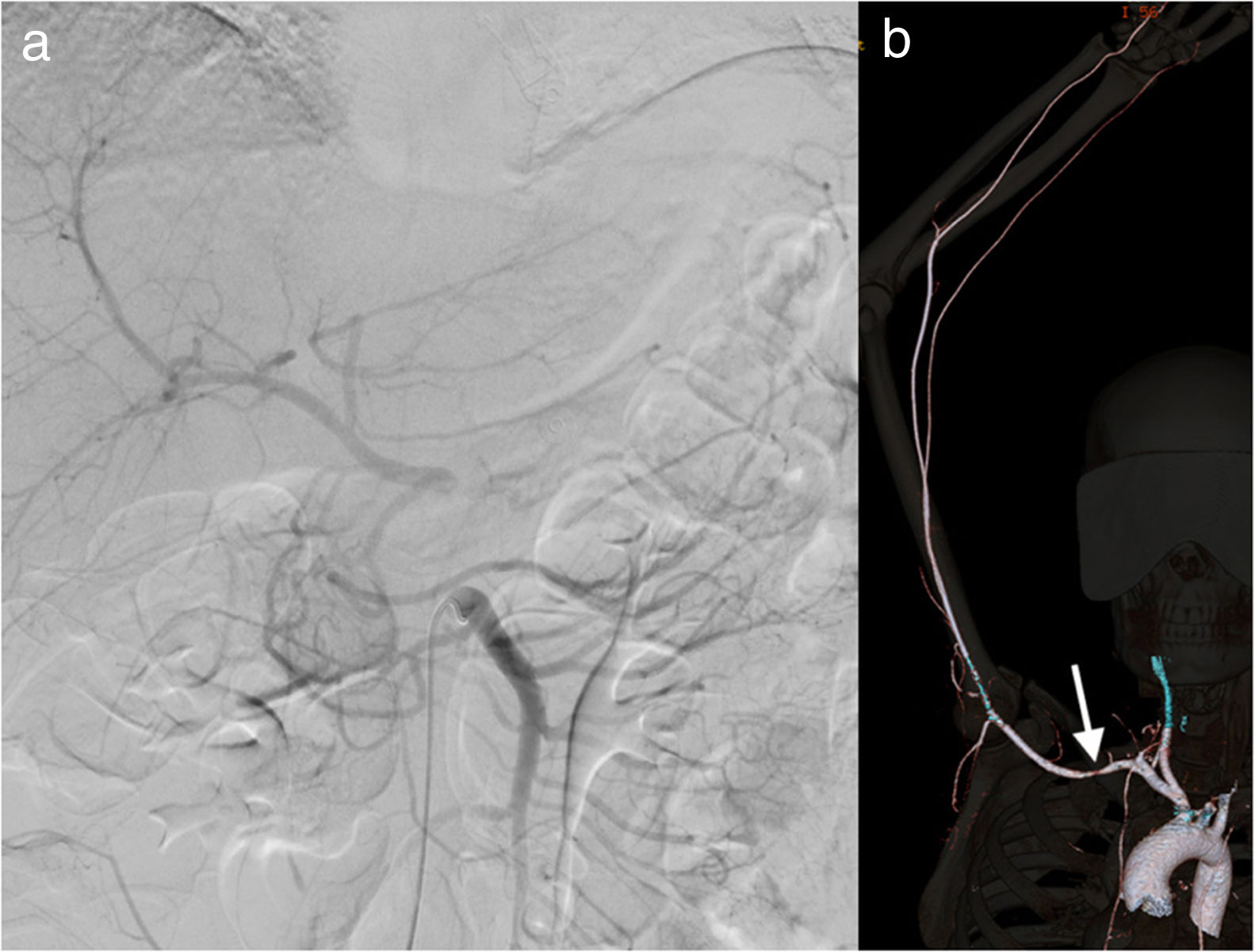
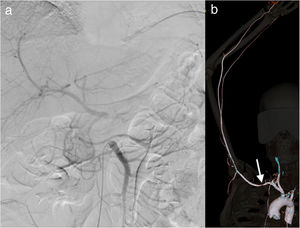
We present the case of a 35-year-old woman, with no family history of interest or known cardiovascular risk factors except obesity and oral contraception, who came to the emergency department due to exacerbation of postprandial epigastric abdominal pain that had been progressing for months. Lab work showed evidence of leukocytosis with neutrophilia, and abdominal ultrasound revealed no significant findings. The patient was hospitalized with suspected erosive gastropathy. Gastroscopy demonstrated changes in coloration of the gastric mucosa suggestive of ischemic disease. Subsequently, emergency abdominal CT scan identified complete thrombosis of the celiac trunk, hepatic hypoperfusion and splenic infarction. Diagnostic arteriography was performed and the findings were compatible with the CT scan (Fig. 1a). Due to the high risk of thrombus migration and signs of hypoperfusion of the abdominal organs, endovascular treatment was ruled out, and we opted to perform surgical treatment.
