Gastrointestinal stromal tumours (GIST) are the most common mesenchymal neoplasms of the digestive tract (3%). They are most frequently located in the stomach and small bowel, which are involved in 75% and 25% of cases, respectively.1 Oesophageal locations are rare (5%); the most common tumours in this region are leiomyomas, which represent 70% of benign oesophageal tumours. Given the clinical, endoscopic and radiological similarities between GIST and leiomyomas, they may not be properly differentiated until after resection. We present the case of an oesophageal leiomyoma that was treated as a GIST due to metabolic hyperactivity observed on PET/CT.
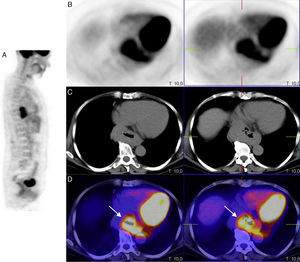
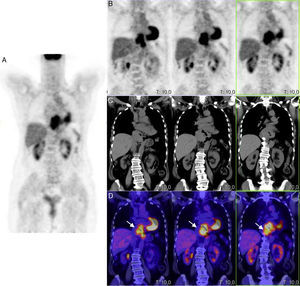
The patient is a 59-year-old woman with no medical history of interest, who reported epigastric discomfort that had progressed over the previous 5 years in association with a sensation of premature postprandial fullness in recent months. Upper gastrointestinal (UGI) endoscopy revealed, at the entrance to the gastric cavity, a large impression on the anterior lesser gastric curvature involving a lesion with bilobulated morphology that was submucosal in appearance. Endoscopic ultrasound (EUS) identified a mediastinal mass measuring 4×7cm, which was well-outlined and suggestive of benign disease, in contact with the left liver lobe, inferior vena cava and left atrium, with no signs of infiltration; the mass was slightly hypoechogenic compared to the liver parenchyma and well vascularised. The result of the EUS-guided fine-needle aspiration (FNA) was compatible with low-grade mesenchymal neoplasm (c-kit [−], actin ML [±], CD31 [−]). Computed tomography (CT) scan demonstrated a hypodense mass in the oesophagogastric junction (OGJ) measuring 9cm in length that caused circumferential wall thickening in its upper portion of up to 3.5cm, and somewhat more eccentric at its lower gastric portion, where it showed a clear submucosal component. With homogenous density and absence or very slight uptake of intravenous contrast, it was in contact with the posterior wall of both atriums, but with a defined interface. These findings were compatible with a submucosal tumour of the oesophagogastric junction, whose differential diagnosis included GIST, other mesenchymal tumours or adenocarcinoma. The study was completed with PET/CT, which demonstrated a hypermetabolic mass in the posterior mediastinum over the distal third of the oesophagus and extended towards the cardia, with a maximum SUV of 8.21 (Figs. 1 and 2).
PET/CT scan with FDG, in sagittal PET (A), axial PET (B), axial CT (C) projections and a superimposed PET-CT image (D) showing increased metabolic activity in the lower third of the oesophagus and in the oesophagogastric junction, with a notable increase in the thickness of the oesophageal and gastric wall.
Given the high diagnostic probability of c-kit (−) oesophageal GIST (some 5% do not express c-kit), due to the large tumour size, positive uptake in PET/CT and inconclusive FNA, we decided to perform oesophagectomy.
Midline laparotomy and a transhiatal approach revealed a large mass (10×8cm) in the distal oesophagus and OGJ that completely surrounded the oesophagus. The tumour was encapsulated, did not affect the serosa, and had several lobulations but no apparent lymph node involvement. Subtotal oesophagectomy was conducted with substitution gastroplasty and cervical oesophagogastric anastomosis.
The postoperative period ran its course without complications. Oral intake was properly re-established, and a follow-up transit study showed no pathological findings. The patient was discharged from hospital on the 7th day after surgery.
The pathology study confirmed a multinodular lesion in the distal oesophagus measuring 8.5cm×6cm×5.8cm, surrounded by a thin translucid capsule that was whitish-yellow in appearance, whirled, well-outlined and located at the transmural level, with no infiltration and free surgical margins. The microscopic analysis diagnosed an oesophageal leiomyoma with the following immunochemistry profile: desmin (+), total actin (+), actin ML (+), c-kit (−), myoglobin (−), vimentin (−), CK (−), CD34 (−), S100 (−) and Ki-67 (less than 0.5%).
In order to establish the differential diagnosis between GIST and leiomyoma, different diagnostic tools can be used, such as EUS, CT, MRI, etc. Recently, several authors have considered that PET/CT could play an important role in this dilemma, as leiomyomas, unlike GIST, do not usually have an affinity with 18-fluorodeoxyglucose.2 Nevertheless, as occurred in our case, PET is not infallible and has false positive results, especially when the accumulation of 18F-FDG is an incidental finding. In fact, the accumulation of 18F-FDG in the distal oesophagus is not uncommon. It can be seen in benign inflammatory lesions, such as gastroesophageal reflux, Barrett's oesophagus, glycogenic acanthosis and infections.3 Only 8.3% of reports are of malignant processes in incidental findings of increased uptake of 18F-FDG in the oesophagus.4 Leiomyomas with intense uptake can be confused with malignant lesions.
It has traditionally been suggested that, in well-outlined submucosal tumours of the oesophagus, preoperative biopsies should not be done due to the risk for increasing the rupture of the mucosa during enucleation. However, due to the increased experience with EUS+FNA, many hospitals are now using this technique. Nevertheless, today, in spite of the advances made in diagnostics, the histology study of the surgical specimen is still what provides the definitive diagnosis of GIST versus leiomyoma. Typically, leiomyomas are positive for desmin and actin, and negative for CD34 and CD117, which is the opposite of what happens in GIST.5
With this case report, we would like to emphasise the need to keep advancing in the preoperative differential diagnosis for these tumours, due to the radically different approach that they require. The treatment of choice of oesophageal leiomyomas is enucleation, which is unlike GIST, where treatment is based on complete tumour resection (R0) with histologically negative margins.6 In the oesophagus, this usually involves oesophagectomy, except in tumours smaller than 2cm, in which case enucleation, endoscopic resection or follow-up without surgery are acceptable, as the potential for metastatic spread is almost null.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Álvarez Martín MJ, Garcia Navarro AM, Rodriguez Fernandez A, Jimenez Rios JA. Leiomioma de esófago con intensa captación de 18fluorodeoxiglucosa en la tomografía por emisión de positrones-tomografía computarizada. Cir Esp. 2016;94:419–422.