Inflammatory pseudotumors (IPT) are rare benign lesions. Described by Brunn in the lungs in 1939,1 they are defined as masses comprised of a benign proliferation of inflammatory cells with a variable grade of fibrosis that can resemble malignant neoplasms. Their clinical presentation, laboratory data and radiological findings are variable, and differential diagnosis is difficult. Treatment is controversial, and may entail medical or surgical options.
IPT have the appearance of malignant tumors, but histologically they are benign. We present the case of a patient with a solid hepatic mass diagnosed as hepatic inflammatory pseudotumor, treated with long-term antibiotics that provided resolution of the symptoms. We will discuss the therapeutic management of this type of lesions and their differential diagnosis.
The patient is a 28-year-old male with a history of fever secondary to community-acquired pneumonia one year earlier. He came to our emergency room with symptoms of colicky abdominal pain in the right hypochondrium and fever of 38.5°C during the previous 2 days. Lab work demonstrated the presence of leukocytosis with hypertransaminasemia and total bilirubin of 3.3mg/dL. Serology for hydatidosis was negative, and tumor markers were within normal levels.
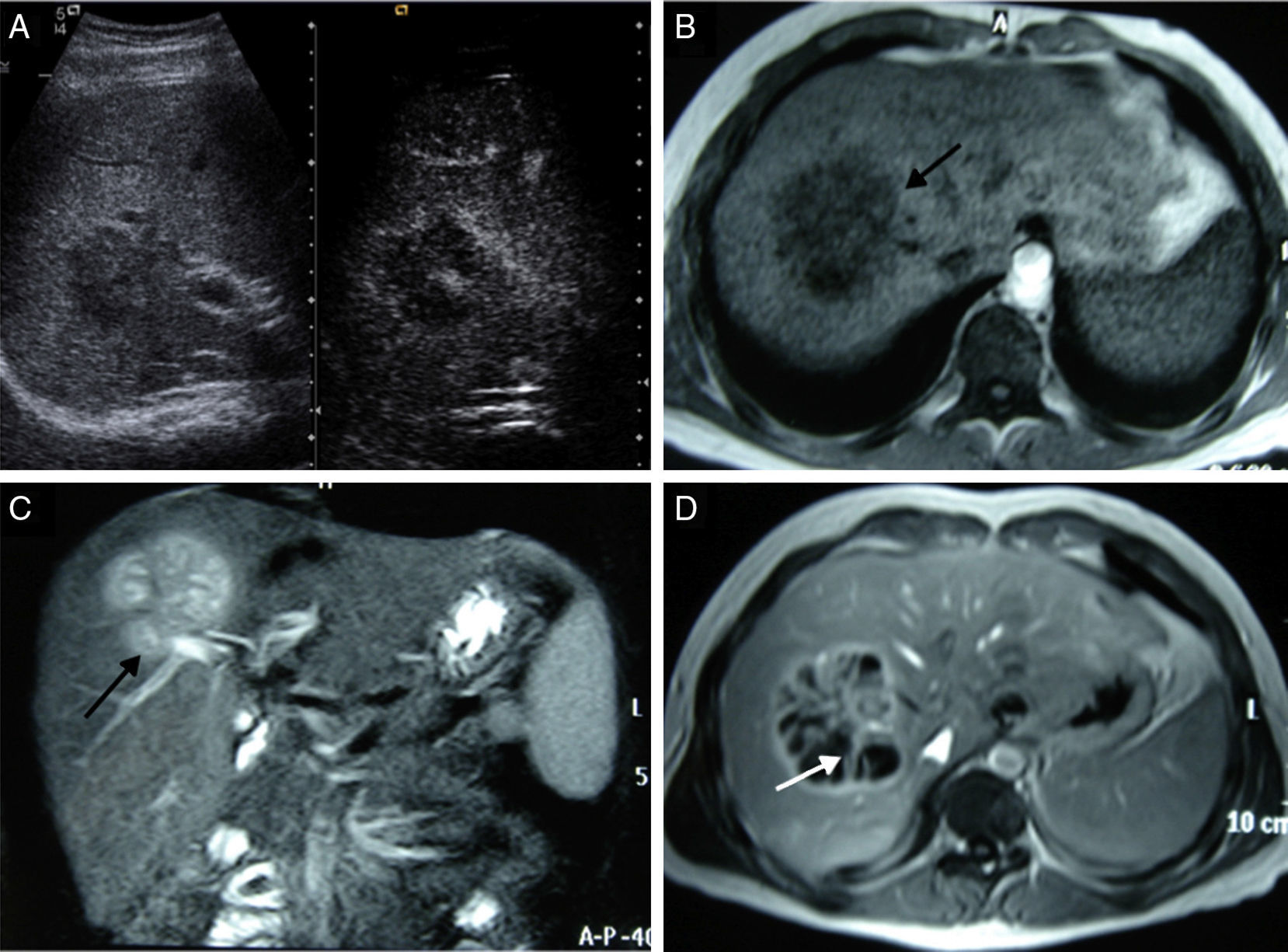
Ultrasound revealed the presence of a mass in the right hepatic lobe (RHL) that was hypoechoic with poorly defined edges and thin peripheral enhancement after the administration of contrast (Fig. 1). A magnetic resonance study with contrast revealed an 8cm focal lesion in the RHL (segments VII and VIII), which led to the differential diagnosis between hydatid cyst or a hepatic abscess in this clinical context (Fig. 1).
(A) B-mode ultrasound (left) shows a lesion with poorly defined edges and thin peripheral enhancement after the administration of contrast (right); (B–D) focal lesion in the RHL, hypointense in T1 (arrow in B) and hyperintense in T2 (arrow in C). The contrast study (D) shows peripheral uptake with irregular septa in its interior (arrow) in the portal phase.