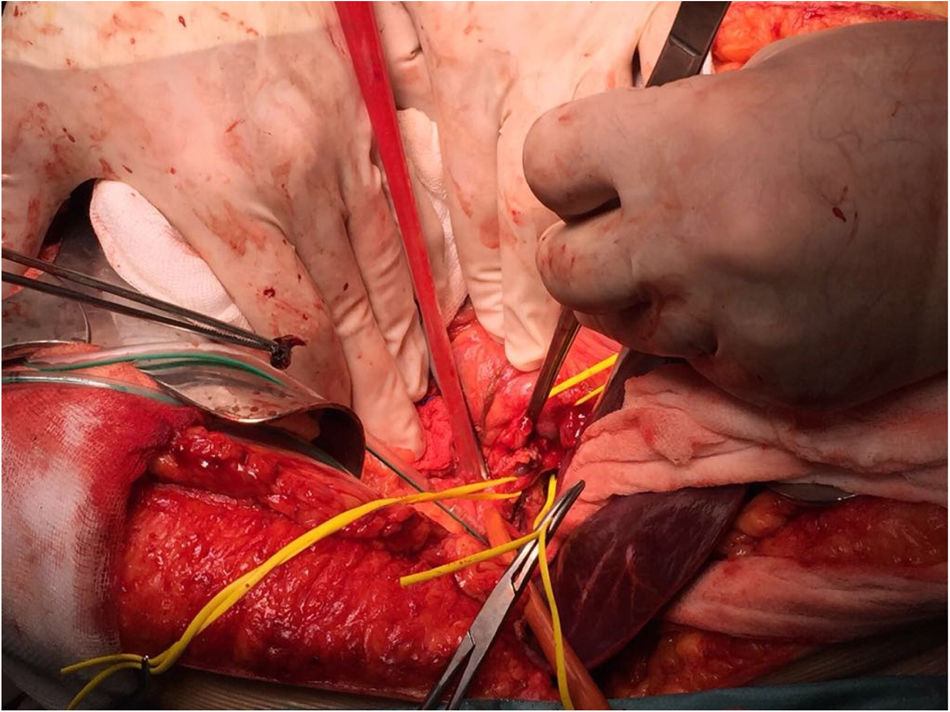
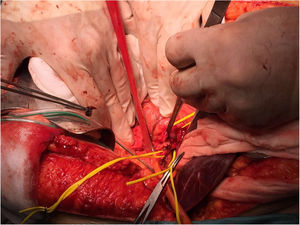
During emergency exploratory laparotomy, we observed generalized hepatic hypoperfusion and splenic infarction, with no other alterations. Thrombectomy was performed (Fig. 2), followed by angioplasty through the splenic artery to subsequently perform splenectomy. Hepatic reperfusion and restoration of flow to the celiac trunk were confirmed by intraoperative Doppler ultrasound.