Given the findings, antibiotic therapy was begun (amoxicillin/clavulanic acid 875/125mg every 12h) with anti-inflammatory treatment (dexketoprofen 25mg every 8h), and the patient was referred to our hospital. At that time, the follow-up lab work showed the disappearance of leukocytosis and normalization of transaminase and bilirubin levels.
Due to the absence of a conclusive radiological diagnosis despite the reduction of the lesion after antibiotic treatment, a liver biopsy was performed to rule out malignancy. The histological study showed dense fibrous-inflammatory tissue with plasma cellular and eosinophilic infiltration but no presence of necrosis or abscess, suggestive of inflammatory pseudotumor.
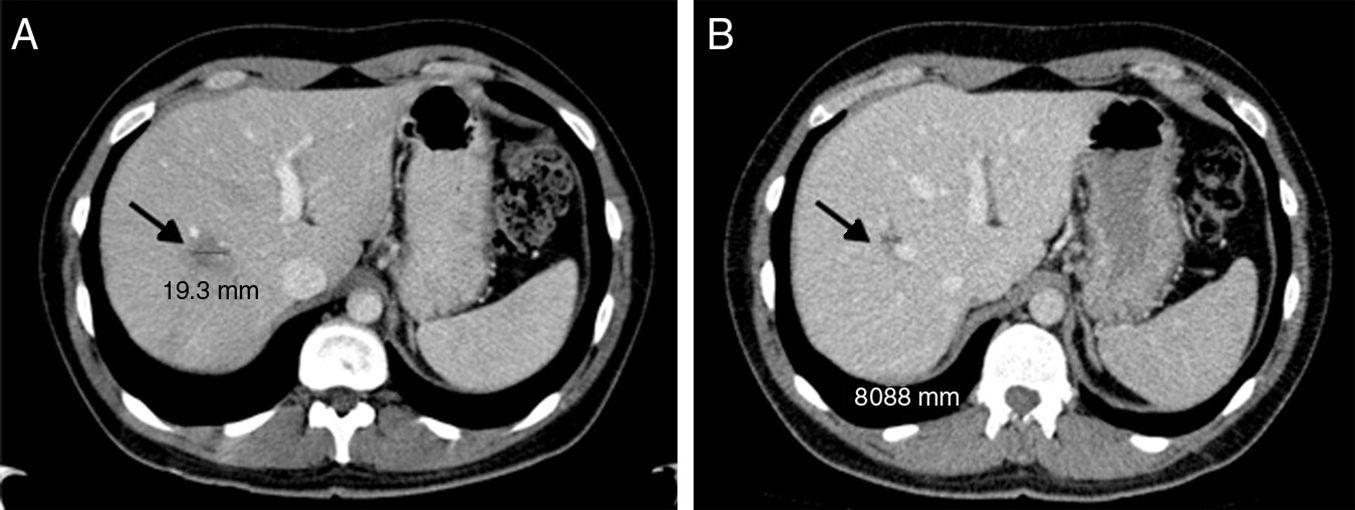
With the diagnosis of inflammatory pseudotumor, we continued to treat the patient conservatively. The patient was studied in the outpatient clinic, and the mass was observed to progressively reduce (Fig. 2) until its complete disappearance.
The most frequent location of inflammatory pseudotumors is the lungs, although there are also descriptions of IPT in the central nervous system, salivary glands, breast, liver, pancreas and spleen.
IPT most frequently affects young adults and males, with a mean age at appearance of 30 years. Its etiopathogenesis is unknown, although an autoimmune or infectious origin has been proposed,2 and there have been case reports with microorganisms involved (Escherichia coli and gram-positive bacteria).3
This entity has many forms of presentation, including altered general state, abdominal pain or fever, as in our patient. On other occasions, there is weight loss or diarrhea. On physical exploration, pain during palpation of the right hypochondrium and hepatomegaly may be present, although symptoms of cholestasis or liver failure are rare.
Laboratory findings can be within normal ranges, or alterations can be detected in inflammation or liver function parameters,4 as in our patient. Tumor marker levels are usually normal,5 while elevated CEA and CA 19-9 have been reported.6
From a radiological standpoint, the presence of a solid hepatic tumor with no specific criteria can make it suspicious of a neoplasm. Inflammatory pseudotumors usually present as well-defined lesions7 that can adopt different radiological patterns according to the evolution of the disease, quantity of fibrous stroma or inflammatory component,8 complicating the differential diagnosis with other lesions such as cholangiocarcinoma, hepatocarcinoma or liver metastases.9
Because of the uniformity of the clinical characteristics and complementary test results, this entity continues to be a current diagnostic challenge that should be contemplated in the differential diagnosis of hepatic lesions.
In our case, the suspicion of this pathology, based on symptoms, radiological images and the response to prescribed medical treatment, enabled us to make a preoperative diagnosis, thereby avoiding a surgical intervention.
The treatment of choice of inflammatory pseudotumors is medical, based on antibiotics, corticosteroids and anti-inflammatory drugs. Spontaneous remission has been described in some patients6 after progressive reduction in the size of the tumor in a variable time period that ranges from weeks to one year. However, the low incidence of IPT and the difficulties in diagnosis mean that most patients are diagnosed after surgical excision of the tumors because it is impossible to rule out malignancy preoperatively.
In our case, given the reduction in the size of the lesion in response to antibiotic treatment, we also considered the diagnostic possibility of hepatic inflammatory pseudotumor, and, because of the lack of a conclusive radiological diagnosis, a liver biopsy was conducted to rule out malignancy and to confirm our suspicion.
As it is a benign pathology, prognosis is excellent in most cases, and neighboring structures are rarely infiltrated.
Please cite this article as: Ballester-Pla N, García-Domínguez R, Pérez-Girbes A, Orbis-Castellanos JF, Pareja E. Tratamiento conservador en el seudotumor inflamatorio de origen hepático. Cir Esp. 2016;94:422–424.