On the second day of the postoperative period, a follow-up Doppler ultrasound was performed, which showed the absence of flow in the celiac trunk but no clinical repercussions. CT scan confirmed these findings but showed no alterations in the perfusion of the abdominal organs. On postoperative day 15, the patient was discharged from the hospital with home anticoagulation therapy using low molecular-weight heparin after hypercoagulability studies had shown no alterations.
One month later, the patient came to the emergency department for cyanosis of the fingertips of the right hand; corticosteroid and antihypertensive treatment were prescribed. After one month of treatment and persistence of pain along with claudication of the upper right limb, the patient was hospitalized. CT angiography of the aorta and supra-aortic trunks with 3D reconstruction showed wall thickening at the origin of the right subclavian causing a small stenosis in the segment between the clavicle and the first right rib (Fig. 1b).
Given the symptoms, claudication of the upper right limb, and the difference in systolic blood pressure between both arms greater than 10mmHg, the diagnosis of Takayasu disease was established. Treatment with prednisone and methotrexate was initiated, and the patient's progress was good.
TA is a chronic, idiopathic inflammatory disease that mainly affects women under the age of 40 and children. The annual incidence is estimated at 1.2–2.6 cases per million inhabitants per year in the western population, although it is much higher in Southeast Asia.1
Histopathology revealed adventitial thickening, areas of leukocyte infiltration of the tunica media and intimal hyperplasia. This response predisposes patients to the development of stenoses or arterial occlusion.2
The spectrum of presentation, severity and rate of progression of the disease can often lead to an inaccurate evaluation and a delay in diagnosis.3 Clinically, it presents with general symptoms and specific symptoms of vascular involvement (arterial hypertension, carotidynia and vascular murmurs)1 related to involvement of the celiac trunk in 18% of cases, according to the literature.3,4
The diagnostic criteria of the American College of Rheumatology are: age of onset before age 40, claudication of one of the extremities, decrease in the pulse of a brachial artery, difference in systolic blood pressure between both arms greater than 10mmHg, vascular murmur and alterations on imaging tests. Three of these 6 criteria are necessary to establish the diagnosis.5
In its treatment, corticosteroids, immunosuppressants, biological agents, antiplatelet/ anticoagulants or vasodilators can be used.1 The main surgical indications are renovascular hypertension, cerebrovascular diseases, coronary ischemia or vascular claudication.2
Chronic thrombosis of the celiac trunk may lead to different clinical manifestations, such as an ischemic syndrome of the celiac region, or it may remain asymptomatic due to the development of collateral circulation.6 In case of acute occlusion, ischemic necrosis will occur, which will affect to a greater extent those organs with terminal vascularization, such as the spleen in this case, an event described in the literature by Kelekis et al.,7 among others. Treatment involves revascularization, which can be either endovascular or by surgical bypass.6
Splenic infarction is a relatively uncommon diagnosis, and only 10% are diagnosed pre-mortem.8 The main causes include: thromboembolism, acute infection and hematological disease.9 There are hardly any cases associated with vasculitis, with a frequency of 2% in the O’Keefe et al. study, and no specifically described events due to TA in the literature.8,9 Genc et al. report a similar case of splenic infarction associated with thrombosis of the celiac trunk in a context of acute abdomen, although without being associated with vasculitis.10
In conclusion, despite the fact that the involvement of the celiac trunk in TA has been described in the literature,3,4 the case we present is an extremely rare event given its complete occlusion, causing splenic infarction.
FundingThis article has received no funding or grants from public, private or non-profit organizations.
Please cite this article as: García-Jiménez ML, Gómez-Pasantes D, Castro-Diez L, Rivas-Polo JI, Gómez-Gutiérrez M. Trombosis del tronco celíaco como presentación de la arteritis de Takayasu. Cir Esp. 2020;98:241–243.